Preparing for an Unplanned Radiation Event
advertisement

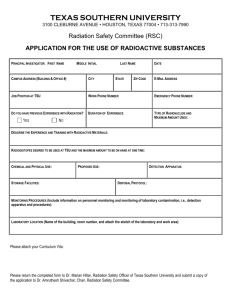
Preparing for an Unplanned Radiation Event Niel Wald, M.D. Michael P. Kuniak, D.O., M.P.H. Acknowledgments Prepared by the Radiological Emergency Medical Preparedness & Management Subcommittee of the National Health Physics Society Ad Hoc Committee on Homeland Security. Jerrold T. Bushberg, PhD, Chair Kenneth L. Miller, MS Marcia Hartman, MS Robert Derlet, MD Victoria Ritter, RN, MBA Edwin M. Leidholdt, Jr., PhD Consultants Fred A. Mettler, Jr., MD Niel Wald, MD William E. Dickerson, MD Appreciation to Linda Kroger, MS who assisted in this effort. Christine Hartmann Siantar, Ph.D. Deputy Program Leader Nuclear and Radiological Countermeasures Monterey Institute of International Studies Center for Nonproliferation Studies Resource Links CIF 2004-2005 (http://cif.miis.edu/resource.htm) Associate Professor UC Davis OUTLINE Radiation Terrorism and Response 1. Radiation Basics 2. Radiation Protection Rules 3. Radiation Threats Nuclear device, “dirty” bomb Equivalent Experiences: Chernobyl, Goiana 4. Health Management of Affected Population What is Radiation? • For the purpose of this presentation, defined as energetic emissions from unstable atoms that can result in ionizing events to target atoms • Ionizing radiation is radiation capable of imparting its energy to the body and causing chemical changes • Ionizing radiation is emitted by – - Radioactive material – Some devices such as x-ray machines • Common Radiation Terms • Radioisotope - a generic name for a radioactive element • Radionuclide - a specific radioisotope such as Uranium-235 • These terms are often used interchangeably Radiation Physics • Ionizing Radiation – Radiation with enough energy to cause ionization of atoms by ejecting electrons from their atomic orbits • Types of Radiation – Electromagnetic (Photons - No Mass) • X-ray, Gamma – Particulate • Alpha (helium nucleus), Beta (electron), Proton, Neutron Types of Radiation Emitted from Radioactive Material • Particulate – Charged • Alpha Radiation • Beta Radiation – Uncharged • Neutron Radiation • Electromagnetic • Gamma Radiation Types of Ionizing Radiation Alpha Particles Stopped by a sheet of paper Radiation Source Beta Particles Stopped by a layer of clothing or less than an inch of a substance (e.g. plastic) Gamma Rays Stopped by inches to feet of concrete or less than an inch of lead Alpha and Beta Radiation • Alpha – Typically emitted from a heavy element – Most have energies between 4-8 MeV – Particles up to 7.5 MeV stopped by dead skin layer (only a few microns penetration) – Can be shielded by paper – Penetrates a few cm in air – Does not penetrate the dead layer of skin • Beta – Travels about 4 meters in air per MeV – Penetrates about 0.5 cm in soft tissue per MeV – Can reach the basal cell layer of skin Pertinent Alpha Emitters Neutron Radiation • Neutral particle emitted from the nucleus • Can be very penetrating • Requires special consideration for shielding • Can induce radioactivity when absorbed by stable elements (N, Na, Al, S, Cl, P, etc.) Electromagnetic Radiation • Energy = hf • Energy expressed typically in KeV or MeV (not joules) • Absorption of Electromagnetic Radiation by matter – Photoelectric – Compton Scattering – Pair production (photon energy must exceed 1.02 MeV) • Stochastic event • Low energy photons more readily absorbed The Electromagnetic Spectrum Gamma Radiation • Electromagnetic energy emitted from the nucleus • Specific energies can be analyzed to identify source • Very penetrating (many meters in air) • Difficult to shield, often shielded with lead X-ray Radiation • Electromagnetic energy emitted from outside the nucleus • May be “machine-produced” by bombarding high energy electrons on a target • May also be emitted from radioactive materials • Similar shielding and penetrating powers as gamma radiation Radiation Units Measure of Quantity Unit Amount of radioactive material Activity curie (Ci) Ionization in air Exposure roentgen (R) Absorbed energy per mass Absorbed Dose rad Absorbed dose Dose weighted by type Equivalent of radiation For most types of radiation rem 1 R 1 rad 1 rem Units of Radioactivity • Quantity – 1 Becquerel (Bq) = 1tps – 1 Curie (Ci) = 3.7 x 1010 tps • Exposure – 1 Roentgen (R) = 2.58 x 10-4 C/Kgair 87.7 ergs/gair • Exposure to Dose Relationship – 1 R exposure 95 ergs/g absorption in muscle Half-Life • The time required for a radioactive substance to loose 1/2 of its radioactivity • Each radionuclide has a unique half-life • Half-lives range from extremely short (fraction of a second) to billions of years Example of the Effect of Half-Life • Assume an initial amount of 32 uCi of TC-99m with a half-life (T1/2) of 6 hours – after 1 half-life (6 h): 16 uCi – after 2 half-lives (12 h): 8 uCi – after 3 half-lives (18 h): 4 uCi – after 4 half-lives (24 h): 2 uCi • After 10 half-lives, less than 1/1000 of the original activity remains Selected Radionuclides with Radiations Radionuclide Radiation(s) Half-Life Eff. Half-Life Hydrogen-3 12 y 12 d Cobalt-60 5.26 y 10 d Strontium-90 28 y 15 y Iodine-131 8.05 d 8d Cesium-137 30 y 70 d Iridium-192 74 d - Radium-226 1602 y 44 y From Mettler, Jr., F.A. and Upton, A.C., Medical Effects of Ionizing