Gastrectomy,Dumping Syndrome, Megaloblastic & Iron Deficiency
advertisement

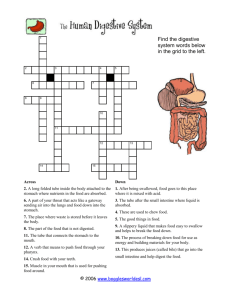
1 2 THE STOMACH, UNDER NORMAL PERFORMS THREE MAIN FUNCTIONS. CONDITIONS, Firstly, it acts as a place of STORAGE, so that 2 or 3 meals a day can provide all our energy needs. Secondly, it also aids the digestive process, as it is here that food is turned into a semi-liquid substance so that the nutrients can be absorbed from it. A third very important function of the stomach is the destruction of contaminants that the food may contain – bacteria and other micro-organisms. Very little is absorbed into the bloodstream straight through the stomach walls – aspirin and alcohol being exceptions to this rule. 3 The main functions of the stomach is to break down & digest food to extract nutrients from what you have eaten. It is necessary that the stomach, the digestive glands and the intestines must produce various enzymes, including pepsin, and acid. These acids and enzymes need to change the food into a semi-liquid form. The starch, fat and protein need to be broken down into smaller chemical units that can be absorbed into the bloodstream through the wall of the intestine. 4 The process of digestion starts in the mouth, where food is chewed and broken into smaller pieces. Saliva is mixed with the food, which makes it easier to move around in the Mouth. SALIVARY AMYLASE also starts to digest carbohydrates like sugar and starches. Once the food has been chewed, it is pushed by the tongue to the back of the mouth. From here, muscles move it further down the oesophagus and from there past a ONE-WAY VALVE, which is called the OESOPHAGEAL SPHINCTER. The muscles of the oesophagus are STRONG AND GRAVITY-DEFYING – one can swallow even if you are standing on your head or lying down. Once the food is in stomach, it is not supposed to move back up again, even lying down, or if the stomach contracts. 5 The amount of acid in stomach varies – it increases with food intake. The stomach itself is made of protein, and if not protected, will be consumed by the acid. The stomach and the duodenum are protected from the acid by a layer of mucus that stops the acid from consuming the stomach lining. Several factors, can lead to the malfunctioning of this protective layer of mucus,stomach and duodenal ulcers can result. The oesophagus does not have this protective layer, hence the feeling of heartburn if food pushes back up past the oesophageal sphincter. 6 After a few hours in the stomach, the liquidized food is pushed downward through another valve, called the PYLORUS, into the small intestine, so called because it is narrow and not short – it could be up to six metres long. Here chemicals are added to neutralise stomach acid: ◦ Enzymes from the pancreas ◦ bile from the liver are secreted to further the digestive process and to break down fats, carbohydrates and proteins. 7 Refers to erosion of the mucosa lining any portion of the G.I. tract. It is defined as : “A circumscribed ulceration of the gastrointestinal mucosa occurring in areas exposed to acid and pepsin and most often caused by Helicobacter pylori infection. (Uphold & Graham, 2003)” GASTRIC ULCER : the ulcer that occurs in the stomach lining ,some of them may be malignant DUODENAL ULCER : most often seen in first portion of duodenum (>95%) 8 9 Protective factors vs. hostile factors 10 A) Normal B) Increased Attack *Hyperacidity *Pepsin. *NSAIDs. C) Weak defense *Helicobacter pylori *Stress, *drugs *smoking 11 12 13 The causes of peptic ulcer disease include the following: Infection with the bacteria Helicobacter pylori occurs in 80 to 95% of patients with peptic ulcer disease. H. pylori infection impairs the protective mechanisms of the G.I. tract against low pH and digestive enzymes and leads to ulceration of the mucosa. Stress — Emotional, trauma, surgical. Injury or death of mucus-producing cells. Excess acid production in the stomach. The hormone gastrin stimulates the production of acid in the stomach; therefore, any factors that increase gastrin production