Risk Assessment
CAADA-DASH-RIC
Michelle Robson (Newham) / Rachel Ozanne (Camden)
Why assess for DV?
•
By not asking we may be increasing risk to a client and possibly ignoring a major
driver for their substance use.
•
Increased risk of harm due to:
– Acute/chronic effect that alcohol/drugs may prevent them from accurately
assessing the level of danger posed by perpetrator
– Under the influence they may feel more powerful – may believe can defend
themselves/fight back – not realising the substances impact on their gross
motor functioning or reflexes
– Impaired judgement/thought process/memory – makes safety planning more
difficult.
•
Models of Care (NTA)
– The experiences of violence and abuse may be severely impacting on your
service users ability to engage and retain in treatment.
– Duty of care – if you are working with both partners there is a duty of care to
ensure the safety and well being of the service user who is the victim of violence
•
Legal responsibility
– section 17 Crime and Disorder Act – there is a responsibility to take ‘reasonable’
action to prevent a crime which includes domestic violence.
Slide 2
DV & Substance Use
•
50 – 90 % of women in Drug & Alcohol services report experiencing current or past
physical, emotional or sexual abuse
•
Merry go round = Substance use makes it harder to escape a violent situation or heal
from past violence – continuing violence or unresolved feelings about abuse make it
harder to give up drugs/alcohol (Illinois DHS 2000)
•
Ignoring alcohol/drug issues might result in:
–
–
–
–
–
Your client may be less able to leave a violent relationship
In greater danger of more severe violence
Ineffective criminal justice intervention
More likely to lose children
Less likely to benefit from counselling
•
Are we asking the right questions – in the right way?
•
Asking about drug/alcohol use – Samples :
–
–
–
–
–
Normalise – some people find alcohol/drugs help them cope – does this apply to you?
Assume use - How much alcohol do you drink each day? What sort of substances do you use?
What do you use to cope with the violence/pain?
Do you drink any alcohol or use any drugs, prescription medication etc?
Does your partner ever make you feel like you have to use drugs/alcohol?
Slide 3
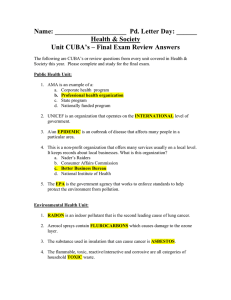
Risk Identification Checklist
•
Safety of victim must be main concern
– Substance use may impacts on ability to remain safe
– May not be able to begin addressing substance use
unless safe
•
Women often disclose at different times during their
intervention
•
Confidentiality (perpetrator may also be a client)
•
Safety planning needs to be included in treatment/care plans
Slide 4
Risk Identification Checklist
• ANOTHER RISK ASSESSMENT
– Not an NTA requirement
– Not on NTDMS
• SU RISK Assessment
– At best asks whether the client has or is experiencing DV (many
don’t ask this or ask in an appropriate way)
– Identify there is a risk – then what?
• Need to assess level and plan treatment accordingly / monitor
regularly (re-assess)
Slide 5
Risk Identification Checklist
•
•
•
•
•
•
•
•
•
•
•
•
•
Has the current incident resulted in injury?
(Please state what and whether this is the first injury)
Are you very frightened?
What are you afraid of? Is it further injury or violence? (Please give an indication of what you think
(name of abuser (s)…) might do and to whom, including children).
Do you feel isolated from family/friends i.e. does (name of abuser (s)…) try to stop you from seeing
friends /family/doctor or others?
Are you feeling depressed or having suicidal thoughts?
Have you separated or tried to separate from (name of abuser (s) …) within the past year?
Is there conflict over child contact?
Does (…) constantly text, call, follow, stalk or harass you? (Please expand to identify what and
whether you believe that this is done deliberately to intimidate you? Consider the context and
behaviour of what is being done)
Are you pregnant or have you recently had a baby (within the last 18mths)?
Is the abuse happening more often?
Is the abuse getting worse?
Does (…) try to control everything you do and/or are they excessively jealous? (In terms of
relationships, who you see, being ‘policed at home’, telling you what to wear for example.
Slide 6
Risk Identification Checklist
•
•
•
•
•
•
•
•
•
Has (…) ever used weapons or objects to hurt you?
Has (…) ever threatened to kill you or someone else and you believed them? (If yes,
tick who)
You Children Other (please specify)
Has (…) ever attempted to strangle/choke/suffocate/drown you?
Does (…) do or say things of a sexual nature that make you feel bad or that physically
hurt you or someone else? (If someone else, specify who)
Is there any other person who has threatened you or who you are afraid of? (If yes,
please specify whom and why. Consider extended family if HBV)
Do you know if (…) has hurt anyone else? (Please specify whom including the
children, siblings or elderly relatives. Consider HBV) Children Another family
member Someone from a previous relationship Other (please specify)
Has (…) ever mistreated an animal or the family pet?
Are there any financial issues? For example, are you dependent on (…) for
money/have they recently lost their job/other financial issues?
Has (…) had problems in the past year with drugs (prescription or other), alcohol or
mental health leading to problems in leading a normal life? (If yes, please specify
which and give relevant details if known) Drugs Alcohol Mental Health
Slide 7
Risk Identification Checklist
•
•
•
Has (…) ever threatened or attempted suicide?
Has (…) ever broken bail / an injunction and / or formal agreement for when they can see you and /
or the children?
– (You may wish to consider this in relation to an ex-partner of the perpetrator if relevant)
Do you know if (…) has ever been in trouble with the police or has a criminal history?
– (If yes, please specify) DV Sexual violence Other violence Other
•
Total ‘yes’ responses – 14 ticks threshold – DOES NOT NEGATE PROFESSIONAL JUDGEMENT
•
For consideration by professionals:
– Is there any other information (from victim or professional) which may increase risk level?
– Consider victim’s situation in relation to disability, substance misuse, mental health issues,
cultural/language barriers, ‘honour’-based systems and minimisation.
– Consider abuser’s occupation/interests – could this give them unique access to weapons?
– What are the victim’s greatest priorities to address their safety?
•
Do you believe that there are reasonable grounds for referring this case to MARAC? Yes/No
•
Do you believe that there are risks facing the children in the family? Yes / No
Slide 8
What is needed for this to work.
•
NOT GOOD PRACTICE TO BE A TICK BOX EXERCISE
•
Training on Domestic Violence
•
Training on RISK in relation to DV specifically
– Understand professional judgement
•
Ensuring links with DV Services
•
MARAC - Representative
Slide 9