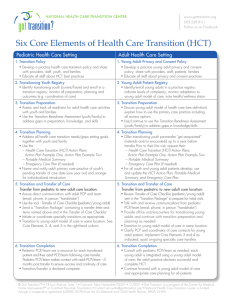
Six Core Elements of Health Care Transition
advertisement

Innovations in Pediatric to Adult Health Care for Clinicians and Health Systems SCTR Scientific Retreat February 8, 2016 Patience H White, MD, MA, FAAP, FACP Got Transition/Center for Health Care Transition Improvement Professor of Medicine and Pediatrics George Washington University School of Medicine and Health Sciences CENTER FOR HEALTH CARE TRANSITION IMPROVEMENT 1 Disclosures • I have no commercial relationships to disclose. CENTER FOR HEALTH CARE TRANSITION IMPROVEMENT 2 Presentation Learning Objectives 1. Identify the national case for pediatric to adult health care transition (HCT) improvements 2. Review the 6 core elements and tools for implementing the AAP/ACP/AAFP HCT Clinical Report 3. Discuss how to start a HCT quality improvement process 4. Review lessons learned from implementing HCT process from integrated delivery systems CENTER FOR HEALTH CARE TRANSITION IMPROVEMENT 3 Health Care Transition Goals • To improve the ability of youth and young adults to manage their own health and effectively use health services • To ensure an organized clinical process in pediatric and adult practices to facilitate transition preparation, transfer of care, and integration into adult-centered care CENTER FOR HEALTH CARE TRANSITION IMPROVEMENT 4 Got Transition/Center for Health Care Transition Improvement • Funded by federal Maternal and Child Health Bureau to: 1. Disseminate Health Care transition quality improvements 2. Provide education/training to health professionals 3. Expand youth/young adult and family engagement 4. Improve transition policy 5. Serve as a clearinghouse (www.GotTransition.org) CENTER FOR HEALTH CARE TRANSITION IMPROVEMENT 5 Making the Case for Transition Improvements* Health is diminished: • Youth often unable to name their health condition, relevant medical history, prescriptions, insurance source • Adherence to care is lower and medical complications are increased • Youth and families are worried Quality is compromised: • Youth, young adults, and families are dissatisfied about lack of preparation, information about adult care, vetted adult providers, communication between pediatric and adult providers, and sharing of medical information. • Discontinuity of care and lack of usual source of care are common • Surveys of health care providers consistently show they lack a systematic way to support youth, families, and young adults in transition Costs are increased: • Increased ER, hospital use, and duplicative tests result *Prior et. al. Pediatrics 134:1213 2014 CENTER FOR HEALTH CARE TRANSITION IMPROVEMENT 6 National Context for Transition • US youth 18 years of age • • There are est 4.5 million youth 18 years of age in the US*; 25% 12-17 year olds have a SHCN**, thus each year an est 1 million youth with SHCN will need transition support. National Organizations supporting transition • • • • • ACA: Transition an essential health home service, insurance expansions for young adults NCQA medical home standards on transition (plan of care, self-care support, transfer of medical records) Healthy People 2020 (discussion of transition planning with health care provider) Bureau of Maternal Child Health has transition as one of 13 national priorities CMS/CMMI focus on transition from hospital to home * 2010 Census **2011/2012 National Survey of Children's Health CENTER FOR HEALTH CARE TRANSITION IMPROVEMENT US and SC Transition Performance • National data – from 2009/10 – show that 60% of YSHCN are not receiving needed transition support: – Health care providers (HCP) discussed shift to adult provider – HCP encouraging youth to take responsibility for own health care needs – HCP discussed changing health needs as youth becomes adult – Discussed future insurance needs • SC – show that 59% are not receiving needed support – similar to US • However, these national findings overstate transition performance -- if perceived need was removed from the transition question, results would show that 90% of YSHCN are not receiving transition support. CENTER FOR HEALTH CARE TRANSITION IMPROVEMENT 8 CENTER FOR HEALTH CARE TRANSITION IMPROVEMENT California High Speed Rail Authority (Public Domain) State of Health Care Transition from Pediatric to Adult Health Care Approaches CENTER FOR HEALTH CARE TRANSITION IMPROVEMENT NOAA Historic Coast & Geodetic Survey Collection (Public Domain) AAP/AAFP/ACP Clinical Report