Hyperglycemia: Is
This Still a Concern?
Lauren E. Healy BA, PharmD, BCPS
NYSCHP Downstate Critical Care
Program
October 2, 2015
Conflicts of Interest
None to disclose
2
Learning Objectives
Explain the pathophysiology of hyperglycemia in
critically ill patients
Define the association between hyperglycemia
and clinical outcomes
Evaluate the recent literature on glycemic
control in critically ill patients
Specify glycemic targets for individual patient
populations
Compare the options for glycemic control
3
Stress Hyperglycemia
Blood glucose (BG) > 200 - 220 mg/dL in the
presence of an acute illness
Usually resolves with treatment of underlying
illness but can have lasting sequela
Donahey. Pharm Pract News. November 2013.
4
A Little History
1997
Malmberg and Colleagues of the Diabetes Mellitus
Insulin Glucose Infusion in Acute Myocardial Infarction
(DIGAMI) study group
Considered long-term, all cause mortality in patients with
Diabetes who were post-MI
Compared intensive insulin treatment (IIT) (126 – 180
mg/dL) vs. control
Mean (range) follow-up was 3.4 (1.6 – 5.6) years
102 (33%) deaths in the treatment arm and 138 (44%) in
the control arm (p = 0.011)
Malmberg. BMJ. 1997;314:1512.
5
Causes of Hyperglycemia in
Critically Ill Patients
External
Internal
Metabolic stress
Hormones
Cortisol,
catecholamines,
glucagon, growth
hormone
Insulin Resistance
Demonstrated in > 80%
of critically ill patients
Poor glucose control
Lack of pharmacologic
management
Medications
Glucocorticoids
Nutrition
TPN
Fluids
Donahey. Pharm Pract News. November 2013.
6
Effects of Hyperglycemia
Has been associated with poor clinical outcomes
Acute kidney injury (AKI)
Sepsis
Critical illness polyneuropathy (CIP)
Respiratory failure
Decreased wound healing
Increased mortality rates
Increased length of stay
Hospital and ICU
Donahey. Pharm Pract News. November 2013.
7
Van Den Berghe et al.
2001
Prospective, randomized, controlled study
IIT (80 – 110 mg/dL) versus conventional
treatment (180 – 200 mg/dL)
1548 Surgical patients enrolled
12 months
Van Den Berghe. N Engl J Med. 2001;345:1359 – 67.
8
Van Den Berghe et al.
Conventional
(180 – 200 mg/dL)
IIT
(80 – 110 mg/dL)
P-value
8.0 %
4.6 %
<0.04
Treatment with
antibiotics for >10d (%)
17.1 %
11.2 %
<0.001
Need for RRT (%)
8.2 %
4.8 %
0.007
EMG evidence of CIP
(on more than 2
occasions) (%)
18.9 %
7.0 %
0.001
Mortality during ICU
stay (%)
Van Den Berghe. N Engl J Med. 2001;345:1359 – 67.
9
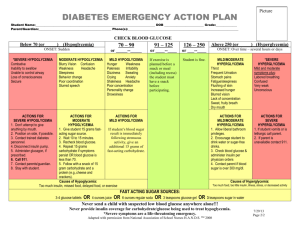
Effects of Moderate Intensity Glycemic
Control After Cardiac Surgery
Patients with Diabetes Mellitus or Random BG
>150 mg/dL post cardiac surgery
Targets
(mg/dL)
Glucose levels
(mg/dL)
Infection
rate (%)
Hypoglycemia
rate (%)
Control
(n = 207)
-
166 + 27
11
2.5
Intervention
(n = 410)
110 - 150
151 + 19
5
3.0
P - value
-
0.0001
0.018
1.0
Leibowitz. Ann Thorac Surg. 2010;90:1825-32.
10
Association Between Hyperglycemia
and Increased Hospital Mortality
Hospital Mortality (%)
Hospital Mortality vs. Mean BG
45
40
35
30
25
20
15
10
5
0
42.5
37.5
28.4
9.6
80 - 99
12.2
100 119
15.1
32.9
29.4
18.8
120 140 160 180 139
159
179
199
Mean BG (mg/dL)
200 249
250 299
>300
Heterogeneous ICU patient population
Krinsley. Mayo Clin Proc. 2003;78(12):1471-8.
11
Hyperglycemia and
Mortality Risk
Retrospective cohort
173 United States Veteran’s Health Administration
ICU’s
N = 259,040 admissions from 10/2002 – 9/2005
Hyperglycemia was associated with increased
hospital mortality independent of ICU type,
length of stay and diabetes
Mortality from hyperglycemia varied based on
admission diagnosis
Falciglia. Crit Care Med. 2009;37(12)3001-09.