will in turn increase the production of stomach acid. Drugs: Chronic use of aspirins and NSAIDs, or Corticosteroids 14 15 Most common infection in the world (20%) 10% of men, 4% women develop PUD Positive in 70-100% of PUD patients. H.pylori related disorders: Chronic gastritis – 90% Peptic ulcer disease – 95-100% Gastric carcinoma – 70% Gastric lymphoma Reflux Oesophagitis. Non ulcer dyspepsia 16 Gram negative, Spiral bacilli Spirochetes Do not invade cells – only mucous Gram negative, Spiral bacilli Breakdown urea - ammonia Break Spirochetes down mucosal defense Superficial inflammation Chronic Do not invade cells – only mucous Breakdown urea - ammonia Break down mucosal defense Chronic Superficial inflammation 17 duodenal sites are 4x as common common in late middle age. as gastric sites incidence increases with age. most common in middle age with Male to female ratio—2:1 peak 30-50 years Male to female ratio—4:1 More common with bl. group A Use of NSAIDs: associated with a Genetic link: 3x more common in three- to four-fold increase in risk of 1st degree relatives more common with blood group O gastric ulcer Less related to H. pylori than associated with increased serum duodenal ulcers : about 80% pepsinogen 10 - 20% of patients with a gastric H. pylori infection common,up to ulcer have a concomitant duodenal 95% ulcer smoking is twice as common 18 Manifestations of peptic ulcer disease: • Episodes of remission and exacerbation • Pain that for duodenal ulcers is often relieved by eating or antacids • G.I. bleeding and possible hemorrhage (20 to 25% of patients) • Perforation of ulcers with significant mortality • Obstruction of G.I. tract 19 Endoscopy Barium meal – contrast x-ray Biopsy – bacteria & malignancy H.Pylori: Endoscopy cytology Biopsy – Special stains Culture - difficult Urease Breath test. 20 1-Avoid spicy food. 2-Avoid xanthin containing beverges. 3-Avoid Alcohol. 4-Avoid Smoking. 5-Avoid heavy meals. 6-Encourage small frequent low caloric meals. 7-Avoid ulcerating drugs e.g. NSAIDs, corticosteroids, xanthines and parasympathomimetics 21 ◦ Proton Pump Inhibitor + clarithromycin and amoxicillin Omeprazole (Prilosec): 20 mg PO bid for 14 d or Lansoprazole (Prevacid): 30 mg PO bid for 14 d or Rabeprazole (Aciphex): 20 mg PO bid for 14 d or Esomeprazole (Nexium): 40 mg PO qd for 14 d plus Clarithromycin (Biaxin): 500 mg PO bid for 14 and Amoxicillin (Amoxil): 1 g PO bid for 14 d Can substitute Flagyl 500 mg PO bid for 14 d if allergic to Penicillin. ◦ In the setting of an active ulcer, continue on proton pump inhibitor therapy for additional 2 weeks. Goal: complete elimination of H. Pylori. Once achieved reinfection rates are low. 22 SURGICAL REMOVAL OF ALL OR PART OF THE STOMACH There are THREE MAIN TYPES of gastrectomy: ◦ PARTIAL GASTRECTOMY, removal of the lower half of the stomach ◦ FULL GASTRECTOMY, removal of the entire stomach ◦ SLEEVE GASTRECTOMY, removal of the left side of the stomach Removing the stomach doesn’t remove the body’s ability to digest liquids and foods. However, a few lifestyle changes after the procedure may be needed. 23 GASTRECTOMY IS PERFORMED MOST COMMONLY TO TREAT THE FOLLOWING CONDITIONS: ◦ STOMACH CANCER ◦ BLEEDING GASTRIC ULCER ◦ PERFORATION OF THE STOMACH WALL ◦ NONCANCEROUS POLYPS In severe duodenal ulcers it may be necessary to remove the lower portion of the stomach called the pylorus and the upper portion of the small intestine called the duodenum. 24 Bill Roth Procedure If there is a sufficient portion of the upper duodenum remaining a Bill Roth I procedure is performed, where the remaining portion of the stomach is reattached to the duodenum before the bile duct and the duct of the pancreas. If the stomach cannot be reattached to the duodenum a Bill Roth II is performed, where the remaining portion of the duodenum is sealed off, a hole is cut into the next section of the small intestine called the jejunum and the stomach is reattached at this hole. 25 The pylorus is used to grind food and slowly release the food into the small intestine, removal of the pylorus can cause food to move into the small intestine faster than normal, leading to gastric dumping syndrome. 