Neck Trauma
advertisement
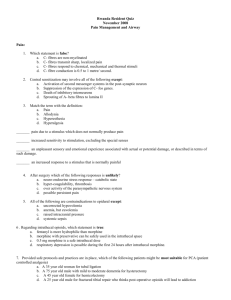
Prepared by Dr.Hiwa As’ad As the incidence of violence rises in the society the rate of penetrating head &neck trauma also increase 5-10 % of all trauma cases potentially dangerous & require emergency treatment There are four groups of vital structures which are vulnerable to injury in a small anatomical area & are not protected by bone: 1-Air passages including (Pharynx, Larynx, trachea & lungs) 2-Vascular ( Carotid ,Jugular, Subclavian, Innomenate, Aortic arches) 3-Gastrointestinal tract ( Pharynx, esophagus) 4-Neurologic structures (Spinal cord ,brachial plexus ,cranial nerve ,peripheral nerve) Air way 1-Strider 2-Cyanosis 3-Respiratory distress 4-Hemoptysis 5-Hoarsness 6-Tracheal deviation 7-Surgical emphysema 8-Sucking wounds Vascular system 1-Hematoma 2-Persistant bleeding 3-Neurologic deficit 4-Absent pulse 5-Hypovolemic shock 6-Thril 7-Bruit 8-Change of sensorium Neurologic 1-Hemiplegia 2-Quadreplegia 3-Coma 4-Crainal nerve deficit 5-Change of sensorium Esophagus & Hypo-pharynx 1- Dysphagia 2-Odenophagia 3-Subcunatous emphysema 4-Hematamesis 5-Hemoptysis 6-Tachycardia 7-Fever The most important is the initial evaluation and resuscitation performed in the emergency department. The protocol is based on a primary and secondary survey approach This treatment can be divided into four categories—primary survey, resuscitation, secondary survey, and definitive care. 1-Airway Establishment of the airway. The oropharynx, larynx, and trachea can be obstructed by secretions, blood, and foreign bodies. Collapse of the oropharyngeal airway can occur with loss of consciousness and from facial fractures. Direct trauma to the larynx and trachea may cause airway obstruction below the oropharynx. Maneuvers range from positioning,manual cleaning of the oropharynx followed by suctioning of secretions to surgical procedures. There is risk of an occult cervical spinal fracture. The airway must be controlled with the assumption that such a fracture exists and the neck must be completely immobilized in a neutral position. Maintain manual stabilization of the head and avoid hyperextension by holding the cervical spine with the hands while immobilizing the head with the forearms Traction on the head is avoided, because distraction with further injury to the spinal cord can occur if the patient has an unstable cervical spinal injury. Once the neck of an unconscious patient has been secured, forward traction of the mandible is performed to overcome pharyngeal collapse Once the airway has been established and the patient is spontaneously breathing, supplemental oxygen can be provided through nasal prongs or a face mask. In sever cases more aggressive airway management is needed: 1.Nasotracheal intubation for establishing an airway in a conscious patient who may have a cervical spinal injury because it can be done without excessive mobility of the neck and is better tolerated by an awake patient than is orotracheal intubation 2.orotracheal intubation: In ideal circumstances, a lateral cervical spine radiograph is obtained before orotracheal intubation to evaluate for a possible cervical spinal fracture. Bag-mask intubation can be an effective method of maintaining the airway until radiographs are obtained. If the patient is unconscious and cervical spinal injury has been ruled out, orotracheal intubation can be readily accomplished. A patient who is awake must be paralyzed with succinylcholine for successful orotracheal intubation. After intubation, the chest is auscultated to ensure that the tube is in the trachea and not in the esophagus or in one of the mainstem bronchi. If an endotracheal tube cannot be inserted, as when a patient has major facial fractures or has sustained laryngotracheal trauma, surgical airway intervention may be needed. There are four surgical methods of obtaining an airway 1-Needle cricothyrotomy, 2-Conventional cricothyrotomy, 3-Tracheotomy, and 4-Percutaneous transtracheal ventilation. For children is the best procedure. performed by placing a no. 12 or no. 14 intravenous cannula with a plastic sheath through the crico-thyroid membrane into the tracheal lumen. Once in the airway, the needle is withdrawn and the plastic sheath is advanced. When properly positioned, the sheath is connected to bottled oxygen. Patients can be maintained for up to 30 minutes with this technique. The preferred approach for adult patients. It consists of a small vertical skin incision over the area of the cricothyroid membrane followed by a horizontal incision through the cricothyroid membrane itself. The blunt end of the scalpel is inserted between the cricoid and the thyroid cartilages and rotated 90 degrees to make an opening through which an endotracheal tube or tracheostomy tube can be inserted. For patients with laryngeal trauma, tracheal trauma, or tracheal disruption, cricothyrotomy is inadvisable, and emergency tracheotomy is performed. Percutaneous transtracheal ventilation, a technique similar to needle cricothyrotomy, is an acceptable alternative in the treatment of these patients. Continuous monitoring of oxygenation with pulse oximetry is extremely helpful in determining the adequacy of oxygenation of a trauma patient and is used in the care of all critically injured patients to allow early detection of arterial oxygen desaturation. The secondary survey consists of a detailed physical examination with the patient fully exposed (from head to toe). It is undertaken once the lifesaving priorities of the primary survey have been done. The breadth and speed of this examination depend on the patient's injuries and the need for definitive surgical intervention. history: including the mechanism of injury, preexisting medical problems, current medications, known drug allergies, and when the patient last ate. Routine investigations: including a complete blood cell count, chest radiography, and urinalysis. If drug overdose or alcohol consumption is suspected, toxicological studies can be performed. Hypotension warrants blood typing and