CONSCIOUS SEDATION
advertisement

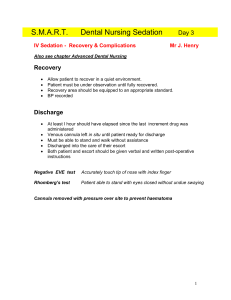
Dr. CATHERINE GALLANT Department of Anesthesiology University of Ottawa General Campus OUTLINE Definition Indications for use Contraindications Pharmacology Complications DEFINITION A technique to provide an altered state of consciousness by administration of medications that permits a patient to undergo painful procedures but still respond to verbal commands while maintaining an unassisted airway INDICATIONS Used to facilitate many diagnostic and therapeutic procedures May be used intra-operatively May be performed in a location remote from the operating room Ever increasing demand fuelled by patients Limited capacity for anesthesiologists to provide these services APPLICATIONS Primarily day surgeries Lack of dependence on hospital beds More flexibility in scheduling Shorter waiting lists Improved efficiencies Low morbidity and mortality Low rates of complications Lower costs Less special investigations required APPLICATIONS Dental Dermatology Gynecology General surgery Ophthalmology Orthopedics Pain Clinic Plastic surgery Urology DEFINITIONS Analgesia - Relief of pain without intentionally producing a sedated state. Altered mental status may occur as a secondary effect of medications administered for analgesia. DEFINITIONS Minimal sedation – drug induced state where the patient responds normally to verbal commands. Cognitive function and coordination may be impaired but ventilatory and cardiovascular function are unaffected. Anxiolysis alternate term DEFINITIONS Moderate sedation and analgesia – a drug induced depression of consciousness where the patient responds purposefully to verbal commands alone or when accompanied by light touch. Protective airway reflexes and adequate ventilation are maintained without intervention. Cardiovascular function remains stable. Conscious sedation DEFINITIONS Deep sedation and analgesia - A drug induced depression of consciousness where the patient cannot be easily aroused but responds purposefully to noxious stimulation. Assistance may be needed to ensure the airway is protected and adequate ventilation maintained. Cardiovascular function is usually stable. DEFINITIONS General anesthesia – a drug induced loss of consciousness, during which the patient cannot be aroused, even with painful stimuli, and often requires assistance to protect the airway and maintain ventilation. Cardiovascular function may be impaired. EUROPEAN UNION OF MEDICAL SPECIALISTS Level 1 Fully awake Level 2 Drowsy Level 3 Rousable by normal speech OBJECTIVES To achieve sedation level 2 and 3 (minimal to moderate sedation) which allows patients to undergo and tolerate unpleasant procedures To avoid deeper levels of sedation and the related complications This cannot be completely avoided! Continuum which is difficult to divide into discrete stages Always maintain verbal contact BENEFITS Appropriate sedation/analgesia will allow the patient to tolerate unpleasant procedures by relieving anxiety, discomfort or pain In the uncooperative patient, sedation/analgesia may facilitate those procedures which are not uncomfortable but which require that the patient not move QUALIFIED INDIVIDUALS Competency based education, training and experience in: Patient evaluation Performance of sedation Knowledge of pharmacology of drugs used Rescuing the patient from complications of deeper levels of sedation Airway compromise Inadequate ventilation Cardiovascular instability PATIENT EVALUATION Screening for medical risk factors How will these alter response to sedation? Abnormalities of major organ systems? Previous adverse reactions with sedation/analgesia as well as regional and general anesthesia? Allergies to drugs? Medications – drug interactions? History of drug and alcohol abuse? NPO status PATIENT EVALUATION Abnormalities of major organ systems Cardiac Respiratory Renal Hepatic PATIENT EVALUATION Previous adverse reactions with sedation/analgesia as well as regional and general anesthesia Details Where it happened PATIENT EVALUATION • Allergies to drugs? What is the reaction? When did it occur? Family history? PATIENT EVALUATION • History of drug and alcohol abuse? May indicate tolerance Cross tolerance between classes of drugs PATIENT EVALUATION Review medications – possible drug interactions? MAOIs such as phenelzine (Nardil) , tranylcypromine (Nardil), moclobemide PATIENT SELECTION Focused physical exam Evaluation of airway Auscultation of heart and lungs Assessment vital signs Review labs Consider consult prn PATIENT SELECTION Airway issues that may present concerns History Previous problems with anesthesia or sedation Snoring, stridor or sleep apnea Advanced rheumatoid arthritis Chromosomal abnormalities e.g. trisomy 21 Physical examination Obesity especially involving neck and facial structures PATIENT SELECTION Airway issues that may present concerns Physical examination Short neck, limited neck extension, decreased TMD of < 3 cm in adult, neck mass, c-spine disease or trauma, tracheal deviation, dysmorphic features Small mouth opening (< 3 cm in adult), protruding incisors, loose or capped teeth, dental appliances, high arched palate, macroglossia, tonsillar hypertrophy Micrognathia, retrognathia, trismus, significant malocclusion DIFFICULT AIRWAY PATIENT SELECTION Who is a candidate for sedation? ASA 1 and ASA 2 ASA 3 in stable condition Must be compatible with the procedure Must be capable of giving informed consent PATIENT SELECTION Who is at increased risk of complications? Extremes of age Multiple co-morbidities Severe systemic disease Drug and/or alcohol abuse Uncooperative patient Morbidly obese patient Potential difficult airway Obstructive sleep apnea ADVANCED AGE Higher risk of adverse events Increased sensitivity to sedative drugs Medication interactions Higher peak serum levels of medications MULTIPLE CO-MORBITIES ↑ing ASA status correlates with ↑ing risk of adverse events (ASA III or >) Any co-morbidity that increases risk of cardiorespiratory depression with sedatives is significant CHF, neuromuscular disease COPD, dehydration Anemia PATIENT SELECTION Who is not a candidate? Language barrier History of problems with previous anesthesia Known or suspected difficult ventilation or difficult intubation No person to accompany them home PREPARATION Do you have informed consent? Is patient aware of risks and the limitations? Have they been given alternative choices to procedure? Have questions been answered? What is the NPO status? Risks versus benefits Machine and drug check? Drugs and antagonists Emergency equipment available and checked? Defibrillator and skills of use ASPIRATION RISK Fasting pre-procedure decreases risks during moderate sedation and strongly decreases risks during deep sedation ASA guidelines recommend if procedure is elective fasting guidelines should be as for GA If not met then consider delaying procedure, reducing sedation level or ETT If emergency then may have to reconsider approach SUMMARY OF ASA PREPROCEDURE FASTING GUIDELINES INGESTED MATERIAL MINIMUM FASTING PERIOD Clear liquids 2 hours Breast milk 4 hours Infant formula 6 hours Nonhuman milk 6 hours Light meal 6 hours EQUIPMENT Dedicated qualified personnel Must be uninterrupted and continuous presence IV access Airway adjuncts Bag valve mask, oral and nasal airways, equipment for endotracheal intubation Suction for secretions MONITORING Does monitoring level of consciousness decrease risks of complications when administering procedural sedation? MONITORING Maintain verbal contact with patient Blood pressure, heart rate, respiratory rate measured at regular intervals Oxygen saturation, cardiac rhythm and ETCO2 should be monitored continuously MONITORING Monitor patients response to medication and procedure Level of alertness, depth of respiration and response to painful stimuli all determine subsequent dosing MONITORING Supplemental oxygen often recommended to maintain oxygen reserves and prevent hypoxemia May delay recognition of hypoventilation ETCO2 monitoring useful Brief episodes hypoxemia and hypoventilation may occur – clinical significance? TECHNIQUES Technique will vary from patient to patient Dosing of analgesics and anxiolytics vary widely Dosing depends on procedure as well as the anxiety of the patient Comfort measures contribute to reducing anxiety and pain TECHNIQUES Anxiety may be reduced by other methods than pharmacological Preoperative explanation of the procedure Calm and reassuring manner Quiet atmosphere with appropriate music Comfortable room temperature or warm blankets AGENTS USED Ideal drug has rapid onset of action and short duration of action, will maintain hemodynamic stability and have no side