physiology_lec20_13_3_2011
advertisement
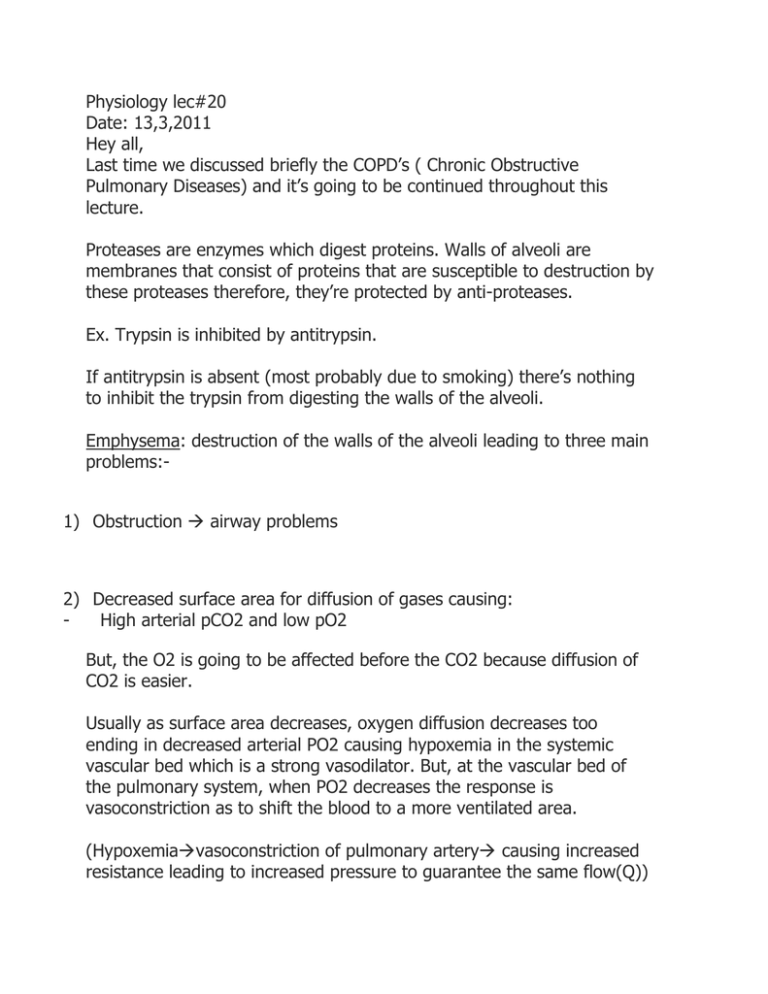
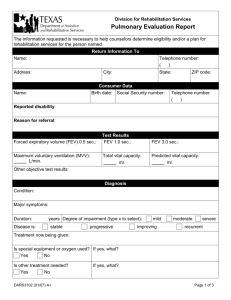
Physiology lec#20 Date: 13,3,2011 Hey all, Last time we discussed briefly the COPD’s ( Chronic Obstructive Pulmonary Diseases) and it’s going to be continued throughout this lecture. Proteases are enzymes which digest proteins. Walls of alveoli are membranes that consist of proteins that are susceptible to destruction by these proteases therefore, they’re protected by anti-proteases. Ex. Trypsin is inhibited by antitrypsin. If antitrypsin is absent (most probably due to smoking) there’s nothing to inhibit the trypsin from digesting the walls of the alveoli. Emphysema: destruction of the walls of the alveoli leading to three main problems:1) Obstruction airway problems 2) Decreased surface area for diffusion of gases causing: High arterial pCO2 and low pO2 But, the O2 is going to be affected before the CO2 because diffusion of CO2 is easier. Usually as surface area decreases, oxygen diffusion decreases too ending in decreased arterial PO2 causing hypoxemia in the systemic vascular bed which is a strong vasodilator. But, at the vascular bed of the pulmonary system, when PO2 decreases the response is vasoconstriction as to shift the blood to a more ventilated area. (Hypoxemiavasoconstriction of pulmonary artery causing increased resistance leading to increased pressure to guarantee the same flow(Q)) 3) Vascular problem which is manifested by destruction and decrease of the capillary beds causing:[Q= P/R(pulmonary vascular resistance)] - decreased surface area increased resistance As a result, P in the pulmonary arteries has to increase by the same proportion as resistance to keep Q constant . But, this will cause the right ventricle to increase the force of contraction to overcome the high pressure and cause:1) Dilatation 2) Failure As a conclusion, smoking clearly leads to emphysema and therefore right heart failure. NOTE: Emphysema increases vascular resistance due to: 1) Hypoxemia 2) Destruction of the capillary bed Both reasons increased the load on the heart causing a condition called Cor pulmonale which is right heart dilatation and sometimes failure due to lung disease that either increases pulmonary vascular resistance or decreases PO2. NOTE: Destruction of the alveolar wall (Emphysema) is irreversible in smoking since some alveolar cells can’t repair themselves. People who live in high altitude areas where there is a decrease in PO2 It means they have hypoxia due to decreased arterial O2 ,but for a long time with more decrease of O2 this will lead to Cor pulmonale. Another COPD is [Chronic Bronchitis] -Too much mucus secreted from bronchioles which is an ideal medium for the growth of bacteria causing continuous infection - Epithelium becomes very