12
Adjusted Odds of Hospital
Mortality Based on Hyperglycemia
Odds ratio w/ 95% CI
3.5
3
2.5
2
1.5
1
0.5
0
111-145
146-199
200-300
>300
Mean Glucose (mg/dL)
Falciglia. Crit Care Med. 2009;37(12)3001-09.
13
Admission Diagnosis Associated with
Hyperglycemia and Hospital Mortality
Acute Myocardial
Infarction
Stroke
Ischemic and Hemorrhagic
Arrhythmia
GI bleed
Unstable Angina
Acute Renal Failure
Pulmonary Embolism
Pneumonia
Congestive Heart Failure
Sepsis
Falciglia. Crit Care Med. 2009;37(12)3001-09.
14
Admission Diagnosis NOT Associated
with Hyperglycemia and Hospital
Mortality
Chronic Obstructive
Pulmonary Disease
Hepatic Failure
Gastrointestinal
Post Surgical
Coronary Artery Bypass
Graft
Peripheral Vascular Disease
Hip Fracture
Neoplasm
Falciglia. Crit Care Med. 2009;37(12)3001-09.
15
Audience Participation
Hyperglycemia has been shown to
increase the rates of:
A. Acute Kidney Injury
B. Infection
C. Critical Illness Polyneuropathy
D. Hospital Mortality
E. All of the above
16
We can’t ignore
hyperglycemia, so what do
we do about it?
17
Audience Participation
What BG goal is generally targeted in
the ICU’s at your institution?
A. 80 - 120 mg/dL
B. 120 - 140 mg/dL
C. 140 – 180 mg/dL
D. < 200 mg/dL
18
What do the Guidelines Say?
Organization
Target
(mg/dL)
Notes
Strength of
Recommendation
AACE/ADA
2009
140 – 180
> 110 mg/dL
*110 – 140 mg/dL
A
ACP
2011
140 - 200
SCCM
2012
100 – 150
Not 80 – 110 mg/dL •Weak
• Moderate quality
evidence
< 180 mg/dL
‘Very low quality of
evidence’
*In some Critically Ill patients – level of evidence C
1.
2.
3.
4.
Moghissi. Diab Care. 2009;32(6):1119–31.
Diab Care. 2012;35(1):S11-63.
Qaseem. Ann Intern Med. 2011;154:260-67.
Jacobi. Crit Care Med. 2012;40(12):3251-76.
19
Cardiology
Van Den Berghe et al – 2001
63% post cardiac surgery
Decreased mortality with BG 80 – 110 mg/dL compared
to 180 – 200 mg/dL (RRR 42%)
High risk for hypoglycemia
5.1 % vs. 0.8 % had BG < 40 mg/dL
Leibowitz et al - 2010
Post Cardiac Surgery
Intervention group targeted 110 – 150 mg/dL
Decreased infection rates from 11 % to 5 % (p = 0.018)
2.5% to 3% hypoglycemia (p = 1.0)
1.
2.
Van Den Berghe. N Engl J Med. 2001;345:1359 –
67.
Leibowitz. Ann Thorac Surg. 2010;90:1825-32.
20
Neurology
Treatment Hypoglycemia episodes ICU LOS
arms
(BG <80 mg/dL)
(days)
Bilotta
2008
N = 97
Post
severe
TBI
Bilotta N = 493
2009
Brain
surgery
6 month
survival (%)
80 – 120
mg/dL
15
10
10.4
< 220
mg/dL
7
7.3
12.2
P <0 .0001
P < 0.05
NS
80 – 110
mg/dL*
8
6
74
< 215
mg/dL*
3
8
72
P < 0.0001
P= .0001
NS
*Converted from mmol.
1. Bilotta. Neurocrit care. 2008;9(2):159-66.
2. Bilotta. Anesthesiology. 2009;110:611-9.
21
Medical patients
Surviving Sepsis guidelines - 2012
Target BG <180 mg/dL
Van Den Berghe - 2006
Prospective, randomized, controlled study in a
medical ICU
N = 1200, intention to treat
Overall hospital
mortality (%)
Hypoglycemia (%)
Conventional*
40
3.7
IIT (80 – 110 mg/dL)
37.3
18.7
*Started insulin infusion when BG > 215 mg/dL and titrated down when BG < 180 mg/dL
1. Crit Care Med. 2013;41(2):580-637.
2. Van Den Berghe. N Engl J Med. 2006;354:449-61.
22
Van Den Berghe – 2006
IIT
Reduced ICU length of stay
Hazard ratio (HR) 1.15 [1.01, 1.32], p = 0.04
Reduced hospital length of stay
HR 1.16 [1.00 1.35] p = 0.05
Reduced duration of mechanical ventilation
HR 1.21 [1.02, 1.44] p = 0.03
Less acute kidney failure
8.9 % to 5.9 %, p = 0.04
Decreased hospital mortality when treated > 3 days
52.5 % to 43.0 %, p = 0.009
But…
Increased rates of hypoglycemia
No mortality benefit
Different nutritional approach
Hard to identify patients > 3 days
Van Den Berghe. N Engl J Med. 2006;354:449-61.
