File
advertisement

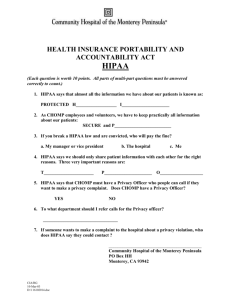
Chapter 5 Discussion Questions 2. Discuss the impacts of a breach to healthcare information systems, especially the financial and privacy impacts. According to Glandon, Smaltz & Slovensky (2008), protection of the privacy of health information is a major issue faced by all healthcare organizations. Protected health information, privacy and security must be made priority in healthcare. Despite the requirements in the Health Information Technology Act for Economic and Clinical Health (HITECH) Act of 2009 to provide stronger safeguards for patient data, healthcare organizations are still being found with data breaches incidents, which bring cost impact. According to a study by the Ponemon Institute in Traverse City, Michigan, data breaches cost the healthcare system an estimated $6 billion annually (DeGaspari, 2011). The study found that some healthcare organizations have inadequate resources to secure patient records or securing patient data is not their priority. The study also noted that the top three causes of breaches are unintentional employee action, lost or stolen computing devices and third-party snafu. “HIPAA has improved the state of data record security and has enabled better privacy practices” but it is believed that most organizations will not make the investment but instead they will look for ways to just barely meet the requirements (DeGaspari, 2001). 3. What is HIPAA? What are the potential benefits to healthcare organizations to be gained by compliance with HIPAA standards? What are the potential drawbacks? HIPAA stands for Health Insurance Portability and Accountability Act of 1996. HIPAA was enacted on August 21, 1996 to publicize standards for the electronic exchange, privacy and security of health information known as the Administrative Simplifications Provisions (www.hhs.gov/ocr). The U.S. Department of Health and Human Services (HHS) issued the Privacy Rule to implement the requirement of HIPAA. The standards address the use and disclosure of individuals’ health information – called protected health information as well as standards for individuals’ privacy rights to understand and control how their health information is used (p. 1). The rule permits important use of health information and at the same time protecting the privacy of people who are seeking care. Allowing the flow of information will provide and promote high quality healthcare (p. 1). Complying with the HIPAA standards comes with benefits for the healthcare organization. According to Glandon, Smaltz & Slovensky (2008), HIPAA improved quality by enhancing efficiency of electronic transmission through a standardized identifier called the National Provider Identifier (NPI) that uniquely identified the provider and payer source (p. 119). It also reduced paper consumption, increased coordination of insurance benefits and payments. Health care organizations are able to move away with health plan specific reporting and filing requirements and they are able to maintain patient’s personal health information in a secure and confidential manner (Bowers, 2001). One of the drawbacks of the Act for healthcare organizations is cost especially for larger organizations, as they had to hire extra staff, a dedicated privacy officer, to keep up with HIPAA requirements (www.finweb.com). There were costs associated with compliance. The federal mandate came about during the time healthcare organizations were experiencing reimbursement reduction due to the Balanced Budget Act. Healthcare organizations also believed that some elements of the privacy rules impeded their ability to treat patients (Bowers, 2001). 8. What concepts are important to information security policies and procedures? What effect does HIPAA have on healthcare organizations’ policies and procedures? Are there any other laws that may affect them? According to Glandon, Smaltz & Slovensky (2008), there are two essential elements that are important to security policies and procedures to maintain data security, privacy and confidentiality of information. First is protecting against system failures or external catastrophic events such as fires, storms, deliberate sabotage, and other acts of God; where critical information could be lost and second is controlling access to computer files by unauthorized personnel (p. 125-126). HIPAA forced healthcare organizations to review their policies and procedures related to data and information management. Development of comprehensive plans for security and policy revision were necessary. There was a need to review the organization’s confidentiality policy to cover necessary elements such as access rights, release of information, special handling of specific information, availability and integrity of medical information, and approved methods of information (p. 127). According to Ferrell (2001), HIPAA security rules resemble a collection of recommended best practices. If the healthcare organization has already adopted sound security practices, there will be no huge effort necessary to update policies and procedures. Another law that may affect healthcare organizations is the American Recovery and Reinvestment Act of 2009 (ARRA). The Act has provisions that affect health information management including technology adoption incentives and health information privacy. The privacy provision came about due to concerns over the confidentiality and transparency of electronic information. It relates as part of the HIPAA privacy rule to increase the protection of patient information and increase transparency of how information are used. (Rhodes, 2010). Also the requirements set forth by the Health Information Technology Act for Economic and Clinical Health Act of 2009 (HITECH) also may affect healthcare organizations. References Bowers, D. (2001). The health insurance portability and accountability act: is it really all that bad. PMC Journal. 14(4). Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1305898 DeGaspari, J. (2011). Data breaches cost healthcare system billions. Healthcare Informatics. Retrieved from http://www.healthcare-informatics.com/article/databreaches-cost-healthcare-system-billions Feller, T. (2001). Impact of HIPAA security rules on healthcare organizations. SANS Institute InfoSec Reading Room. Retrieved from http://www.sans.org/readingroom/whitepapers/policyissues/impact-hipaa-security-rules-healthcareorganizations4957 Financial Web. (nd). 5 disadvantages of HIPAA. Retrieved from http:// www.finweb.com/insurance/5-disadvantages-of-hipaa.html#axzz2gJ4BZM9u Glandon, G. L., Smaltz, D. H., & Slovensky, D. J. (2008). Austin and Boxerman’s information systems for healthcare management (7th ed.). Chicago, IL: Health Administration Press. Rhodes, H. (2010). HIPAA, too many ARRA privacy provisions amend HIPAA, not create new regulation. Journal of AHIMA 81(1). Retrieved from http://www.library.ahima.org