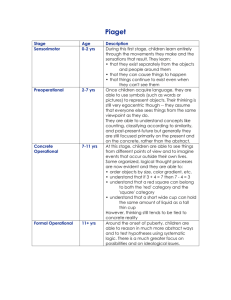
Demography,Incidence,Etiology,Presentation,Pathogenesis
advertisement
This lecture was conducted during the Nephrology Unit Grand Ground by Medical Student rotated under Nephrology Division under the supervision and administration of Prof. Jamal Al Wakeel, Head of Nephrology Unit, Department of Medicine and Dr. Abdulkareem Al Suwaida, Chairman of Department of Medicine. Nephrology Division is not responsible for the content of the presentation for it is intended for learning and /or education purpose only. The management of IgA nephropathy “ what was, what is and what will be “ Presented by: Dr. Abdullah Al-Mutairi Medical Student August 2008 Introduction Was first described by berger and hinglais in 1865 Soon became the most common primary GN Caused by glomerular IgA deposition Demography Onset in the second and third decades Male > female ( 2 : 1 ) More common in Whites and Asians Rare in blacks Incidence 20 – 40% in Japan and Australia 2 -10 % in USA and Canada High prevalence = routine screening for urinary abnormalities and low threshold for biopsy Low prevalence = in USA no biopsy is done for asymptomatic hematuria Etiology IgA deposition is found in association with many diseases ( 2ndy IgA nephropathy ) eg. Liver cirrhosis, celiac, HIV infection However, the cause primary IgA nephropathy is still unknown Presentation 40 -50 % present with gross hematuria (usually post URTI ) 30 – 40 % present with microscopic hematuria and Protienuria ( usually incidentally discovered ) Less than 10 % present with nephrotic syndrome or RPGN Pathogenesis 35 % of IgA nephropathy patients transplanted with new kidneys had recurrence Patients transplanted with kidneys from IgA nephropathy donors, showed disappearance of the deposits Therefore, IgA nephropathy is a systemic disease rather than a disease of the kidney alone Pathogenesis High IgA deposits does not it self cause the disease Rather, it is related to multiple palying factors, 1- Abnormal IgA immune complexes, polymeric IgA that are more likely to deposit in the mesangium ( galactosylation, sialation ) 2- Abnormal systemic immune response to antigens 3- Impaired clearance ( hepatic , mesangial clearance ) Pathogenesis Provocative factors; - Infections ( staph.aurues, CMV, Toxoplasma ) - Food antigen ( as in celiac ) These trigger the abnormal immune response, in the genetically predisposed patients leading to the production of the pathogenic IgA complexes in the bone marrow, which in turn deposit in the mesangium Pathogenesis Deposited IgA leads to ; IL-6 which switches on the inflammatory cascade C3 (local complement activation) - inflammation TGF – Beta – mesangial proliferation PDGF – Beta – mesangeal proliferation Histopathology Light microscopy, focal or diffuse mesangial proliferation other findings, segmental sclerosis/necrosis and crescents Electron microscopy, electron dense deposits within the mesangium Immunofluorescence, predominant IgA deposition ( Co-deposition of IgG,IgM,C3,lambda, and kappa light chains ) The management - 1 Approach to therapy Approach to Rx There is no cure However, measures to slow the progression are available . The treatment is based upon multiple factors that predicts progression to more severe disease Approach to Rx Clinical predictors of progression initial creatinine > 2.5 mg/dL ( 221 umol/L ) if 150umol/l ,ESRD >70% at 7yrs hypertension protein excretion 500 – 1000 mg/day ( 55%) indicates active and progressive disease thus, used for monitoring disease activity Approach to Rx Histologic predictors of progression glomerulosclerosis tubular atrophy interstitial fibrosis vascular disease crescents Approach to Rx Genetic predictors DD genotype of ACE gene upregulation of megsin gene The management - 2 Treatment Treatment General interventions ACE inhibitors / ARB’s Statins ?? Fish oil Immunosuppressive therapy Other interventions Corticosteroids Cyclophosphamide Cyclosporin, cellecept Tonsillectomy Low antigen diet IV immunoglobulins ACE inhibitors known