Radiation 2 nd edition Radiation Dose • Absorbed Dose (D) • Dose Equivalent (HT) [ HT = DQ] 1 Gray (Gy) = 1 J/Kg 1 Seivert (Sv) = 1 J/Kg 1 rad = 100 ergs/g 1 rem = 100 ergs/g 100 rad = 1 Gy 100 rem = 1 Sv Deterministic Acute Effects Stochastic Late Effects Note: 1 MeV = 1.6 x 10-13 Joules Weighting Factors Organization NRC ICRU NCRP ICRP Weighting factor Q Q Q WR X &Gamma Rays 1 1 1 1 Beta Rays 1 1 1 1 Thermal Neutrons 2 5 5 Fast Neutrons 10 20 20 Hi Energy Protons 10 1 5 Alpha Particles 20 20 20 25 25 Radiation Doses and Dose Limits Flight from Los Angeles to London Annual public dose limit mrem Annual natural background Fetal dose limit Barium enema Annual radiation worker dose limit Heart catheterization (skin dose) Life saving actions guidance (NCRP-116) mrem Mild acute radiation syndrome LD50/60 for humans (bone marrow dose) mrem Radiation therapy (localized & fractionated) mrem 5 mrem 100 300 mrem 500 mrem 870 mrem 5,000 mrem 45,000 mrem 50,000 200,000 mrem 350,000 6,000,000 Radioactive Material • Radioactive material consists of atoms with unstable nuclei • The atoms spontaneously change (decay) to more stable forms and emit radiation • A person who is contaminated has radioactive material on their skin or inside their body (e.g., inhalation, ingestion or wound contamination) Examples of Radioactive Materials Radionuclide Physical Half-Life Cesium-137 30 yrs 1.5x106 Ci Food Irradiator Cobalt-60 5 yrs 15,000 Ci Cancer Therapy Plutonium-239 24,000 yrs 600 Ci Nuclear Weapon Iridium-192 Radiography 74 days 100 Ci Industrial Hydrogen-3 12 yrs 12 Ci Strontium-90 29 yrs 0.1 Ci Iodine-131 Therapy 8 days 0.015 Ci Nuclear Medicine Technetium-99m 6 hrs 0.025 Ci Diagnostic Imaging Americium-241 432 yrs Radon-222 4 days Activity 0.000005 Ci 1 pCi/l Use Exit Signs Eye Therapy Device Smoke Detectors Environmental Level Radiation vs. Radioactive Material • Radioactive Material – Any substance that spontaneously gives off radiation • Radiation – The energetic emissions of radioactive material – Can be in various chemical forms – Can be subatomic particles (, , n), photons (X-ray, ) or combinations – If not contained (sealed source) can lead to contamination External, Internal or Both – Results in ionization of the absorbing material (if living tissue radiation injury) Half-Life (HL) • Physical Half-Life Time (in minutes, hours, days or years) required for the activity of a radioactive material to decrease by one half due to radioactive decay • Biological Half-Life Time required for the body to eliminate half of the radioactive material (depends on the chemical form) • Effective Half-Life The net effect of the combination of the physical & biological half-lives in removing the radioactive material from the body • Half-lives range from fractions of seconds to millions of years • 1 HL = 50% 2 HL = 25% 3 HL = 12.5% Criticality Incident Operation Upshot/Knothole, a 1953 test of nuclear artillery projectile at Nevada Test Site Nuclear Fission Fissile Material • U-235 – Enriched from 0.7% (Natural) to 3% > 90% – Used: • Commercial Reactors • Research Reactors • Naval Reactors • Atomic Bomb • Pu-239 – Byproduct of U-235 fission – Used in Breeder Reactor – Also can be weaponized Radionuclides of Concern Causes of Radiation Exposure/Contamination • Accidents – Nuclear reactor – Medical radiation therapy – Industrial irradiator – Lost/stolen medical or industrial radioactive sources – Transportation • Terrorist Event – Low yield nuclear weapon – Radiological dispersal device (dirty bomb) – Attack on or sabotage of a nuclear facility Size of Event Event Radiation Accident Radioactive Dispersal Device No. of Deaths Most Deaths Due to None/Few Few/Moderate Radiation Blast Trauma (Depends on size of explosion & proximity of persons) Low Yield Large Nuclear Weapon (e.g. tens of thousands in an urban area even from 0.1 kT weapon) Blast Trauma Thermal Burns Radiation Exposure Fallout (Depends on Distance) Dose Limits - ICRP 60 Application Occupational Public Whole Body 20 mSv/year Effective dose averaged over 5 years, max: 50 mSv/yr 1 mSv in 1 year Lens of eye 150 mSv 15 mSv Skin 500 mSv 50 mSv Hands & Feet 500 mSv _ Annual Equiv. Dose: Emergency Exposure Guidelines - ICRP 60 Dose Limit (Whole Body) Activity Performed Conditions 5 rems All….. ……. 10 rems Protecting major property Where lower dose limit not practicable. 25 rems Lifesaving or protection of large Where lower dose limit populations not practicable >25 rems Lifesaving or protection of large Only on a voluntary basis populations to personnel fully aware of the risks involved Radiography Source Sealed Source Accident • 13 Curie Cs-137 Radiography Source • Found by a man at an Argentina construction site • Carried in front pockets for 18 hours Accident Dose Calculation • Cs-137 Gamma Constant = 0.323 R-m2/hr-Ci • 0.323 R-m2 hr-Ci x (18hr)(13Ci) (0.01m)2 = 755,820 R Accident Isodose Curves Basic Radiobiology • Atom Molecule Ionization in Water or Cell Molecules Chemical Damage Bond Breakage DNA Chromosomal Aberration Cell Death Mutation Radiosensitivity (most to least): • Lymphocytes • Endothelial Cells • Erythroblasts • Connective Tissue Cells • Myeloblasts • Tubular Cells of Kidneys • Epithelial Cells • Bone Cells – Intestinal crypts • Nerve Cells – Testis • Brain Cells – Ovary • Muscle Cells – Skin – Secretory glands – Lungs and bile ducts 19-A Classification of Medical Radiation Problems • Anxiety • Acute Radiation Syndrome • Local Radiation Injury • External Radionuclide Contamination • Local Trauma with Radionuclide Contamination • Internal Radionuclide Contamination Radiation Injuries • External exposure to penetrating radiation – Criticality Incident (,N) – Sealed Source (,) – External Contamination (, ) – Beam Generator (,N) • Internal contamination with radionuclides – Wound Contamination (, , ) – Injection (, , ) – Inhalation (, , ) – Ingestion (, , ) Late Health Effects from Radiation • Radiation is a weak carcinogen at low doses • No unique effects (type, latency, pathology) • Natural incidence of cancer ~ 40%; mortality ~ 25% • Risk of fatal cancer is estimated as ~ 4% per 100 rem • A dose of 5 rem increases the risk of fatal cancer by ~ 0.2% • A dose of 25 rem increases the risk of fatal cancer by ~ 1% What are the Risks to Future Children? Hereditary Effects • Magnitude of hereditary risk per rem is 10% that of fatal cancer risk • Risk to caregivers who would likely receive low doses is very small - 5 rem increases the risk of severe hereditary effects by ~ 0.02% • Risk of severe hereditary effects to a patient population receiving high doses is estimated as ~ 0.4% per 100 rem Fetal Irradiation No significant risk of adverse developmental effects below 10 rem Weeks After Period of Fertilization Development Effects <2 Pre-implantation Little chance of malformation. • Most probable effect, if any, is death of embryo. • Reduced lethal effects. 2-7 Organogenesis • Teratogenic effects. Fetal • Growth retardation. 7-40 • Impaired mental ability. • Growth retardation with higher doses. All • Increased childhood cancer risk. (~ 0.6% per 10 rem) Types of Radiation Hazards Internal Contamination • External Exposure whole-body or partialbody (no radiation hazard to EMS staff) • Contaminated - External Contamination External Exposure – external radioactive material: on the skin – internal radioactive material: inhaled, swallowed, absorbed through skin or wounds Radioactive Contamination • Contamination is simply the presence of radioactive material where it is not wanted • Persons may be contaminated either externally, internally or both • Exposure does not necessarily imply contamination In order to limit the amount of radiation you are exposed to, think about: SHIELDING, DISTANCE and TIME Shielding: If you have a thick shield between yourself and the radioactive materials more of the radiation will be absorbed, and you will be exposed to less. Distance: The farther away from the blast and the fallout the lower your exposure. Time: Minimizing time spent exposed will also reduce your risk. ALARA Techniques • Work quickly and efficiently (TIME) • Rotate personnel if qualified replacements are available (TIME) • When not involved in patient care, remain a few feet away from the patient (DISTANCE) • Use long-handled forceps to remove contaminated particles, contaminated dressings, etc. (DISTANCE) • Remove contaminated materials from the treatment area (DISTANCE & QUANTITY) • Put contaminated metal or glass in lead in lead “pigs” obtained from nuclear medicine department (SHIELDING) Radiation Protection: Reducing Radiation Exposure Time Minimize time spent near radiation sources To Limit Caregiver Dose to 5 rem Distance Distance time Maintain maximal practical distance from radiation source Rate Stay 1 ft min 12.5 R/hr 24 2 ft 3.1 R/hr 1.6 hr 5 ft 0.5 R/hr 10 hr 8 ft 0.2 R/hr 25 hr Shielding Place radioactive sources in a lead container Risk to Contaminated Patient • ARS, local radiation injury or contamination (both internal & external) never demands immediate medical attention. • Priority 1: True medical emergencies – ABC’s – Bleeding assessment – Trauma assessment – Wound assessment • Remove contaminated clothing as soon as reasonably possible (removes 80% of external contamination) • Proceed with decontamination procedures after patient stabilized Risk to Healthcare Provider • Minimal if using proper precautions • Remember ALARA techniques • Worst case - 15 mSv/hr close to contaminated wound • At 1 foot ( 30 cm) - 0.02 mSv/hr • NCRP public monthly equivalent dose to embryo/fetus: 0.5 mSv Healthcare Provider - Controlling the Spread of Contamination • Goal: Minimize and control contamination • Use proper protective clothing • Do not eat drink or smoke in contamination areas • Check yourself for contamination prior to leaving a potentially contaminated area • Limit access to treatment area to necessary personnel only Putting It All Together OUTLINE Radiation Terrorism and Response 1. Radiation Basics 2. Radiation Protection Rules 3. Radiation Threats Nuclear device, “dirty” bomb Equivalent Experiences: Chernobyl, Goiana 4. Health Management of Affected Population Mass Exposure Events • Criticality Events – Improvised Nuclear Device (IND) – Reactor Release • Nuclide Contamination – Radiological Dispersal Device (RDD) aka: Dirty Bomb – Intentional Contamination of Resources • External Radiation Source -- Industrial or Medical Source Injury Sources From Nuclear Device Detonation Terrorist Event Low yield nuclear weapon • Energy Distribution – 50% Blast – 35% Thermal