Good Morning!!!
advertisement
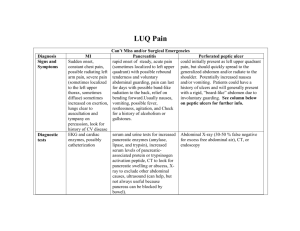
Morning Report July 9, 2012 Symptoms Acute (or subacute) Chronic Localized Diffuse Single (ie. Monoarticular) Multiple Static Progressive Constant Intermittent Single Episode Recurrent Abrupt Gradual Severe Mild Painful Nonpainful Bilious Nonbilious Sharp/Stabbing Dull/Vague Predisposing Conditions Age, gender, preceding events (trauma, viral illness, etc), medication use, past medical history (diagnoses, surgeries, etc) Pathophysiological Insult What is physically happening in the body Clinical Manifestations Signs and symptoms that result from the pathophysiological insult Use semantic qualifiers GER/GERD Protein intolerance Gastroenteritis Pyloric stenosis UTI Malrotation with midgut volvulus Intestinal atresia/stenosis Intussusception Predisposing conditions Presentation in the first few months of life, peaks at 4 months Resolves in up to ~90% by 12 months and nearly all by 24 months Likely combination of genetic predisposition and environmental factors (liquid diet /overfeeding/horizontal body positioning) Immature lower esophageal sphincter Pathophysiological insult Passage of stomach contents into the esophagus, can be physiologic Disease state caused by frequent or persistent episodes of esophageal exposure to caustic gastric contents that produce esophagitis/esophageal symptoms or respiratory sequelae or failure to thrive Clinical manifestations Postprandial regurgitation, nonbillious Irritability, arching, choking, gagging, feeding aversion Failure to thrive Respiratory symptoms of obstructive apnea, stridor, or lower airway disease Sandifer syndrome Predisposing conditions Manifests in the first several months of life First form of allergy to affect infants and children About 2.5% of children experience this allergy within the first 3 yrs of life Most children “outgrow” this allergy, ~50% resolve within 3-5 years Pathophysiological insult Cell-mediated hypersensitivities Lymphocytes, primarily food allergen-specific T cells, secrete cytokines that lead to chronic inflammatory process in skin, GI tract, or respiratory tract Most commonly provoked by cow’s milk or soy-based formulas Clinical manifestations Irritability Protracted vomiting and diarrhea that may result in dehydration Vomiting generally occurs 1-3hrs after feeds Prolonged exposure leads to abdominal distention, bloody diarrhea, anemia, and failure to thrive Predisposing conditions Risks include environmental contamination , increased exposure to enteropathogens Young age, immunodeficiency, malnutrition, lack of exclusive or predominant breast-feeding 2nd leading cause of child mortality worldwide Pathophysiologic insult Numerous pathogens: viral, bacterial, and parasitic Noninflammatory diarrhea caused by enterotoxin production by some bacteria, destruction of villus cells by viruses, adherence by parasites, and adherence and/or translocation by bacteria Inflammatory diarrhea caused by bacteria that directly invade the intestine or produce cytotoxins that cause fluid, protein and cells to enter the intestinal lumen Clinical manifestations Acute onset of vomiting followed by diarrhea, abdominal cramps, and possible fever Vomiting is a self-protective process that may reduce the load of infectious organisms or associated toxins/irritants Watery versus bloody diarrhea related to etiology Timing of symptoms related to whether preformed toxins are present and to the enteropathogen involved Predisposing conditions Males affected 4 to 6 times more frequently 1/3 of cases in first-born infants Genetic predisposition Use of erythromycin Increased incidence with B and O blood types Pathophysiological insult Hypertrophy and spasm of the pyloric muscle resulting in gastric outlet obstruction Abnormal muscle innervation, elevated serum levels of prostaglandins, and infant hypergastrinemia have been implicated Also, reduced neuronal nitric oxide might contribute to the pathogenesis Clinical manifestations Typically a 3- to 6-week-old infant with progressive or intermittent vomiting after feeding Nonbilious emesis, often projectile in nature Infant is often hungry after vomiting Hypochloremic hypokalemic metabolic alkalosis and dehydration Palpable small “olive-shaped mass” in right midepigastric area, visible gastric peristaltic wave after feeding Predisposing conditions Female, uncircumcised males Primary or secondary urinary tract obstructions Indwelling catheters Pathophysiological insult Cystitis – infection localized to the bladder Pyelonephritis – infection of the renal parenchyma, calyces, and renal pelvis Renal abscess – intrarenal or perinephric Most common organism: E. coli; other organisms: Enterococcus, Pseudomonas, Klebsiella, Proteus, S. saprophyticus Clinical manifestations Neonates: failure to thrive, feeding problems, direct hyperbilirubinemia Infants: feeding problems, failure to thrive, vomiting, diarrhea, unexplained fever >2yrs: urgency, dysuria, frequency, abdominal pain Predisposing conditions Majority present in first year of life, >50% present within first month of life Often associated with other abnormalities of the abdominal wall – such as diaphragmatic hernia, gastroschisis, and omphalocele Also associated with heterotaxy syndrome – complex of congenital anomalies including congenital heart disease, malrotation, and either asplenia or polysplenia Pathophysiological insult Nonrotation occurs when, in utero, the bowel fails to rotate after it returns to the abdominal cavity; leaving the cecum near the right upper quadrant This results in an extremely narrow mesenteric root susceptible to volvulus Abnormal mesenteric attachments (Ladd bands) extend from the cecum across the duodenum, causing partial obstruction Clinical manifestations About ~60% of children with malrotation present with bilious vomiting during the first month of life – Could be due to duodenal obstruction by Ladd bands or volvulus If bilious emesis due to volvulus, then venous drainage of the gut is impaired, leading to ischemia, pain, tenderness, and possibly bloody stools If the bowel undergoes ischemic necrosis, the child may appear septic Predisposing conditions Congenital partial or complete blockage of the intestine (1:1500 live births) Small intestine is the most common site of intestinal atresia/stenosis (~90%) Possible prenatal history of polyhydraminos Pathophysiological insult Intrinsic causes include inherent abnormalities of intestinal innervation, mucus production, or tubular anatomy Extrinsic causes involve compression of the bowel by vessels, organs (annular pancreas), and cysts Clinical manifestations Classic symptoms: bilious vomiting and abdominal distention Findings more subtle if the obstruction is partial Obstruction high in the intestinal tract results in highvolume, frequent, bilious emesis with little or no distention. Pain is intermittent and usually relieved by vomiting. Obstruction in the distal small bowel leads to moderate or marked abdominal distention with emesis that is progressively feculent. Predisposing conditions Most common between 3 months – 6 years of age, Rare in neonates Most common abdominal emergency in children <2years Male:female ratio of 3:1 90% idiopathic; 2-8% with recognizable lead points Seasonal peaks in spring and autumn Risk factors: Lymphoid nodular hyperplasia, HSP, CF Pathophysiological insult Proximal intestine is telescoped into a distal portion of intestine Most often ileocolic, less common cecocolic and rarely ileo-ileal Constriction of the associated mesentery leads to venous congestion, edema and intestine ischemia, then mucosal bleeding Clinical manifestations Sudden onset of severe paroxysmal colicky pain that recurs Painful episodes associated with legs and knees flexed Lethargy can be associated and out of proportion to the abdominal symptoms Vomiting occurs in most cases, nonbilious in the early phase and can be bilious in the later phase “Currant jelly stool” “Sausage-shaped mass” may be palpable Predisposing Conditions Age 6-24 months Very rare before 3 months and after 6 years Male: Female 3:1 90% - no etiology, healthy child Sometimes associated with viral Illness or gastroenteritis Rare cases: HSP, CF, Celiac dz, Crohn disease, leukemia Pathophysiologic Insult Telescoping of the intestine into an area distal to it 95% involve the ileocecal valve Age < 2 years: typically no etiology for lead point Older children: 5-10% have lead point Meckel’s, polyp, appendiceal stumps, enteric duplication, ectopic pancreas, foreign body, mass Compressed mesentery venous obstruction intestinal mucosal ischemia leakage of blood and mucus into lumen Bowel ischemia can lead to release of endogenous opiods Clinical Manifestations Intermittent, colicky episodes of abdominal pain Normal between episodes Vomiting (starts non-bilious, may progress to bilious) Bloody stool Abdominal exam often normal Pain over site of intussusception; “sausage mass” Lethargy Abdominal x-rays 25% show normal gas pattern Crescent sign Ultrasound Target sign Very accurate Test of choice Contrast or air enema Diagnostic and therapeutic Surgery aware and present More successful when symptoms present for <24hrs 10% recur Most within 24hours of reduction – observation Surgical reduction warranted when contrast enema unsuccessful 15% of patients require surgical intervention