23
COIITSS trial - 2010
Multicenter, randomized, 2x2 factorial, open-label trial
IIT (80 – 110 mg/dL) vs. conventional BG control (2004
surviving sepsis guidelines)
All patients with septic shock receiving corticosteroids
n = 509
No significant difference in In-hospital mortality or 90-
day mortality
Increased risk of hypoglycemia (BG <40 mg/dL)
72 vs. 44, p <0.001
The COIITSS Study Investigators. JAMA. 2010;303(4):341 – 348.
24
Mixed Medical/Surgical Patients
Volume Substitution and Insulin Therapy in Severe Sepsis
(VISEP) - 2008
Multicenter, 2x2 factorial trial
Compared IIT (80 – 110 mg/dL) to conventional (180 – 200
mg/dL)
The IIT arm was stopped early due to increased
hypoglycemia
IIT
Conventional
P – value
28 day mortality (%)
24.7
26.0
0.74
90 day mortality (%)
39.7
35.4
0.31
Hypoglycemia (%)
17
4.1
<0.001
25
Mixed Medical/Surgical Patients
NICE-SUGAR – 2009
IIT (81 – 108 mg/dL) vs. conventional (< 180
mg/dL)
N = 6104 patients in ICU
Increased mortality and hypoglycemia
BG goal
(mg/dL)
90-day
mortality (%)
Hypoglycemia rate
BG<40 mg/dL (%)
Surgical Subgroup 90
day mortality (%)
81 – 108
27.5
6.8
24.4
< 180
24.9
0.5
19.8
P - value
P = 0.02
P < 0.001
P = 0.10
NICE-SUGAR study investigators. N Engl J Med.2009;360:1283-97.
26
Glucotrol Study
2009, multicenter trial
Medical and surgical patients
IIT (80 – 110 mg/dL) vs. Conventional (140 – 180 mg/dL)
Trial stopped early due to protocol violations
IIT
Increased hypoglycemia (8.7 % vs. 2.7 %, p < 0.0001)
No difference in ICU mortality
Non-significant trend towards increased 28 day and
hospital mortality
18.7 % IIT vs. 15.3 % conventional
Preiser. Intensive Care Med. 2009;35:1738-48.
27
Blood Glucose Targets
Organization
Target
(mg/dL)
Notes
Strength of
Recommendation
AACE/ADA
2009
140 – 180
> 110 mg/dL
*110 – 140 mg/dL
A
ACP
2011
140 - 200
SCCM
2012
100 – 150
Not 80 – 110 mg/dL •Weak
• Moderate quality
evidence
< 180 mg/dL
‘Very low quality of
evidence’
Study
Control (mg/dL)
IIT (mg/dL)
Van Den Berghe 1, 2
180 +
80 - 110
NICE-SUGAR
< 180
80 - 110
VISEP
180 - 200
80 - 110
Glucotrol
180 - 200
80 - 110
28
Recurring Safety Concern is
Hypoglycemia…
29
Hypoglycemia
Moderate
BG < 70 mg/dL
Severe
BG < 40 mg/dL
Associated with increased morbidity and
mortality
Seizures
Brain damage
Depression
Cardiac arrhythmias
Donahey. Pharm Pract News. November 2013.
30
NICE-SUGAR
Post-Hoc analysis of 6026 patients
Patients with hypoglycemia had a higher risk of
death
Casual?
BG
Hazard Ratio
95% CI
P - value
41 – 70 mg/dL
1.41
1.21 – 1.62
< 0.001
< 40 mg/dL
2.10
1.59 – 2.77
< 0.001
The NICE-SUGAR Study Investigators. N Engl J Med. 2012;367:1108-18.
31
Risk Factors for and Outcomes of
Hypoglycemia
Retrospective, case-control analysis (1:3)
Define risk factors that increase the risk for severe
hypoglycemia (SH) (< 40 mg/dL)
Assess whether a single occurrence increases risk of
death
Results
N = 102 patients had SH out of 5,365 medical, surgical,
and cardiac admissions
Risk factors (next slide)
Mortality rates for SH group were 55.9 % compared to
39.5 % in control group (p = 0.057)
Krinsley. Crit Care Med. 2007;35(10):2262-67.