Radiation – 15% Ionizing Radiation • Health Consequences – Injury – Burns – Penetrating Ionizing Radiation • Prompt (1/3) • Delayed (2/3) – Fallout • Contamination • Penetrating Ionizing Radiation A nuclear weapon is expected to cause many deaths and injuries: radiation is not the primary hazard • Blast and thermal effect comprise of the majority of effects/casualties • Radiation lethality out-distances thermal and blast damage only in low yield weapons (≤ 1 kiloton) Thermal: 35% of the energy 1st “flash” Pulse 2nd pulse (99% of the energy) The pattern is from the dark colored areas on her kimono Long distance visual effects Retinal burn: visual capacity is permanently lost in the burned area. Retinal burns can be produced at great distances from the nuclear detonation because the probability of occurrence does not follow the inverse square law as is true of many other types of nuclear radiation. Flash Blindness, also referred to as "dazzle," is a temporary impairment of vision. Victim does not have to be looking directly at the source for this to occur. Nighttime greatly increases distance of effect Fallout: important for surface bursts • A nuclear detonation results in a fireball with a temperature estimated to be several tens of millions of degrees. • The radioactive particles resulting from nuclear fission and activation of surrounding materials are carried up by the fireball and then drift downwind to later settle on the ground. Real-World Example Similar to Russian Suitcase Nukes Same type of nuclear warhead was used in a small artillery round, called Davy Crockett. Davy Crockett Fallout – NYC FOR TRAINING PURPOSES ONLY • Results from Davy Crockett overlaid on New York City map • Building that houses detonation device is destroyed • Adjoining buildings damaged • People within 1200 feet receive lethal dose of radiation (650,000 mrem or higher) from blast (not fallout) • 1~50,000 fatalities in estimation • 1~200,000 casualties 10,000 mrem/hr 1,000 mrem/hr 10,000 mrem/hr Lethal Dose Area Point of Detonation Atomic Weapon NuclideYields Approximate Yields of the Principal Nuclides per Megaton of Fission Nuclide Half-life MCi 89Sr 90Sr 95Zr 103Ru 106Ru 131I 137Cs 131Ce 144Ce bFrom Klement (1965) cFrom Knapp (1963) 53 d 28 y 65 d 40 d 1y 8d 30 y 1y 33 d 20.0b 0.1b 25.0b 18.5b 0.29b 125.0c 0.16b 39.0b 3.7b Environmental Radioactivity 4th Ed., Eisenbud M (1997) The Chernobyl Accident Chernobyl: Healthcare Resources Used • Local medical facilities • 400 special medical brigades – M.D., H.P., etc. • 15,000 health workers – 2,000 M.D.’s, 4,000 nurses, med students, etc • 213 mobile laboratories • Special hospitals (Kiev, Moscow) Chernobyl: Healthcare Procedures Medical Examinations 1,000,000 persons Dosimetric & lab 700,000 tests (216,000 children) Inpatient care 32,000 persons (12,000 children) Iodine prophylaxis 5,400,000 persons (1,700,000 children) Chernobyl: Aftermath • 31 deaths – 1 from roof collapse – 1 severe burns – 21 of 22 with ARS and skin burns (400-1600 r) – 7 of 23 (200-400 r) • Estimate additional 300 cases of thyroid cancer in exposed children and 100 cases in exposed adults. • 135,000 persons from 176 communities evacuated out to 30 km from plant • Dose to public (3-15 km zone): estimate 43 rem (50 year commited dose) Lessons Learned • In the USSR highly organized Civil Defense, Health system, Military and other government resources were quickly mobilized. • In the US less centralized resources might currently have more difficulties, although the maturation of the Homeland Security Agency should facilitate such a response. OUTLINE Radiation Terrorism and Response 1. Radiation Basics 2. Radiation Protection Rules 3. Radiation Threats Nuclear device, “dirty” bomb Equivalent Experiences: Chernobyl, Goiana 4. Health Management of Affected Population What Is a Radiation Threat? A radiation threat or "Dirty Bomb" is the use of common explosives to spread radioactive materials. It is not a nuclear blast. The force of the explosion and radioactive contamination will be more localized. In order to limit the amount of radiation you are exposed to, think about shielding, distance and time. Local authorities may not be able to immediately provide information on what is happening and what you should do. However, you should watch TV, listen to the radio, or check the Internet often for official news and information as it becomes available. Russian Nuclear SuitcaseDevices • 84 of 132 devices are missing “We do not know what the status of the other devices is, we just could not locate them…” Russian General Lebed, 1998 • “No direct evidence that any have been stolen.” US Assistant Sec of Defense of Nuclear Chemical Biological Programs, January 2003 Black Market Smuggling Total Number of Material Seizures (April 2001) • • • 217 low-grade nuclear material 14 weapons usable material 299 Radioactive Sources Sophisticated RDD May not be recognized before it is exploded Probability of RDD Terrorist Event Radiological dispersal device (dirty bomb) Health Consequences: Injury Burns Single Nuclide Contamination(?) Much higher probability than the use of a nuclear weapon: • Simple to build • Widely available materials • Ease of building simple explosives • More than 200 naturally-occurring and man-made radionuclides