on Health Care Transition* • In 2011, Clinical Report on Transition published as joint policy by AAP/AAFP/ACP • Targets all youth, beginning at age 12 • Algorithmic structure with: – Branching for youth with special health care needs – Application to primary and specialty practices • Extends through transfer of care to adult medical home and adult specialists Age 12 Youth and family aware of transition policy Age 14 Health care transition planning initiated Age 16 Preparation of youth and parents for adult approach to care and discussion of preferences and timing for transfer to adult health care Age 18 Transition to adult approach to care Age Transfer of care to adult medical home and 18-22 specialists with transfer package *Supporting the Health Care Transition from Adolescence to Adulthood in the Medical Home(Pediatrics, July 2011) CENTER FOR HEALTH CARE TRANSITION IMPROVEMENT Six Core Elements of Health Care Transition: QI Model • Original Six Core Elements (1.0), developed in 2011, as QI strategy based on AAP/AAFP/ACP Clinical Report with set of sample tools and transition index. • HCT Learning Collaboratives (with primary and specialty care practices) – Conducted between 2010-2012 in DC, Boston, Denver, New Hampshire, Minnesota, Wisconsin – Used well-tested Learning Collaborative methodology from the National Initiative for Children’s Healthcare Quality and pioneered by Institute for Healthcare Improvement – Demonstrated Six Core Elements and tools feasible to use in clinical settings and resulted in quality improvements in transition process* * McManus et al. Journal of Adol Health 56:73 2014 CENTER FOR HEALTH CARE TRANSITION IMPROVEMENT Updated Version of Six Core Element Tools Published in 2014 Based on learning collaboratives in DC, MA, NH, WI, MN Reviewed by over 100 clinical (primary and subspecialty providers, nurses, nurse practitioners, PAs and social workers) and consumer experts Represents state-of-the-art (process and tools) New Six Core Elements have three packages with expanded measurement options and tools for core element and can be used by all members of the health care team. 5th grade reading level, Spanish translation available CUSTOMIZABLE, USE YOUR OWN LOGOS FREE (download from www.gottransition.org) CENTER FOR HEALTH CARE TRANSITION IMPROVEMENT 13 Six Core Element Approach to Health Care Transition • Discuss Transition Policy AGES 14-15-1617-18 • Assess skills • Track progress AGES 14-15-1617-18 • Develop transition plan, including medical summary AGES 14-15-1617-18 AGE 12-14 • Transfer to adult – centered care • Integration into adult practice AGES 18-26 • Confirm transfer completion • Elicit consumer feedback • Ongoing Care AGES 18-21 1 2 3 4 5 6 Transition Policy Transition Tracking and Monitoring Transition Readiness Transition Planning Transfer/ Integration into AdultCentered Care Transition Completion/ Ongoing Care CENTER FOR HEALTH CARE TRANSITION IMPROVEMENT Six Core Elements 2.0 (See Side-by-Side Handout) Today I will offer mainly examples of tools from the “transitioning youth to an adult provider” package Transitioning Youth to Adult Health Care Providers (Pediatric, Family Medicine, and Med-Peds Providers) Transitioning to an Adult Approach to Health Care Without Changing Providers (Family Medicine and Med-Peds Providers) Integrating Young Adults into Adult Health Care (Internal Medicine, Family Medicine, and Med-Peds Providers) CENTER FOR HEALTH CARE TRANSITION IMPROVEMENT 15 CENTER FOR HEALTH CARE TRANSITION IMPROVEMENT CORE ELEMENT #1: POLICY • Purpose: Formalize practice’s approach, reduce clinician variability and offer a transparent approach to youth and families • Content: – Define practice approach and recommended ages for transition preparation for adult-focused care, transfer, and integration into adult care – Clarify adult approach to care and legal changes at age 18 – Reading level should be appropriate • Post: Communicate it to all involved early in the process CENTER FOR HEALTH CARE TRANSITION IMPROVEMENT 17 Element 1. Transition Policy • Make larger CENTER FOR HEALTH CARE TRANSITION IMPROVEMENT 18 CENTER FOR HEALTH CARE TRANSITION IMPROVEMENT Core Element #2: Transition Tracking and Monitoring • Purpose: Facilitate systematic data collection to improve quality at individual and population levels • Content: – Demographic and diagnostic/complexity data – Date of receipt of each core element (eg, policy shared, readiness assessment administered, etc.) • Format: paper check list, excel spread sheet, EHR CENTER FOR HEALTH CARE TRANSITION IMPROVEMENT 20 DE CENTER FOR HEALTH CARE TRANSITION IMPROVEMENT 21 CENTER FOR HEALTH CARE TRANSITION IMPROVEMENT 22 CENTER FOR HEALTH CARE TRANSITION IMPROVEMENT Core Element #3: Transition Readiness (Pediatric practice example) • Purpose: assess the youth’s skills to manage their health/health care in the adult approach to care and (selfcare skills assessment available in adult package) • Content: • Ranks importance of changing to adult provider before age 22 • Ranks confidence about ability of changing to adult provider • Assesses self-care skills related to own health and using health care services • Use: • • • • Completed several times during the transition process Used as a discussion tool to plan skill building education Does not predict transition success Customized to meet the needs of the practice’s population CENTER FOR HEALTH CARE TRANSITION IMPROVEMENT 24 CENTER FOR HEALTH CARE TRANSITION IMPROVEMENT 25 Core Element #3: Orientation to Adult Practice (Adult Practice Example) Purpose: Establish a process to welcome and orient new young adult patients into practice Content: • Identify adult providers in practice interested in caring for young adults • Acknowledge young adults as a distinct patient population • Clarify privacy, consent, and shared decision-making • Describe patient responsibilities • Describe services, hours, insurance info, costs (Share welcome letter/ adult office policy) CENTER FOR HEALTH CARE TRANSITION IMPROVEMENT 26 CENTER FOR HEALTH CARE TRANSITION IMPROVEMENT Core Element #4: Transition Planning (Pediatric Practice Example) • Purpose: Establish agreement between youth and provider about set of actions to address priorities and access current medical information • Content: – Identify what matters most to youth in becoming adult beyond health goals – Define how learning about health and health care supports youth’s over all goals (add readiness assessment skill needs to the plan) • Complete portable medical summary and emergency care plan with “special information” for adult provider – Include non medical information that the youth and family want to share and will assist the adult provider to engage the youth easily CENTER FOR HEALTH CARE TRANSITION IMPROVEMENT 28 CENTER FOR HEALTH CARE TRANSITION IMPROVEMENT 29 CENTER FOR HEALTH CARE TRANSITION IMPROVEMENT 30 CENTER FOR HEALTH CARE TRANSITION IMPROVEMENT 31 Facilitate Youth Knowledge of their Health Information • Majority of youth/young adults have a cell phone • Add health information to their phone (diagnosis, allergies, medications, who to contact in an emergency) ideally before the phone needs to be unlocked so EMS has access to it • Facilitates their ability to communicate key health information when needed • iPhone example: utilize Health App CENTER FOR HEALTH CARE TRANSITION IMPROVEMENT 32 Core Element #4: Integration into Adult Practice (Adult Practice Example) • Purpose: Establish systematic process for coordinating transfer with pediatric practice and obtaining current medical information • Content: – Communicate with pediatric provider and arrange consultation, if needed – Ensure receipt of transfer package and condition fact sheet, if needed – Office could make pre-visit reminder call and ask if special accommodations are needed – Identify community resources (eg. Decision support, support groups, insurance information) CENTER FOR HEALTH CARE TRANSITION IMPROVEMENT 33 CENTER FOR HEALTH CARE TRANSITION IMPROVEMENT Core Element #5: Transfer of Care (Pediatric Practice Example) • Purpose: Ensure completion and sharing of transfer package with adult provider and support engagement of young adult with a new provider • Content: – Transfer letter, clarifying coverage of youth’s care until initial adult visit with transfer package – Communicate directly with the adult provider, send transfer package with the last readiness assessment, plan of care, medical summary and emergency care plan, condition fact sheet, guardianship doc., and offer consultation. CENTER FOR HEALTH CARE TRANSITION IMPROVEMENT 35 Core Element #5: Initial Adult Visit (Adult Practice Example) • Purpose: Ensure a personalized, efficient, and consistent initial visit • Content: – Review of transfer package prior to visit – Address young adult’s concerns about confidentiality, and transfer, clarify adult approach to care and access to information, and preferred methods