Open
advertisement
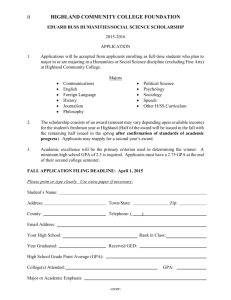
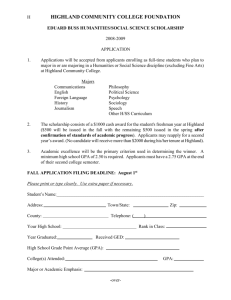
Presentation by Heidi May Board Nurse Director NHS Highland April 1st 2012 NHS Highland integrated with the Highland Council The Lead Agency model was used (not Body Corporate) NHS Highland leading on Adult Health and Social Care (including 17 Care Homes and Care At Home Services); the Highland Council leading on Community Children’s Services Employment of Children’s Services Health Visitors, some Learning Disability Nurses and AHPs transferred to the Council Social Workers, Contract Managers, Care Home staff, Care at Home staff, OTs transferred employment to NHS Highland Like most Boards NHS Highland has more than one Council in its Boundary Integration with Argyll and Bute Council will take place by 1st April 2016 Body Corporate Model being used NHS Highland = 41% landmass of Scotland (size of Denmark) 24 inhabited Islands 312,000 population 24 Hospitals Multiple Community Teams Two Councils IN Then a miracle occurs “Good work ……. but I think we need just a little more detail right here” JW99 OUT Corporate Visible approach Coal face to Professional identity & standards The Person boardroom Influencing Visioning Workforce Planning Human factor staff Communication Structures formal / informal Hardest thing?? What are we trying to achieve that we aren't currently doing What has to change “The Highland Partnership is committed to achieving the best possible outcomes for our population and service users. We believe that services should be person centred and enabling, should anticipate and prevent need as well as react to it, should be evidence based and acknowledge risk. We will improve the quality and reduce the cost of services through the creation of new, simpler, organisational arrangements that are designed to maximise outcomes and through the streamlining of service delivery to ensure it is faster, more efficient and more effective.” The Highland Council & NHS Highland 16 December 2010 Seamless care – health and social care Quality of Experience – right every time Opportunity to design/redesign care pathways – what adds value to the person Joint vision – Staff, People, Relatives, Carers, Residents Joint working – health, social care Single budget – everyone agrees what priorities are Performance management structure – what’s the impact on the person The will to improve! Single Point of Access Co-location Integrated Teams under one manager Virtual Ward Single Budget Fear of change/unknown Different organisational cultures Team Leader structures Maintaining clinical identity Reaching the decision makers Connecting decisions to the patient Who has accountability We don’t know what we don’t know • • • • • • • Stakeholder Events Staff workshops Issues Log Escalation Process Ward Forums Communication and Engagement Plan – Public events, newsletters, website, public notices, newspaper articles Elected and Board Members Briefing No Magic Bullet! Marathon – not a sprint Be visible Meet with staff Do visioning events with staff Use tools to bond the multidisciplinary Team ◦ CBAS ◦ Releasing Time to Care Capture the stories Address the logistical problems and concerns ◦ E.g. shared data bases Care Home standards (Care Inspectorate grading) have risen across the Board Care Standards Steering Group Dedicated Care Home staff e.g. falls prevention, food fluid and nutrition Reduction in length of stay in Care Homes Increased availability of Care at Home services Improved co-ordination, response and flexibility of multi disciplinary teams. Easier access to services through a single point of access Enhanced community care through Virtual Wards Improved satisfaction and quality of life Thank you Any Questions?