can be potentially used for RDD Background • After the 1991 Gulf War Iraqis disclosed they had worked on an RDD made of iron bombs packed with zirconium oxide irradiated in a research reactor. (USAF SAB, 1998 and IAEA documentation) • ~ 200 of the 2 million regulated radioactive sources and devices are lost, stolen, or abandoned each year in the USA. • Cesium-137, the most commonly lost radiation source has a 33 year half-life emits Beta (0.510, 1.17 MeV), and Gamma (~0.662 KeV) and substitutes for Potassium in the body. Radiation exposure from most RDDs in urban areas would expose many, kill few • The principal type of dirty bomb, or Radiological Dispersal Device (RDD), combines a conventional explosive, such as dynamite, with radioactive material. In most instances, the conventional explosive itself would have more immediate lethality than the radioactive material. At the levels created by most probable sources, not enough radiation would be present in a dirty bomb to kill people or cause severe illness. However, certain other radioactive materials, dispersed in the air, could contaminate up to several city blocks, creating fear and possibly panic and requiring potentially costly cleanup. Prompt, accurate, non-emotional public information might prevent the panic sought by terrorists. • A second type of RDD might involve a powerful radioactive source hidden in a public place, such as a trash receptacle in a busy train or subway station, where people passing close to the source might get a significant dose of radiation. • A dirty bomb is in no way similar to a nuclear weapon. The presumed purpose of its use would be therefore not as a Weapon of Mass Destruction but rather as a Weapon of Mass Disruption. Good reference: http://www.nrc.gov/reading-rm/doc-collections/fact-sheets/dirty-bombs.html Concerns • Immediate radiation injury—very few • Cancer—small (if any) increase on overall 25% probability of dying from cancer Exceptions: iodine and children’s thyroid cancer • Birth defects—only a concern for a few (if any), has been dramatically overestimated in the past Goiania Contamination Accident 454-2 Location of Goiania, Brazil 451-1 Goiania Accident Source 137Cs teletherapy source capsule: Physical form: CsCl hygroscopic powder with blue fluorescence as it absorbed moisture. Radioactivity: 50.9 TBq (1375Ci) Dose rate @1 m: 4.56 Gy/hr (456 rad/hr) Goiania Event Sequence 451-3 Goiania Medical Disposition 580-9 Goiania Casualty Burial Goiania Local Injury 454-5 Goiania Contaminated Areas 451-2 Goiania Population Screening 55-3 Goiania Accident Magnitude People monitored: Chromosome analyses: Roads monitored: Remediation workers: Above DL: 10 mSv CDE) 112,000 110 2,000 Km 755 38 (Highest: Homes contaminated: Demolished: 85 7 Vehicles contaminated: 50 Radwaste created: 3,800 - 200L drums Lessons Learned Lack of awareness of the detrimental health effects of radiation exposure can impede its recognition on the part of patients and medical practitioners until much damage is done. The alert M.D. who faces an unusual public health problem must find a collaborating H.P. to evaluate its possible radiogenic origin and if confirmed, to help deal with it. Shelter if you can’t evacuate • Use the Shelter to Shield and Distance yourself from the fallout contamination. Particle Filtering Factors • Filtration Efficiencies – Man’s cotton handkerchief, 16 thick. 94% – Man’s cotton handkerchief, 8 thick. 88% – Toilet paper, 3 thick. 91% – Bath towel, 2 thick. – Cotton Shirt, 2 thick. • Turn off ventilation 85% 65% Recommended Accumulated Dose Levels at which to Consider Evacuation and/or Relocation Fallout: The 7-10 Rule of Thumb Time (hours) Relative Fallout Dose Rates H + 1* 100% H + 7 (1•7) 10 % H+49 (7•7) 1% H+343 (7•7•7) ~14 Days 0.1% H+2401 (74) ~100 Days 0.01% • Shelter as long as possible before evacuating across fallout contamination. Waiting 2 days will reduce exposure by a factor of 100! Decontamination: important for nuclear weapons and radiation dispersal devices Evacuate the Fallout Path • Although dose rates are highest within the first few hours, this only represents a relatively small area • Evacuating the fallout area before fallout arrival will save the most lives If there is a radiation or a “dirty bomb” threat 1. If you are outside and there is an explosion or authorities warn of a radiation release nearby, cover your nose and mouth and quickly go inside a building that has not been damaged. If you are already inside check to see if your building has been damaged. If your building is stable, stay where you are. Close windows and doors; turn off air conditioners, heaters or other ventilation systems. If there is a radiation or a “dirty bomb” threat 1. If you are inside and there is an explosion near where you are or you are warned of a radiation release inside, cover nose and mouth and go outside immediately. Look for a building or other shelter that has not been damaged and quickly get inside. 2. Once you are inside, close windows and doors; turn off air conditioners, heaters or other ventilation systems. 3. If you think you have been exposed to radiation, take off your clothes and wash as soon as possible. 