of communication – Discuss young adult’s health priorities as part of plan of care, review transition readiness assessment and/or complete self-care assessment, and update medical summary, emergency care plan and phone app CENTER FOR HEALTH CARE TRANSITION IMPROVEMENT 36 CENTER FOR HEALTH CARE TRANSITION IMPROVEMENT Core Element #6: Transfer Completion (Pediatric Package Example) • Purpose: Confirms initiation of the new adult provider and the ending of pediatric role, except as consultant • Content: – Communicate with adult practice confirming completion of transfer – Obtain consumer feedback anonymously after last pediatric visit (example feedback form at gottransition.org) CENTER FOR HEALTH CARE TRANSITION IMPROVEMENT 38 CENTER FOR HEALTH CARE TRANSITION IMPROVEMENT 39 Core Element #6: Ongoing Adult Care (Adult Practice Example) • Purpose: Ensure continuity of care and ongoing care management • Content: – Confirm with pediatric provider transfer of care responsibilities and obtain consultation, as needed – Identify needed adult specialists and assist with referrals to community resources – Provide ongoing care and periodically assessing self care skills – Elicit consumer feedback anonymously CENTER FOR HEALTH CARE TRANSITION IMPROVEMENT 40 Photo by Ovidiu Maris Used under Creative Commons License (CC BY-NC 2.0) Measurement Options CENTER FOR HEALTH CARE TRANSITION IMPROVEMENT Measurement Options 1 Initial Health Care Transition Assessment • Qualitative self-assessment tool modeled after index • Provides a snapshot of where practice initially is in implementing transition processes • Questions on consumer feedback and leadership CENTER FOR HEALTH CARE TRANSITION IMPROVEMENT Core Element #1: Policy CENTER FOR HEALTH CARE TRANSITION IMPROVEMENT 43 Measurement Options 2 Health Care Transition Process Measurement Tool • Objective scoring method with documentation requirements • Measures implementation of Six Core Elements, consumer feedback and leadership, and dissemination • Intended to be conducted at start of QI initiative as baseline measure and repeated to assess progress CENTER FOR HEALTH CARE TRANSITION IMPROVEMENT Measurement Tool: Policy Example CENTER FOR HEALTH CARE TRANSITION IMPROVEMENT What to do? Where to start? CENTER FOR HEALTH CARE TRANSITION IMPROVEMENT Photo: Jon Candy (CC BY-SA 2.0) Integrated Care Systems collaborating with Got Transition on HCT QI Cleveland Clinics Primary Care Henry Ford Health System (MI) Primary Care University of Rochester Specialty Care Walter Reed National Military Medical Center (MD) Specialty Care DC Managed Care CENTER FOR HEALTH CARE TRANSITION IMPROVEMENT Partnership in implementing and evaluating new Six Core Elements packages Pediatric and adult provider (includes Med-Peds and Family Medicine) teams participating Coaching support to networks by Got Transition Goal: to learn about dissemination of transition QI and ROI Starting a Transition Improvement Process (see available tip sheet at gottransition.org) • Developed with integrated health care systems implementing HCT QI with Six Core Elements • Steps to maximize success – Step 1: Secure senior leadership support – Step 2: Form transition improvement team eg both pediatric and adult providers/IT/payers/consumers – Step 3: Define transition processes for improvement eg. Articulate scope, population, strategies, time line, measures of success – Step 4: Dedicate time to implement transition improvements eg. This is hard work that takes dedicated time and leadership – Plus additional Tips for Success CENTER FOR HEALTH CARE TRANSITION IMPROVEMENT 48 A Subspecialty Transition Example: U. of Rochester (NY) • Department of Pediatrics identified transition as a top issue across all subspecialty divisions • Chair appointed “transition task force” to facilitate this process, led by Dr. Brett Robbins – Centered in division of adolescent medicine – Strong representation of combined Med-Peds trained faculty • Key stakeholders identified for committee – Enlisted the support of the Chair of Medicine – Access to division chief meetings in both IM and Peds – Chose 6 core elements as template for QI process CENTER FOR HEALTH CARE TRANSITION IMPROVEMENT 49 Subspecialty Transition • Pediatric and Internal Medicine divisions initially completed a baseline Current Assessment of Health Care Transition Activities that helped initiate the focus on HCT • Selected 3 pediatric-medicine subspecialty dyads based on interest and disease