thick - Obstruction -Productive cough (cough with mucus) So, if a smoker starts coughing every single day for three months in the winter time for two successive years this is chronic bronchitis and is irreversible. Anyone is able to make this diagnosis based on the previous information. Any patient with Emphysema has some aspects of Chronic bronchitis and vice versa. Both these COPD’s are mainly caused by alpha 1 deficiency that is acquired for example due to smoking and is very rare at birth. Bronchial Asthma a) Extrinsic asthma gotten from outside the body. b) Intrinsic asthma gotten from inside the body. Both these types are induced by physical exercise. What happens is:An inhaled irritant causes bronchoconstriction (contraction of the muscles of the bronchus) followed by mucus secretion from goblet cells. The water in the mucus is reabsorbed forming a solid and causing an asthma attack. The first line of treatment is a bronchodilator which uses beta 2 sympathetic agonist specific for the lungs or adrenaline for emergencies which is given subcutaneously and causing bronchodilatation. OR -mucolytic degrades mucus -antiinflammatory (cortisol which is an inhaler that decreases swelling) -antibiotic to kill the bacteria in the mucus NOTE: never give a cough suppressant [Back to emphysema] When the walls of the alveoli were destructed the elastic fibres were also destroyed which means active expiration. This is going to decrease the collapsing tendency of the lung meanwhile the expanding tendency of the thorax remains the same so the system is not at equilibrium. The solution would be to increase the FRC increasing the collapsing tendency of the lung and decreasing expanding tendency of the thorax reaching a new equilibrium point where the collapsing tendency is equal to the expanding tendency. [Testing for emphysema during expiration] The first quarter of air is expired quickly, the middle 50 percent is moderately quick and the last quarter is expired at a slower pace. 1) Fill the lungs to full capacity 2) Expire the Forced Vital Capacity (FVC) which is quick exhalation 3) Within 4 seconds for normal people the vital capacity is exhaled. But for a person with an obstruction it takes more time. 4) We check the Forced expiratory volume(FEV) ( volume expired in 1 second) 5) Ex. Normal FEV/FVC= 4/5*100 % 80% Abnormal FEV/FVC=3.5/5*100% 70% The problem with this method is that it doesn’t really indicate the extent of the obstruction therefore, the first and last quarters are going to be deleted since they dilute the result. This is called the MMEF( Mid Mean Expiratory Flow) Ex. Normal 3.5/1*100% Abnormal 1.5/1*100% We can now say that more than 50% of the lung is destroyed making the MMEF a more sensitive test. Your colleague: Hala Salamin Hope I conveyed the message =) Good luck all!