effects No single drug available with all of these features AGENTS USED Anxiolytics Benzodiazepines Diazepam, midazolam, lorazepam Benzene ring fused to diazepine ring All highly lipophilic Highly protein bound All absorbable after po administration MIDAZOLAM Midazolam most commonly used Rapidly enters CNS then redistributed Works through GABA pathways Distribution of GABA receptors restricted to CNS Minimal effects outside of CNS Most important clinical effects Sedative-hypnotic Amnestic Anxiolysis Anti-convulsant No analgesia MIDAZOLAM Favorable side effect profile Minimal depression of ventilation May cause mild ↓BP esp in hypovolemic patient Synergistic with narcotics Combo may cause severe respiratory depression Antagonist available: Flumazenil Dosage 10 to 25 µcg/kg q 3 to 5 minutes AGENTS USED Propofol Phenol derivative, highly lipophilic Can be painful on injection Rapidly metabolized in liver with high plasma clearance Onset within 40 seconds with duration 8 - 10 minutes Causes peripheral vasodilatation ↓ BP more pronounced with ↑ age , ↓ intravascular volume or with rapid injection PROPOFOL Potent respiratory depressant with ↑ doses ↓MV through ↓TV and RR Has anti-emetic effects Sedative and amnestic not analgesic No reversal agent Difficult to titrate in some cases, can cause very deep sedation PROPOFOL Dosage unchanged if renal or liver impairment Metabolism appears to be slower in elderly Reduce doses by 20% and increase dosing interval 100 to 500 µcg/kg every 3 to 5 minutes bolus Continuous infusion 25 to 100 µcg/kg/min May require addition of short acting opioids due to absence of analgesic activity. This increases risk of respiratory complications KETAMINE Highly lipid soluble derivative phencyclidine Rapid onset of action Use limited by side effects Dreams, halllucinations, out of body experiences Significant cardiovascular effects Sympathomimetic ↑BP, HR, CO Minimal respiratory depression Bronchodilatation KETAMINE Profound analgesia Multiple routes of administration May supplement inadequate regional anesthesia 50 to 100 mcg/kg usual single dose No more than 10 mg/hour to avoid side effects PENTOTHAL IV barbiturate, induction agent Hypnotic, sedatives, anticonvulsants Undergoes hepatic metabolism Recovery after bolus comparable to propofol because of redistribution to inactive tissue sites Even single boluses can lead to psychomotor impairment for several hours PENTOTHAL CNS depressant “Anti-analgesic” properties May reduce pain threshold ↓BP due to peripheral vasodilation Transient as compensatory ↑ HR Respiratory depressant ↓ TV and ↓ RR – transient apnea ETOMIDATE IV anesthetic with minimal hemodynamic effects Hypnotic but no analgesic properties Rapid onset of anesthesia – almost immediate - with minimal changes in HR and CO Usual dosing 0.1 to 0.15 mg/kg IV for PSA Causes adrenocortical suppression so not widely used Myoclonus also seen frequently AGENTS USED Miscellaneous agents Chloral hydrate Pentobarbital Methohexital Dexmedetomidine Local anesthetics May reduce doses of sedatives and narcotics Useful as co-analgesics OPIOIDS High degree of variability in dose response Inter-individual variation Analgesia, euphoria, sedation, ↓ concentration Clearance primarily hepatic metabolism May be active metabolites SIDE EFFECTS Cardiovascular May produce orthostatic hypotension Respiratory Dose dependent depression of ventilation Decreased responsiveness to CO2 May persist for several hours Apnea CNS Do not reliably produce unconsciousness Skeletal muscle rigidity SIDE EFFECTS Sedation Nausea and vomiting Direct stimulation CRTZ dopamine receptors Biliary tract Spasm of biliary smooth muscle May be confused with angina AGENTS USED Fentanyl Synthetic opioid structurally related to meperidine (phenylpiperidine derivative) 75 to 125 times more potent than morphine More lipid soluble than morphine – crosses BBB Short acting with rapid redistribution to tissue Clinically rapid onset (2 to 3 minutes) No amnestic properties FENTANYL Primary side effect is respiratory depression Will potentiate sedative effects of other drugs Wide range of doses 0.25 to 0.5 µcg/kg q 3 to 5 minutes 1 to 2 µcg/kg for analgesia With multiple bolus doses or continuous infusion the duration of action is prolonged ALFENTANIL 1/5 to 1/10th potency fentanyl More rapid onset and shorter duration 1.4 minutes