Acute Visual Loss
advertisement

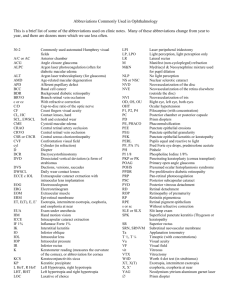
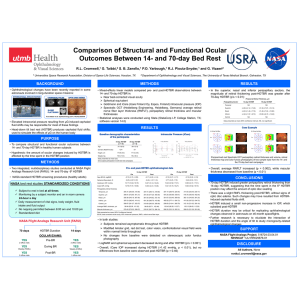
UBC Ophthalmology Interest Group Seminar Series 1.18.2012 ACUTE VISUAL LOSS ANATOMY REVIEW 24 mm Photo courtesy: Heather O’Donnell, PGY2, UBC PRIMARY CARE APPROACH History Onset ie. minutes vs days, following trauma? Transient vs permanent Mono vs binocular Associated symptoms eg. pain, swelling, floaters Other medical conditions and eye history Medications Eye Exam Visual acuity Equivalent to vitals for the eye VISUAL ACUITY TESTING Eye Exam Visual acuity Equivalent to vitals for the eye Pupils, RAPD Another ‘vitals’, from eye/neuro/trauma point of view Confrontational visual field Extraocular movement Tonometry External examination Slit lamp: lids, conjunctiva, AC Dilated examination, fundoscopy CASE 1 Previously well 75F presents to ED for sudden R eye pain and blurry vision while watching TV at night c/o “halo” around lights Symptoms not resolved Hx: cataract in both eye, mild HTN No medications CASE 1 OD CF, OS 20/25 R pupil fixed 4mm Rock hard globe Corneal edema Conj injections Opposite eye looks normal Nausea, vomit x 1 Photo courtesy: A. Doan, MD, University of Iowa IMPRESSION AND PLAN? A. Urgent head CT r/o mass lesion in brain causing high ICP B. Acute bacterial conjunctivitis, pt needs abx eye drops C. Chemical keratitis, rinse eye in sterile water for 10 min immediately D. Acute angle closure glaucoma, consult ophthalmology STAT ACUTE ANGLE CLOSURE GLAUCOMA Results from aqueous outflow obstruction by iris, rise in IOP, ischemia and permanent glaucomatous damage: emergency! IOP = 42 mmHg (normal 12-20mmHg) Acetazolamide and timolol were given initially, followed by pilocarpine 1 hour later. IOP decreased to 19 mmHg Laser peripheral iridotomy arranged the next day is the definitive treatment LASER PERIPHERAL IRIDOTOMY Photo courtesy: A. Doan, MD, University of Iowa CASE 2 50M highly myopic pt sees GP for c/o new onset of “flashing lights and floaters” Blurry vision but no pain Otherwise healthy Rev Ophthalmol, 2006, 6:15 CASE 2 OD 20/80, OS 20/20 Pupils, anterior segment normal Vitreous: tobacco dust IOP: OD 10 mmHg, OS 13 mmHg Rev Ophthalmol, 2006, 6:15 RETINAL DETACHMENT Rhegmatogenous most common, start as a tear, fluid build up beneath neuroretina separates it from retinal pigment epithelium High myopia is a risk factor In office: avoid pressure on globe, protect the eye Immediate ophthalmological consult required Surgery is definitive treatment, often urgent CASE 3 75F with sudden painless loss of vision OD yesterday comes to GP office A “grey spot” in her vision, grown over 10 min Hx incl. CAD, HTN, TIA Denies eye problems Photo courtesy: AAO 2011 CASE 3 OD CF, OS 20/30 R pupil sluggish 3mm RAPD EOM full Cornea, AC grossly normal IOP 10mmHg B/L Cranial nerves intact Photo courtesy: AAO 2011 MANAGEMENT A. Assure pt that her vision is unsalvageable, she needs to start Plavix to prevent a stroke B. Send pt to emergency department STAT C. Compress and release the eye right now D. You don’t know what this is, so you make a regular referral to ophthalmologist in 2-3 weeks CRAO Central retinal artery occlusion often secondary to embolus in a vasculopathic patient Ophthalmological emergency Immediate restoration of retinal blood flow is necessary to save sight Even with compress, sight is often not salvageable. Need to evaluate etiology CASE 4 85F comes to GP for sudden vision loss today 2 months of transient double vision She has been feeling fatigued with muscle and joint aches for the last 6 months New headache in her R temple particularly when she combs her hair Her jaw is painful when she’s eating BMJ 2011, 343d4783 CASE 4 OD LP, OS 20/40 R pupil 3mm RAPD EOM full VF: wide spread loss Anterior segment normal ESR from last week: 80 mm/h Dx: A. Temporal arteritis B. Amaurosis fugax C. Multiple sclerosis D. Compressive optic neuropathy NEXT STEP? A. Urgent neurology referral as stroke is imminent B. Start patient on high dose steroids empirically because benefits outweigh risks C. Ophthalmology referral for a temporal artery biopsy to confirm diagnosis D. Urgent MRI of brain as it’s most sensitive and specific for confirming a central lesion TEMPORAL ARTERITIS Aka giant cell arteritis. Another classic ophthalmological emergency Suspect in older women with new headache, vision loss, and systemic sx Elevated ESR/CRP helps to rule in dx Must initiate high dose steroids immediately followed by temporal artery biopsy SUMMARY Approach: Hx, Va, Pupils, out to in, front to back Acute vision loss is often a sign of serious ocular disease process: Acute angle closure glaucoma Retinal detachment Central retinal artery occlusion Temporal arteritis Urgent ophthalmological referral is needed (timeframe usually minutes to hours) Immediate action is also required; time is sight QUESTIONS ? Acknowledgement Case editor: Steven Schendel, PGY-4 UBC Contact R Tom Liu, UBC Med 2013 rztom.liu@gmail.com