26 The most obvious effect of the removal of the stomach is the loss of a storage place for food while it is being digested. Since only a small amount of food can be allowed into the small intestine at a time, the patient will have to eat small amounts of food regularly in order to prevent gastric dumping syndrome. 27 Another major effect is the LOSS OF THE INTRINSICFACTOR-SECRETING PARIETAL CELLS IN THE STOMACH LINING. Intrinsic factor is essential for the uptake of vitamin B12 in the terminal ileum and without it the patient will suffer from a vitamin B12 deficiency. This leads to a type of anaemia known as megalo blastic anaemia (can also be caused by folate deficiency, or autoimmune disease where it is specifically known as pernicious anaemia) which severely reduces red-blood cell synthesis (known as erythropoiesis, as well as other haematological cell lineages if severe enough but the red cell is the first to be affected). 28 Intrinsic factor is a glycoprotein secreted by parietal (humans) cells of the gastric mucosa. In humans, it has an important role in the absorption of vitamin B12 (cobalamin) in the intestine, and failure to produce or utilize intrinsic factor results in the condition Pernicious anaemia. Dietary vitamin B12 is released from ingested proteins in the stomach through the action of pepsin and acid. It is rapidly bound by one of two vitamin B12-binding proteins that are present in gastric juice; at acid pH, these binding proteins have a greater affinity for the vitamin than does intrinsic factor. In the small intestine, pancreatic proteases digest the binding proteins, releasing vitamin B12 which then becomes bound to intrinsic factor. Finally, there are receptors for intrinsic factor on the ileal mucosa which bind the complex, allowing vitamin B12 to be absorbed into portal blood. 29 Vitamin B12 In all mammals, vitamin B12 is necessary for maturation of erythrocytes, and a deficiency of this vitamin leads to development of anaemia. Since efficient absorption of vitamin B12 in humans depends on intrinsic factor, diseases which decrease the secretion of intrinsic factor (e.g. atrophic gastritis), interfere with cleavage of the binding proteins (e.g. pancreatic exocrine insufficiency) or decrease binding and absorption of the intrinsic factor-vitamin B12 complex (e.g. ileal disease or resection) can result in this type of anaemia. 30 Gastric dumping syndrome, or rapid gastric emptying is a condition: ◦ where ingested foods bypass the stomach too rapidly and enter the small intestine largely undigested. ◦ It happens when the small intestine expands too quickly due to the presence of hyperosmolar (having increased osmolarity) contents from the stomach. ◦ This causes symptoms due to the fluid shift into the gut lumen with plasma volume contraction and acute intestinal distension. 31 "EARLY" dumping begins concurrently within 15 to 30 minutes from ingestion of a meal. Symptoms of early dumping include nausea, vomiting, bloating, cramping, diarrhoea, dizziness, and fatigue. "Late" dumping happens one to three hours after eating. Symptoms of late dumping include weakness, sweating, and dizziness. Many people have both types. The syndrome is most often associated with gastric bypass (Roux-en-Y) surgery. 32 ◦ ◦ ◦ ◦ ◦ ◦ ◦ ◦ ◦ ◦ Nausea Vomiting Abdominal pain and cramping Diarrhoea Feeling uncomfortably full or bloated after a meal Sweating Weakness Dizziness flushing, or blushing of the face or skin rapid or irregular heartbeat 33 ◦ ◦ ◦ ◦ ◦ ◦ Hypo glycaemia Sweating Weakness Rapid or irregular heartbeat Flushing Dizziness 34 Dumping syndrome is caused by problems with the storage of food particles in the stomach and emptying of particles into the duodenum. Early dumping syndrome results from rapid movement of fluid into the intestine following a sudden addition of a large amount of food from the stomach. Late dumping syndrome results from rapid movement of sugar into the intestine, which raises the body's blood glucose level and causes the pancreas to increase its release of the hormone insulin. The increased release of insulin causes a rapid drop in blood glucose levels, a condition known as hypoglycaemia, or low blood sugar. 