to reduce proteinuria through its effect on The size-selective properties of the glomerular capillary wall. Clin Nephrol 200;54:360 As in other CKDs, it slows the progression of the reduction in GFR. Am J Kidney Dis 2006;47:751 ACE inhibitors Praga et al ( 44 pt, creatinine >133 umol/l, prot > 1.9 g/day) came to a conclusion in a randomized controlled trial that enalapril had better effect on renal survival ( 92 % ) and reduction in proteinuria in a six years follow-up when compared to other anti-hypertensives J Am Soc Nephrol 2003;14:1578 ACE inhibitors In HKVIN trial 109 patients were studied over 2 years, Protein 2g/day Few patients in the Valsartan group reached the primary end point ( doubling of creatinine or ESRD ) There was significant improvement in proteinuria ( 33% reduction ) and slower reduction in GFR ( 4.6 Vs 6.9 ml/min/yr ) as compared to placebo and other antihypertensives Am J Kidney Dis 2006;47:751 ACE inhibitors In the IgACE trial ( 65 patients over 38 months ) The primary end point ( > 30% decrease in renal function ) was reached by fewer patients in the Benazepril group Also lower incidence of secondary composite end point ( > 30% decrease in CR clearance or worsening of protienuria to reach nephrotic range ) Higher rate of partial or complete remission J Am Soc Nephrol 2007;18:1880 ACE/ARB combination The COOPERATE trial ( 263 patients, 60% IgAN ) combination versus monotherapy Trandolapril (3mg/day) and losartan Combination had better results in reduction in creatinine concentration + progression to ESRD (11% Vs 23% ) antiprotinuric effect (76% Vs 43% ) Lancet 2003;361:117 Fish oil ( omega-3 fatty acids ) Mechanism unknown, ?? Anti-inflammatory Evidence on benefit is conflicting Mayo clinic trial ( 106 patients , 12 g fish oil ) At 2 yrs - No difference in BP and protein excretion At 4 yrs – lower creatinine increase ( 6 Vs 33 % ) lower death or ESRD ( 10 Vs 40 % ) > 6 yrs – persisting benefit ( 15 Vs 37 % ) N Eng J Med 1994;331:1194. Fish oil ( omega-3 fatty acids ) A meta-analysis published in 1997 , concluded that fish has only minor benefit J Am Soc Nephrol 1997;8:1739. However, a pediatric study by Hogg et al. failed to show this benefit in more advanced disease Clin J Am Soc Nephrol 2006;1:467 Statins As CKD is CAD equivalent, then statins can be used to reduce risk circulation 2003;108:2154 Statins decreases loss of GFR in in mild to moderate CKD J Am Soc Nephrol 2006;17:2006 Target LDL is similar to that for IHD- < 100 mg/dl (2.5 mmol/l) J Am Soc Nephrol 2003;14:2556 Immunosuppressive therapy Steroids only Use of steroids from 6 -24 months decreases protein excretion and improves renal survival Clin Exp Nephrol 2004;8:237 Italian study ( 86 patients follow up for 5 and 10 yrs ) protein 3.5 g/day, creatinine 88.4 methylpred 1 g/day IV for the 3 days of minth 1,3 and 5 Combined with prednisolone 0.5 mg/kg/day on alternate days for 6 months Decreased primary end points ( doubling creatinine) 2 Vs 21% at 5 yrs 2 Vs 30 % at 10 yrs Lancet 1999;353:883 Steroids only However, the southwest pediatric group study, ( prednisolone Vs placebo ) showed no difference at 3 yrs, in reduction of GFR < 60 % of baseline Clin J Am Soc Nephrol 2006;1:467 So still unclear role, hence steroids are kept for diseases with proven active inflammation Clear benefit in acute nephrotic syndrome with histopath showing minimal change disease Am J Kid Dis 1989;14:361 Combined Rx This is only attempted for severe active disease or RPGN Studies showed possible benefit but these – did not compare with steroids alone were published prior to the widespread use of ACE Limited data Combined Rx Ballardie et al.