4. Stay where you are, watch TV, listen to the radio, or check the Internet for official news as it becomes available. If there is a nuclear blast If there is advance warning: Take cover immediately, as far below ground as possible, though any shield or shelter will help protect you from the immediate effects of the blast and the pressure wave. If there is no warning: 1. Quickly assess the situation. 2. Consider if you can get out of the area or if it would be better to go inside a building to limit the amount of radioactive material you are exposed to. 3. If you take shelter go as far below ground as possible, close windows and doors, turn off air conditioners, heaters or other ventilation systems. Stay where you are, watch TV, listen to the radio, or check the Internet for official news as it becomes available. To limit the amount of radiation you are exposed to, think about shielding, distance and time. Use available information to assess the situation. If there is a significant radioactive contamination threat, health care authorities may advise you to take potassium iodide. It may protect your thyroid gland, which is particularly vulnerable, from radioactive iodine exposure. Plan to speak with your health care provider in advance about what makes sense for your family. Conclusions • Radiation dispersal devices could cause significant contamination with low levels of radiation, but would result in few if any radiation casualties. Much of the radiation dispersal device’s impact will depend on how much we over-react to the dangers of radiation. • A nuclear weapon would result in substantial casualties and confusion from many effects, with radiation injury being the dominant one in the fallout region. In a fallout scenario, wise actions on sheltering/evacuation will save thousands of lives. • You can prepare by knowing (and teaching) the facts about radiation, and having a plan about what to do in a radiation emergency—a good place to start is www.ready.gov. OUTLINE Radiation Terrorism and Response 1. Radiation Basics 2. Radiation Protection Rules 3. Radiation Threats Nuclear device, “dirty” bomb Equivalent Experiences: Chernobyl, Goiana 4. Health Management of Affected Population The Real Medical Radiation Problems • Fear • Communication Failure • Uncertainty • Inaction • Chaos Key Points for Emergency Responders • Responders – Lifesaving first aid is the First Priority – Familiarize yourself with work area • Survey instrumentation, protective clothing, respiratory protection suitable to accident conditions – Evacuate personnel to safe areas – Assessment of radiological hazard • Public – Prevention is key as therapeutic measures are limited – Shelter vs Evacuation – Contamination • Rule of thumb: 80 - 90% contamination removed with clothing • Showering will remove an additional 7% Facility Preparation • Activate hospital plan – Obtain radiation survey meters – Call for additional support: Staff from Nuclear Medicine, Radiation Oncology, Radiation Safety (Health Physics) – Establish area for decontamination of uninjured persons – Establish triage area • Plan to control contamination – Instruct staff to use universal precautions and double glove – Establish multiple receptacles for contaminated waste – Protect floor with covering if time allows – For transport of contaminated patients into ED, designate separate entrance, designate one side of corridor, or transfer to clean gurney before entering, if time allows Decontamination Center • Establish a decontamination center for people who are contaminated, but not significantly injured. – Center should provide showers for many people. – Replacement clothing must be available. – Provisions to transport or shelter people after decontamination may be necessary. – Staff decontamination center with medical staff with a radiological background, health physicists or other staff trained in decontamination and use of radiation survey meters, and psychological counselors Protecting Staff from Contamination • Universal precautions • Survey hands and clothing with radiation meter • Replace gloves or clothing that is contaminated • Keep the work area free of contamination Key Points • Contamination is easy to detect and most of it can be removed • It is very unlikely that ED staff will receive large radiation doses from treating contaminated patients CLEAN AREA BUFFER ZONE CONTAMINATED AREA Treatment Area Layout Separate Entrance ED Staff Radiation Survey & Charting Contaminated Waste Waste Trauma Room STEP OFF PAD Radiation Survey Clean Gloves, Masks, Gowns, Booties HOT LINE Detecting and Measuring Radiation • Instruments – Locate contamination - GM Survey Meter (Geiger counter) – Measure exposure rate - Ion Chamber • Personal Dosimeters - measure doses to staff – Radiation Badge - Film/TLD – Self reading dosimeter (analog & digital) Patient Management - Priorities Triage • Medical triage is the highest priority • Radiation exposure and contamination are secondary considerations • Degree of decontamination dictated by number of and capacity to treat other injured patients Patient Management - Triage Triage based on: • Injuries • Signs and symptoms nausea, vomiting, fatigue, diarrhea • History - Where were you when the bomb exploded? • Contamination survey Classification of Medical Radiation Problems • Anxiety • Acute Radiation Syndrome • Local Radiation Injury • External Radionuclide Contamination • Local Trauma with Radionuclide Contamination • Internal Radionuclide Contamination 82-A Mass Casualties, Contaminated but Uninjured People, and Worried Well • An incident caused by nuclear terrorism may create large numbers of contaminated people who are not injured and worried people who may not be injured or contaminated • Measures must be taken to prevent these people from overwhelming the emergency department • A triage site should be established outside the ED to intercept such people and divert them to appropriate locations. – Triage site should be staffed with medical staff and security personnel – Precautions should be taken so that people cannot avoid the triage center and reach the ED Radiation Anxiety • In the event of a nuclear or radiological weapon detonation, thousands of victims will be concerned about their possible exposure to ionizing radiation. • Accurate knowledge of radiation dose can dramatically affect the assignment of triage category, BUT • accepted methods for accurate post-exposure dosimetry take days to measure. • Thus, clinical signs, symptoms and blood counts are best early indicators of radiation injury. Psychological Casualties • Terrorist acts involving toxic agents (especially radiation) are perceived as very threatening • Mass casualty incidents caused by nuclear terrorism will create large numbers of worried people who may not be injured or contaminated • Establish a center to provide psychological support to such people • Set up a center in the hospital to provide psychological support for staff Acute Radiation Syndrome • Depending on the magnitude of the exposure, the hematopoietic system, the gastrointestinal tract, the cardiovascular and central nervous systems may be involved in damage. There are three major forms (in order of severity): – Hematological form – Gastrointestinal form – Neurovascular form Thoma/Wald Prognostic Categories •Group 1: 0.5 to 1.5 Gy; mostly asymptomatic with occasional minimal prodromal symptoms •Group 2: 1.5 to 4 Gy; clinically manifested by transient N/V and mild hemotopoietic changes •Group 3: 4 to 6 Gy; clinically manifested by severe hematopoietic changes with some GI symptoms •Group 4: 6 to 14 Gy; clinically manifested by severe hematopoietic complications dominated by GI complications •Group 5: >50Gy; manifested by marked early neurovascular changes Acute Radiation Syndrome (Cont.) For Doses > 100 rem • Prodromal stage – nausea, vomiting, diarrhea and fatigue – higher doses produce more rapid onset and greater severity • Latent period (Interval) – patient appears to recover Time of Onset – decreases with increasing dose • Manifest Illness Stage – Hematopoietic – Gastrointestinal – CNS Severity of Effect Prodromal Appearance Time 39-J Clinical Effects of ARS Acute Local Radiation Injury Effect Erythema Time of Appearance (days) Threshold Dose (cGy) minutes to weeks (dose dependant) 600 at threshold 8-17 Epilation Dry desquamation Moist desquamation 17-21 300 21 1000-1500 14-21 1800-3000 Localized Radiation Effects - Organ System Threshold Effects • Skin - No visible injuries < 100 rem – Main erythema, epilation >500 rem – Moist desquamation >1,800 rem – Ulceration/Necrosis >2,400 rem • Cataracts – Acute exposure >200 rem – Chronic exposure >600 rem • Permanent Sterility – Female >250 rem – Male >350 rem Special Considerations • High radiation dose and trauma interact synergistically to increase mortality • Close wounds on patients with doses > 100 rem • Wound, burn care and surgery should be done in the first 48 hours or delayed for 2 to 3 months (> 100 rem) Emergency Hematologic Recovery Surgery No Surgery 24 - 48 Hours ~3 Months Surgery Permitted After adequate hematopoietic recovery OUTLINE Radiation Terrorism and Response 1. Radiation Basics 2. Radiation Protection Rules 3. Radiation Threats Nuclear device, “dirty” bomb Equivalent Experiences: Chernobyl, Goiana 4. Health Management of Affected Population Emergency Department Management of Radiation Casualties CAUTION Patient Management - Decontamination • Carefully remove and bag patient’s clothing and personal belongings (typically removes 95% of contamination) • Survey patient and, if practical, collect samples • Handle foreign objects with care until proven non-radioactive with survey meter • Decontamination priorities: – Decontaminate wounds first, then intact skin – Start with highest levels of contamination • Change outer gloves frequently to minimize spread of contamination Patient Management - Decontamination (Cont.) • Protect non-contaminated wounds with waterproof dressings • Contaminated wounds: – Irrigate and gently scrub with surgical sponge – Extend wound debridement for removal of contamination only in extreme cases and upon expert advice • Avoid overly aggressive decontamination • Change dressings frequently • Decontaminate intact skin and hair by washing with soap & water • Remove stubborn contamination on hair by cutting with scissors or electric clippers • Promote sweating • Use survey meter to monitor progress of decontamination Patient Management - Decontamination (Cont.) • Cease decontamination of skin and wounds – When the area is less than twice background, or – When there is no significant reduction between