process – Endocrine (DM), Hematology (SS) , pulmonary (CF) – All 6 completed a baseline HCT Process Measurement Tool – All 6 selected 1-2 representatives (MD, SW, NP) • Monthly Meetings between ped and im division reps • QI process with many PDSA cycles • Goal of incorporating 6 core elements into clinical care process CENTER FOR HEALTH CARE TRANSITION IMPROVEMENT Subspecialty Transition Lessons Learned • Low level of baseline transition work or even awareness • Must have buy-in from Leadership chairs and division chiefs • Choose your pilot projects wisely, the rest of the system is watching • Most of day to day work in QI process done by SW, NP • Ped subspecialty had many misperceptions of IM • Peds had a very hard time letting go • IM not prepared to care for YA, but eager to learn • Need IT support, but don’t get lost in the computers • Moderator with credibility in both departments is very helpful • Policies and assessments come far easier than trust and implementation-next steps QI process for PC ACO CENTER FOR HEALTH CARE TRANSITION IMPROVEMENT Henry Ford Health System HCT Initiative Primary Care Example • Leadership engagement (started 18 months ago) – HCT focus provided HFHS a mechanism to support the shift in physician RVU targets to panel size targets-incentive to keep patients within the HFHS system • Pilot HCT Team – 4 PC practice sites (2 pediatric & 2 IM) – Completed Current Assessment HCT Activities at each site – Physicians, nurse supervisors, pediatrics administrator, patient partner, administrative fellow – Meet by phone monthly CENTER FOR HEALTH CARE TRANSITION IMPROVEMENT Henry Ford Health System HCT Initiative • Started with Healthcare Transition Webinar for pilot Team • Define goals/outcomes/timelines – HCT Policies created in Pediatrics, Internal Medicine and Family Medicine – Defined pilot population – Focused on the “low hanging fruit” for HCT process change (starting with older youth within peds, etc) CENTER FOR HEALTH CARE TRANSITION IMPROVEMENT Henry Ford Health System HCT Initiative • Utilize EMR After visit summary to disseminate HCT Policy PDSA cycles Feedback from providers, patients,& parent • MyChart Healthcare Skills Questionnaire customized and piloted • Next Steps: Developing Epic plan of care Survey of all HFHS adult providers on willingness to care for young adults with and without SHCN for future transfers, directory and welcome letters Stream line adult medicine primary care Epic referral process CENTER FOR HEALTH CARE TRANSITION IMPROVEMENT Current Assessment of Henry Ford Health System HCT Initiative Core Element Pediatric CAHCTA Level Initial/12 months Adult CAHCTA Level Initial/12 months Policy 1/3 1/3 Tracking 1/1 1/1 Readiness 1/3 1/1 Planning 1/2 1/1 Transfer 1/1 1/2 Completion 1/1 1/1 CENTER FOR HEALTH CARE TRANSITION IMPROVEMENT Lessons Learned • HCT fit into a larger strategic issue for HFHS • Motivation and the perceived need for structured HCT approach (tools and processes) differs between pediatric and adult providers: – Pediatrics leads initial work on HCT activities-understand need/urgency for HCT – Most adult providers less engaged in young adult care/find and focus on those interested from the beginning • Engaging the patient is a fundamental strategy for persuading reluctant team members • Perfection is the enemy of good, practice change is hard CENTER FOR HEALTH CARE TRANSITION IMPROVEMENT A Medicaid Managed Care Example: DC • Why are health plans interested in pediatric to adult transition? – Ensure continuity of care and improve self-care, particularly among those with chronic conditions – Retain young adults as health plan members – Improve satisfaction among young adults (often among the most dissatisfied health care consumers) – Comply with PCMH certification standards – Reduce unnecessary ED visits/hospitalization CENTER FOR HEALTH CARE TRANSITION IMPROVEMENT 57 Health Services for Children with Special Needs (HSCSN): A DC MCO • Serves 6,000 Medicaid enrollees from birth to age 26, all with SSI-eligible conditions • GT Analysis of HSCSN utilization data revealed: – A sizeable proportion of young adults over age 22 still being listed as being seen by pediatric providers. – Approximately two-thirds of 18-21 year olds with chronic conditions in the health plan and on the panels of pediatric PCPs will need to transfer to adult care in the next few years (before the age of 26). – A large proportion of young adults are not using their PCP, especially