( single center, controlled prospective trial of 38 pt ) patients = initial creatinine 130 – 250 umol/l that was increasing with rate of 15%/yr protein excretion 4- 4.5 g/day no crescents ( So severe or progressive disease ) Given = prednisolone 40mg/day tapered to 10mg/day by 2 yrs cyclophosphamide 1.5 mg/kg/day x 3months then azathioprine 1.5mg/kg/day x 2yrs Combined Rx Treatment group had decreased protein excretion in the 1st 6 months, ( 4.4g to 1.8g/day ) which persisted during 1yr follow up renal survival higher ( 82 Vs 68 % at 2 yrs ) ( 72 Vs 6 % at 5 yrs ) J Am Soc Nephrol 2002;13:142 Thus, patients with severe or progressive disease , without chronic renal damage on biopsy will benefit from combined immunosuppression Combined Rx Crescentric disease, tumlin et al. studied 12 patients mean creatinine 240 umol/l protein excretion 4g/day Given pulse methylpred 15mg/kg/day x 3days prednisolone 1mg/kg/day x 2months, then 0.6mg/kg/day x 2months, then 0.3 mg /kg/day x2months cyclophosphamide 0.5mg/m2 x 6months Combined Rx At end of the 6 months Creatinine improved ( 240 to 133 umol/l) Protein excretion reduced ( 4 to 1.4 g/day) renal Bx showed absence of crescents and proliferation With 3 yrs follow up ( prednisolon 0.15mg/kg/day + ACE) incidence of ESRD was lower ( 8 Vs 42 % in control ) Same results to other forms of crescentric GN However, still needs study Nephrol Dial Transplant 2003;18:1321 Other Immunosuppressive Rx Cyclosporine – small studies showed reduction in protein excretion but nephro-toxicity, increases creatinine > untreated relapse soon after stopping Rx Clin Nephrol 1991;35 Suppl 1:S43 Mycophenolate Mofetil ( MMF ) 4 small prospective, randomised trials with conflicting results still being studied Other Interventions Tonsillectomy tonsillitis associated with hematuria and proteinuria in IgAN so, thought to be the site of abnormal IgA fromation some retrospective reports showed improved renal survival Am J Kidney Dis 2001;38:736 Acta Otolaryngol Suppl 2004; 38 others showed no benefit Acta Otolaryngol Suppl 2004;32 Other Interventions Low antigen diet a diet free from gluten, dairy products, eggs and most meats proposed that some food antigens triggers the abnormal mucosal IgA system when this was applied in 1 study a dramatic reduction in protein excretion was noted renal Bx showed reduction in IgA and complement deposition and decreased cellularity Nephrol Dial Transplant 1993;8:1193 But still unconfirmed Other Interventions IV IG – It was observed that IgG is deficient in IgA nephropathy thus, predispose to infections leading to flare up of the disease Clin Exp Immunol 1989;75:30 Rostoker et al. studied 11 patients with high dose of IVIG ( 1g/kg 2 days/month x 3months, then im inj /2wks x6 months - Reduction in proteinuria ( 5.1 to 2.3 g/day ) - Improve GFR ( from rate of 3.8 ml/month loss to stable GFR ) - Decreased inflammation and IgA deposition on Bx Ann Intern Med 1994;120:476 Still need more studies Suggestions Suggestion Isolated hematuria, normal GFR - follow every 6 months treat if progress Persistant proteinuria > 500-1000mg/day treat with ACE inhibitors, goal protein excretion reduction by 60% from baseline if target not reached combine with ARBs Can use fish oil with ACE inhibitors Persistant nephrotic syndrome or CKD give statin Suggestions Acute onset nephrotic syndrome with minimal change dis and IgA deposition start steroids Progressive active dis ( hematuria, increasing proteinuria, and increasing creatinine) despite ACE /ARB start steroids alone - methylpred 1g x3days at month 1,3 and 5 with pred alternate days 0.5 mg/kg x 6 months then taper to stop - pred 2mg/kgevry other day x 2months then 0.5 mg/kg every other day x 4 months then taper to stop Suggestions Initially severe( creatinine > 133 umol/l) or progressive eventhough on steroids ( increasing creatinine or proteinuria ) with no chronic damage on Bx , then add cyclophosphamide pred 1mg/kg x3months then taper to 10mg/day x 2 yrs with cycloph 1.5 mg/kg orally x 3months then maintainance with either immuran 1.5 mg/kg or cellecept 1g BD tapering to 500mg BD x 2 yrs Suggestion Crescentric GN and RPGN use pulse steroids with cyclophos Methylpred 500-1g x 3days then pred 1mg/kg x 3months then taper to 10mg/day x 2 yrs With cyclophos 0.5 mg/m2 IV monthly x 3 months then maintainance with either immuran 1.5mg/kg or cellecept 1g bd tapering to 500mg bd X 2yrs Thanks