32
Risk Factors for Developing
Hypoglycemia
Risk Factor
Odds Ratio (95 % CI)
P value
Diabetes
3.07 (2.03 – 4.63)
< 0.0001
Septic Shock
2.03 (1.19 – 3.48)
0.0096
Mechanical
Ventilation
2.11 (1.28 – 3.48)
0.0032
Higher APACHE II
score
1.07 (1.05 – 1.10)
< 0.0001
Krinsley. Crit Care Med. 2007;35(10):2262-67.
33
Hypoglycemia and ICU Mortality
Hermanides et al. - 2010
Retrospective database cohort study in a medical/surgical
ICU; N = 5961
Increased risk for ICU death up to cutoff BG of 85 mg/dL
Hermanides. Crit Care Med. 2010;38(6):1430-34
34
Treating Hypoglycemia
If we can’t avoid it, and it causes harm…we
need to know how to treat it
Prevention
Decrease un – planned nutrition interruptions
Be careful with renal, and hepatic dysfunction
Early treatment and recognition
35
Treatment
Avoid hyperglycemia…
Avoid hypoglycemia…
How??
36
Decrease Glycemic Variability?
Egi et al. - 2006
Retrospective chart review of 7,049 critically ill patients
Average of 4.2 hourly glucose measurements
Mean + SD of BG
30 + 22 mg/dL in survivors and 40 + 27 mg/dL in non-
survivors
Mean and SD were significantly associated with both ICU
and hospital mortality (P < 0.001 for both)
Egi. Anesthesiology. 2006;105:244-52
37
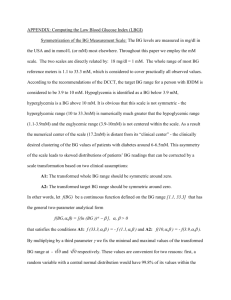
From: Variability of BG Concentration and Short-term Mortality in Critically Ill Patients
Anesthesiology. 2006;105(2):244-252.
38
Date of download: 9/16/2015
Copyright © 2015 American Society of Anesthesiologists. All rights reserved.
Glycemic Variability
2008 – Retrospective review of 3,252
medical/surgical patients
39
Krinsley JS. Crit Care Med. 2008 Nov;36(11):3008-13
A Hypoglycemia Protocol that
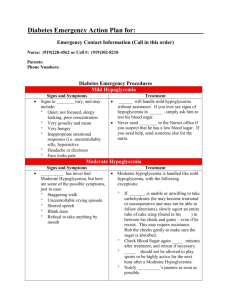
Minimizes Glycemic Variability?
2013 – Retrospective analysis
N = 772
Nursing driven hypoglycemia protocol
BG < 70 mg/dL give varying amounts of
dextrose 50 %
Less Glycemic variability (GV) than giving full 50
grams
BG rechecked every 15 minutes
BG (mg/dL)
< 15
Grams of D50W
25
15 - 25 26 - 35
20
17.5
Arnold. J Intensive Care Med. 2015;30(3):156-60.
36 - 45 46 - 60 60 - 70
12.5
10
7.5
40
Arnold et al. continued
Pre-Protocol
Post-Protocol
P-value
Coefficient of GV (%)
49.3
40.9
.048
Amount of D50W
(grams)
21.2*
11.5
<.001
Degree of BG
overcorrection (%)
86.3
54.5
.009
Time to repeat BG
(minutes)
61
36
.003
ICU mortality (%)
25
22.6
NS
*Pre-protocol patients generally received 12.5 or 25 grams of D50.
Arnold. J Intensive Care Med. 2015;30(3):156-60.
41
Easier Said Than Done…
Avoid hyperglycemia, hypoglycemia, and GV?
How?
Insulin
Intermittent subcutaneous
Intravenous continuous infusion
When?
Persistently elevated BG
> 2 readings >180 mg/dL
Jacobi. Crit Care Med. 2012;40(12):3251-76.
42
Insulin
Subcutaneous
Pros
Less time
“Set it and forget it”
More types/dosing options
Cons
Less adjustable
Who?
More stable patients
No nutrition interruptions
Continuous Infusion
Pros
Most Physiologic
Short half life
Easy titration
Cons
Increased workload
Who?