decon efforts, and – Before intact skin becomes abraded. • Contaminated thermal burns – Gently rinse. Washing may increase severity of injury. – Additional contamination will be removed when dressings are changed. • Do not delay surgery or other necessary medical procedures or exams…residual contamination can be controlled. Initial Management of Externally Contaminated Patient • Gross Decontamination – Removal of Contaminated Clothing – Washing and removal of Contaminated Hair – Removal of Gross Wound Contamination • Intermediate Stage (at clean location,if necessary) – Removal of Contaminated Clothing – Further Local Decontamination, Swabs of Body Orifices – Supportive Measures, First Aid • Final Stage – Patient Discharged with Fresh Clothing – More Definitive Decontamination (surgical) and Other Therapy at Dispensary or Hospital Handling contaminated patients Patient decontamination • Monitor to determine if decontamination is needed • Remove outer clothing • Wash exposed skin surfaces • Flush wounds with water • Do not scrub or abrade skin! Low levels of contamination are not a health hazard and can be left in place if not easily removed (they will decay quickly). Early Treatment For Radionuclide Contaminated Wounds • Irrigate Wound – Saline – Water • Decontaminate Skin (But Do Not Injure) – Detergent • Continue Wound Irrigation Until Radiation Level Is Zero or Constant • Treat Wound as Usual – Consider Excision of Embedded Long-Lived High- Hazard Contaminants Therapy For Isotope Decorporation • Dilution – 3H: Water – 32P: Phosphorus (Neutraphos) • Blocking – 137Cs: – 131I, 99Tc: – 90Sr, 85Sr: Prussian Blue KI (Lugol’s) Na-Alginate (Gaviscon), AlPhosphate or Hydroxide Gel (Phosphajel or Amphojel) Therapy For Isotope Decorporation (cont.) • Mobilization – 86Rb: Chlorthalidone (Hygroton) • Chelation – 252Cf, 242Cm, 241Am, 239Pu, 144Ce, – 210Pb: EDTA, Penicilamine – 210Po: Dimercaprol (BAL) – 203Hg, 60Co: Rare Earths, 143Pm, 140La, 90Y, 65Zn, 46Sc: DTPA Penicilamine Treatment of Internal Contamination • Radionuclide-specific • Most effective when administered early • May need to act on preliminary information • NCRP Report No. 65, Management of Persons Accidentally Contaminated with Radionuclides Radionuclide Cesium-137 Iodine-125/131 Strontium-90 Treatment Route Prussian blue Oral Potassium iodide Oral Aluminum phosphate Oral Americium-241/ Plutonium-239/ Cobalt-60 Ca- and Zn-DTPA IV /or nebulizer Treatment of Internal Contamination: Treatment Options • Reduce G.I. Absorption • Hasten Excretion • Use Blocking and Diluting Agents When Appropriate • Use Mobilizing Agents • Use Chelating Agents If Available Patient Management - Patient Transfer Transport injured, contaminated patient into or from the ED: • Clean gurney covered with 2 sheets • Lift patient onto clean gurney • Wrap sheets over patient • Roll gurney into ED or out of treatment room Facility Recovery • Remove waste from the Emergency Department and triage area • Survey facility for contamination • Decontaminate as necessary – Normal cleaning routines (mop, strip waxed floors) typically very effective – Periodically reassess contamination levels – Replace furniture, floor tiles, etc. that cannot be adequately decontaminated • Decontamination Goal: Less than twice normal background…higher levels may be acceptable Key Points • Medical stabilization is the highest priority • Train/drill to ensure competence and confidence • Pre-plan to ensure adequate supplies and survey instruments are available • Universal precautions and decontaminating patients minimizes exposure and contamination risk • Early symptoms and their intensity are an indication of the severity of the radiation injury • The first 24 hours are the worst; then you will likely have many additional resources Resources • Radiation Emergency Assistance Center/ Training Site (REAC/TS) (865) 576-1005www.orau.gov/reacts • Medical Radiobiology Advisory Team (MRAT) Armed Forces Radiobiology Research Institute (AFRRI) (301) 295-0530 www.afrri.usuhs.mil – Medical Management of Radiological Casualties Handbook, 2003; and Terrorism with Ionizing Radiation Pocket Guide • Websites: – www.bt.cdc.gov/radiation - Response to Radiation Emergencies by the Center for Disease Control – www.acr.org - “Disaster Preparedness for Radiology Professionals” by American College of Radiology – www.va.gov/emshg - “Medical Treatment of Radiological Casualties” • Books: Resources – Medical Management of Radiation Accidents; Gusev, Guskova, Mettler, 2001. – Medical Effects of Ionizing Radiation; Mettler and Upton, 1995. – The Medical Basis for Radiation-Accident Preparedness; REAC/TS Conference, 2002. – National Council on Radiation Protection Reports No. 65 (Contaminated Patient Care) and No. 138 (Radiation Injury Care). • Articles: – “Major Radiation Exposure - What to Expect and How to Respond,” Mettler and Voelz, New England Journal of Medicine, 2002, 346: 155461. – “Medical Management of the Acute Radiation Syndrome: Recommendations of the Strategic National Stockpile Radiation Working Group,” Waselenko, et.al., Annals of Internal Medicine, 2004, 140: 1037-1051. – Guidebook for the Treatment of Accidental Internal Radionuclide Contamination of Workers; Gerber, Thomas RG (eds), Radiation Protection Dosimetry, 1992.