those with developmental disabilities, but using ER CENTER FOR HEALTH CARE TRANSITION IMPROVEMENT 57 Pilot Transition Intervention • Several senior leadership meetings to gain buy-in and health plan context • Meetings with senior nurse care management staff to review and customize each core element tool • Defined roles of HSCSN care managers, adult and pediatric provider practices • Designation of single nurse care manager and AmeriCorps volunteer to implement pilot project within health plan • Invitation and education of pediatric and adult practices (lunch & learn) • Invitation and active outreach to engage young adults • Piloted the customized 6 core element tools with small group of enrollees and pediatric and adult practices • Weekly updating, transition mentoring, and trouble-shooting calls with HSCSN and Got Transition staff throughout the project CENTER FOR HEALTH CARE TRANSITION IMPROVEMENT 59 • WHO: HSCSN Pilot Project – 35 HSCSN members (ages 18-25, SSI-eligible diagnostic groups: mental health, intellectual/developmental disability, and complex medical, Range of case management complexity levels) Practices: 3 pediatric and 1 adult site in DC • Results*: – 80% received 6 core elements in 6 months, 50% knew their medical needs, knew about privacy changes at age 18 and 80% reported needing to learn to call for their own doctor visits – Transfer of those 18 and older was difficult, primarily because YA not engaged in pediatric HC so out reach role of care manager was key – Using Got Transition’s Current Assessment of HCT: HSCSN plan scored at level 1 at start; 6 months later: level 3 for each core element. To get to level 4, dissemination would be required(next step). *McManus et al: JAHM 2015 CENTER FOR HEALTH CARE TRANSITION IMPROVEMENT 60 Lessons Learned • The Six Core Elements can be implemented/customized into a managed care plan’s processes and facilitates transition for their members • Transition process should begin before age 18, preferably around ages 1214, while the youth and family are regularly using their pediatric health services and engaged in their health • Young Adults hard to engage in health and going to an adult health care provider • Important to delineate roles of managed care staff and pediatric and adult health care providers, but SHARED role preferred by clinicians • Health Plan needs to proactively identify adult PCPs willing to treat young adults with mental health, ID/DD, and complex medical conditions; communicate these PCP choices to young adult members; and encourage adult practices to provide welcome information for their new young adult members • Managed care plans need to consider using financial incentives to gain more traction among providers CENTER FOR HEALTH CARE TRANSITION IMPROVEMENT 61 Summary of Primary, Specialty, and Managed Care Transition QI Examples • Feasible to adapt and implement Six Core Elements in primary, specialty and managed care • Starting with a pilot is important to test the processes before dissemination throughout the system • Engagement of system leadership and involvement of pediatric and adult provider leadership with broad based teams including consumers is key • Outline outcome and evaluation strategies upfront, plan the QI process so everyone is on board and knows what success looks like • Everyone is at the same starting point- Level 1 of the GT Measurement tool • Practice change takes time; HCT implementation takes more than writing a policy, doing a readiness assessment or putting tools into the EMR • Progress is rewarding and sustainable CENTER FOR HEALTH CARE TRANSITION IMPROVEMENT 62 Payment for Transition • Code 99240 now can be billed when a readiness assessment/self care assessment is completed by the youth. • See Coding and Reimbursement Tip Sheet for Transition • Developed by Got Transition with the AAP • Describes a set of innovative payment strategies • Provides a comprehensive list of CPT codes and Medicare values CENTER FOR HEALTH CARE TRANSITION IMPROVEMENT 63 Want more information? Got Transition: Federally funded resource center on HCT www.gottransition.org CENTER FOR HEALTH CARE TRANSITION IMPROVEMENT Thank You and Questions pwhite@thenationalalliance.org HealthCareTransition @GotTransition2 Visit www.GotTransition.org CENTER FOR HEALTH CARE TRANSITION IMPROVEMENT 65

![Starting a Transition Improvement Proces[...]](http://s3.studylib.net/store/data/006825099_1-d4c63a142fce04f55ecee809c05e88e0-300x300.png)