Hemodynamically
unstable
Edematous
Unpredictable nutrition
43
Intravenous Insulin Infusion
Protocols
Reach and maintain target BG quickly
Often a bolus is used
Monitor BG hourly initially
In range for 2 – 3 hours; monitor every 2 hours
Adjustment based on
Current BG
Rate of change
Result in minimal hypoglycemia
Jacobi. Crit Care Med. 2012;40(12):3251-76.
44
A Protocol Example
Braithwaite et al. described a tabular, dose-defining
protocol for intravenous insulin
Critically ill trauma service patients in surgical
intensive care unit
N = 27 runs
Mean pre-infusion BG was 230 + 67.9 mg/dL
BG < 140 mg/dL: 100% of the time; median time of 5
hours
BG < 110 mg/dL: 25/27 runs; median time of 11 hours
Hypoglycemia
< 70 mg/dL: 2.4 % of BG measurements
< 50 mg/dL: none
45
Braithwaite. Diab Technol Ther. 2006;8(4):476-88.
Transition to Subcutaneous
Insulin
When?
Consistent nutrition
Hemodynamically stable
Stable dose or no corticosteroids
Minimal peripheral edema
How?
Basal – bolus schedule
With corrective scale
Jacobi. Crit Care Med. 2012;40(12):3251-76.
46
Basal - Bolus
Based on continuous infusion requirements and
carbohydrate intake
80 % of past 24 hour infusion requirement
50 % Basal – long or intermediate acting insulin
50 % Bolus – short acting divided into three doses
‘pre-meal’ insulin
Continuous feeds
Basal (intermediate acting q6h)
Corrective scale
Overlap intravenous insulin and subcutaneous insulin
for 2 hours
Jacobi. Crit Care Med. 2012;40(12):3251-76.
47
How to Convert?
40 vs. 60 vs. 80% of 24 hour requirement?
Schmeltz et al.; N = 75
% of patients with capillary BG monitoring within 80 –
150 mg/dL during 24 hours after conversion
40 % - 58.7%
60% - 44.4%
80% - 67.6%
Hypoglycemia
< 50 mg/dL: 1 patient in 40 % group
< 70 mg/dL: 8 incidences (2% of total)
Schmeltz. Endoc Pract. 2006;12(6):641-649.
48
Patient Case
In the last 24 hours MM has required 30 units
of insulin via intravenous infusion. The team
wants to convert MM to subcutaneous
insulin therapy as her clinical status is
improving. What dose of basal/bolus would
you recommend in addition to a corrective
scale?
A. 15 basal and 5 bolus TID pre-meal
B. 12 basal and 12 bolus TID pre-meal
C. 12 basal and 5 bolus TID pre-meal
D. 12 basal and 4 bolus TID pre-meal
49
BG Monitoring
POC vs. Arterial sampling
Variability has been shown
Convenience
Time
Acceptable error varies
FDA – 20 %
ADA – 5 %
Clinical and Laboratory Standards Institute and
International Organization for Standardization
+15 mg/dL for BG < 75 mg/dL
20 % for BG > 75 mg/dL
Jacobi. Crit Care Med. 2012;40(12):3251-76.
50
BG Monitoring
POC meter variability
Low hematocrit
Glucose Oxidase based assay
Elevated PO2
Drugs
Uric acid
Billirubin
Glucose Dehydrogenase based assay
Maltose containing medications
Q1 - 2 hour testing…unrecognized hypoglycemia?
51
Continuous Glucose Monitoring
Can we decrease this workload?
Boom et al – 2014 in the Netherlands
N = 78 per group were analyzed
CGM
POC
P - value
Severe Hypoglycemia
detected by CGM
(<40 mg/dL*)
7(3/4)
0
-
Time BG in range
(90 – 160 mg/dL*) (%)
69
66
0.47
Nursing time (minutes)
17
36
<.001
Cost (Euros)
40.74
52.89
.02
*BG levels expressed in mmol in study and converted for purpose of presentation
Boom. Crit Care. 2014;18(4):453.
52
Audience Participation
Which of the following are used in the
ICU(s) at your hospital(s) to control
patients’ BG?
A. Continuous Glucose Monitoring
B. Insulin Infusion Protocol
C. Hypoglycemia Protocol
D. B and C
E. All of the above
53
In Summary
Yes, hyperglycemia is still a concern
Exact glycemic goal is still unknown
May depend on population
What we do know
Minimize hyperglycemia (BG > 180 mg/dL)
Minimize hypoglycemia (BG < 40 mg/dL)
Minimize GV
Monitor as closely as possible
Future studies
Define more specific BG goals
Compare GV to mean BG level
54
Hyperglycemia: Is
This Still a Concern?
Lauren E. Healy BA, PharmD, BCPS
NYSCHP Downstate: Critical Care
Program
October 2, 2015