cross-matching. X-rays required after secondary survey are now completed Special investigations such as Angiography ,CT scan, US, gastrograffin /Barium studies may now be performed in hemodynamically stable pt. Penetrating injury 1-Stabs 2-Gun shot wounds *Low velocity *High velocity *Shotgun Blast Blunt • If platysma muscle is penetrated or not . • Although overall uncommon, Pharyngoesophageal injury is the most commonly missed injury to the neck Some authors advocate routine exploration of all injuries penetrating the platysma. Others advocate observation and selective exploration based on preoperative arteriographic findings and on the presence or absence of symptoms that suggest vascular, airway, and neurologic injury. Zone I: sternal notch to cricoid cartilage Zone II: cricoid cartilage to angle of mandible Zone III: angle of mandible to base of skull Patients in unstable condition with active hemorrhage need surgical exploration. If the patient is stable: Penetrating injuries to (zone I) ; are examined by arteriography, laryngoscopy, and esophagoscopy or a barium swallow . Penetrating injuries to(zone III) are examined with arteriography to exclude carotid or vertebral artery injury. Penetrating injuries to (zone II) are examined by routine exploration or combinations of arteriography, laryngoscopy, and esophageal evaluation if the injury has penetrated the platysma. • High risk of injury to great vessels, trachea ,esophagus and lungs • Difficult region for exposure and control • Management: arteriography of arch, great vessels, carotids, and vertebral (may also be used for balloon occlusion for temporary preoperative control); Esophagogram with esophagoscopy, direct laryngoscopy, and bronchoscopy • High risk of injury to carotid sheath (carotid artery, internal jugular vein) and aerodigestive system. • More easily accessible and more easy to control • Management 1.Selective Management: arteriography, esophagram with esophagoscopy, direct laryngoscopy, and bronchoscopy 2.Mandatory Surgical Exploration: gunshot wounds that cross midline, obvious serious injury (strider, active hemorrhage, absent carotid pulse), active bleeding, air bubbling through wound, arteriography not available, intoxicated patient 3.Elective Surgical Exploration: more accurate than diagnostic tests, up to 50–70% of elective neck explorations are negative • High risk of injury to distal carotid artery, parotid gland, and pharynx • Difficult region for exposure and control • Management: arteriography (balloon occlusion), Esophagram and direct laryngoscopy Pharyngeal injuries Suspected in zone II penetrating injury if the pt has dysphagia, odynophagia, subcutaneous emphysema ,hemoptysis, & hoarseness. Diagnosis: 1-Flexible nasopharyngoscopy: edema ,bleeding or perforation 2-Direct phayngscopy: reveals all injuries. 3-Esophagography: unreliable tool Treatment 1- Naso & oro pharynx managed conservatively as it’s capacious & has low intra-luminal pressure 2-Hypopharynx managed like esophageal injury by exploration for it’s high intra-luminal pressure & less capacious Suspected in pt with Zone I & II injuries with hoarseness, neck pain, and crepitus. Fiberoptic examination and C/T scans are extremely helpful. 1-Fiberoptic Nasopharyngoscopy It is well-tolerated in a patient who is awake and is a quick diagnostic test The larynx is evaluated for vocal cord mobility, arytenoids symmetry and extent of the injury from minor edema or hematoma to more severe soft-tissue tears and exposed cartilage. 2-Conventional X-Rays and Soft-Tissue Films Plain-film x-rays of the chest and soft-tissue neck films continue to be essential components in patient evaluation. The best radiographic tool available to evaluate laryngeal trauma . Helpful when the examination is normal but there is a high index of suspicion for occult laryngeal injury where It may reveal a subtle fracture that requires fixation or it may obviate the need for rigid endoscopy if the scanned image is completely normal. To plan the operative procedure in a patient with a controlled and stable airway. Laryngeal injuries are grouped according to increasing severity: 1- Patients with Group I injuries have minor endolaryngeal hematomas or lacerations. These patients are treated conservatively 2- Group II injuries demonstrate airway compromise, more severe soft tissue injury, or single nondisplaced laryngeal fractures. These patients are usually managed with a tracheotomy followed by direct laryngoscopy If an arytenoid dislocation is discovered, then closed reduction should be attempted. 3-Group III injuries include patients with massive edema, mucosal tears with exposed cartilage, displaced fractures, or vocal cord immobility. 4-Group IV describes the unstable larynx with comminuted fractures. 5-Group V classification is the most severe type of injury; these patients present with complete laryngotracheal separation. Injuries within Groups III–V require immediate operative repair. The ability to restore the integrity of the larynx impacts a patient's long-term outcome with regard to voice, airway, and the quality of life. The common carotid artery is the most frequently injured accounting for 22%of vascular injuries hard signs includes ,hematoma persistent bleeding ,neurologic deficit absent pulse ,thrill & bruit. Investigation for Zone I & III is recommended because of difficult assessment clinically but Zone II clinical assessment is reliable Diagnostic tools Angiograghy Is gold standard & has the following benefit Identification of the site of injury Detection of subclinical vascular injury Providing a road map for surgeon Giving idea about the circle of Willis Treatment Vascular surgical intervention (Repair or Ligation) External jugular vein can be safely ligated Unilaterally internal jugular vein can be ligated Bilateral internal jugular vein injury: Repair (loss of consciousness, increase intracranial pressure &even death might occur after bilateral ligation). brachial plexus injury : repaired electively within 24-72 hours unless the neck explored for other reasons.