May be useful for retrobulbar blocks 10 fold inter-individual variation in dosing • 0.1 to 0.4 µcg/kg/min by infusion REMIFENTANIL Unique because of ester linkage and metabolism by plasma esterases Short acting, titratable, rapid onset and offset, rapid recovery after infusion Boluses excellent for short painful procedures Doses 0.25 to 1 µcg/kg Infusions for sedation Doses 0.05 to 0.2 µcg/kg/min TECHNIQUES May be by intermittent bolus or by continuous infusion “Target controlled infusions” Plasma levels Effect site levels TECHNIQUE Monotherapy may be desirable Short acting drugs may be desirable Onset of action Small increments If synergistic action reduce to ¼ usual dose Antagonists readily available TECHNIQUE Sedation and inadequate block Surgeon may have to supplement if block is inadequate Duration of surgery may exceed duration of local anesthetic Restlessness and hypoxia Consider in differential diagnosis TIPS If elderly or co-morbid disease then may be more conservative with approach Start with lower dose Administer meds more slowly Be aware of slower circulation times Redose at less frequent intervals TIPS NEVER BE AFRAID TO CALL FOR HELP COMPLICATIONS Serious complications rare All sedatives and narcotics will cause adverse reactions in some patients even within recommended doses Extremes of age most at risk Most sedatives cause dose dependent respiratory depression Risk of desaturation up to 11% with propofol, even with supplemental oxygen Hypoventilation and apnea usually easily treated COMPLICATIONS Treat respiratory complications with patient stimulation, oxygen, airway positioning or brief ventilatory support Cardiovascular instability uncommon More likely to occur if significant cardiac morbidity Hypotension and bradycardia may develop in patients on CV depressants Usually transient COMPLICATIONS Vomiting Seen in approximately 5% PSA More common if narcotics given Little evidence regarding prophylaxis Inadequate sedation preventing completion of procedure Over sedation Agitation Allergic reactions COMPLICATIONS Inadequate evaluation Inadequate monitoring Inadequate practitioner skills Premature discharge RECORDS Vital signs and level of consciousness Document at baseline Regular, frequent intervals during the procedure Regular, frequent intervals during recovery Prior to discharge RECOVERY PERIOD Requires monitoring as during procedure Patients may be at increased risk after removal of painful stimulus What is ideal length of recovery period? Various criteria available such as Aldrete Consciousness Respiration Activity Saturation Circulation Consider pain and nausea DISCHARGE CRITERIA Fully conscious Respond appropriately Walk unassisted Baseline vital signs Pain, nausea and vomiting, bleeding all under control Must have accompanying responsible person AFTERCARE Responsible accompanying person for 24 hours Written detailed instructions for dealing with complications Medical assistance readily available Should be contacted next day by phone No major life decisions, driving or alcohol for 24 hours REFERENCES Practice Guidelines for Sedation and Analgesia by Non-Anesthesiologists - ASA Basics of Anesthesia 5th edition - Stoelting CLINICAL SCENARIOS You are asked to provide sedation for cataract surgery to an 80 year old male. He has a history of controlled hypertension. NKDA. Medications: Atenolol 50 mg bid Any concerns? What would you choose for sedation for this patient? The procedure finishes and you bring the patient back to the PACU in stable condition. 15 minutes later you receive a call that your patient is no longer responsive What is your differential diagnosis? How do you approach the management? You are monitoring a 62 year old patient under spinal anesthesia for a total knee replacement when she suddenly becomes bradycardic - HR drops to 45 (from 70) What are your first steps? What treatment would you give – if any? You are in the endoscopy suite providing sedation for colonoscopy. Your patient is a 50 year old for routine screening with no significant past medical history. 10 minutes into the procedure BP drops to 100/60 from baseline 135/72 Any concerns? You are monitoring a 73 yo male under SAB who is undergoing TURP. One hour into the procedure he is becoming increasingly restless. You give 1 mg midazolam IV. He becomes more confused and pulls out his IV Differential??