35 People who have had surgery to remove or bypass a significant part of the stomach are more likely to develop dumping syndrome. Some types of gastric surgery, such as bariatric surgery, reduce the size of the stomach. As a result, dietary nutrients pass quickly into the small intestine. Other conditions that impair how the stomach stores and empties itself of food, such as nerve damage caused by oesophageal surgery, can also cause dumping syndrome. 36 A health care provider will diagnose dumping syndrome primarily on the basis of symptoms. A scoring system helps differentiate dumping syndrome from other GI problems. The scoring system assigns points to each symptom and the total points result in a score. A person with a score above 7 likely has dumping syndrome. 37 A modified oral glucose tolerance test checks how well insulin works with tissues to absorb glucose. A health care provider performs the test during an office visit or in a commercial facility and sends the blood samples to a lab for analysis. The person should fast—eat or drink nothing except water—for at least 8 hours before the test. The health care provider will measure blood glucose concentration, haematocrit—the amount of red blood cells in the blood—pulse rate, and blood pressure before the test begins. After the initial measurements, the person drinks a glucose solution. The health care provider repeats the initial measurements immediately and at 30-minute intervals for up to 180 minutes. A health care provider often confirms dumping syndrome in people with ◦ LOW BLOOD SUGAR BETWEEN 120 AND 180 MINUTES AFTER DRINKING THE SOLUTION ◦ AN INCREASE IN HEMATOCRIT OF MORE THAN 3 PERCENT AT 30 MINUTES ◦ A RISE IN PULSE RATE OF MORE THAN 10 BEATS PER MINUTE AFTER 30 MINUTES 38 A gastric emptying scintigraphy test involves eating a bland meal—such as eggs or an egg substitute—that contains a small amount of radioactive material. A specially trained technician performs this test in a radiology center or hospital, and a radiologist—a doctor who specializes in medical imaging—interprets the results. Anaesthesia is not needed. An external camera scans the abdomen to locate the radioactive material. The radiologist measures the rate of gastric emptying at 1, 2, 3, and 4 hours after the meal. The test can help confirm a diagnosis of dumping syndrome. 39 Upper GI endoscopy involves using an endoscope—a small, flexible tube with a light—to see the upper GI tract. A gastroenterologist——performs the test . A small camera mounted on the endoscope transmits a video image to a monitor, allowing close examination of the intestinal lining. The test may show ulcers, swelling of the stomach lining, or cancer. An upper GI series examines the small intestine. An x-ray technician performs the test at a hospital or an outpatient center and a radiologist interprets the images. Anesthesia is not needed. No eating or drinking is allowed before the procedure. During the procedure, the person will stand or sit in front of an x-ray machine and drink barium, a chalky liquid. Barium coats the small intestine, making signs of a blockage or other complications of gastric surgery show up more clearly on x rays. 40 Treatment for dumping syndrome includes changes in eating, diet, and nutrition; medication; and, in some cases, surgery. EATING, DIET, AND NUTRITION The first step to minimizing symptoms of dumping syndrome involves changes in eating, diet, and nutrition, and may include eating five or six small meals a day instead of three larger meals delaying liquid intake until at least 30 minutes after a meal increasing intake of protein, fiber, and complex carbohydrates—found in starchy foods such as oatmeal and rice avoiding simple sugars such as table sugar, which can be found in candy, syrup, sodas, and juice beverages increasing the thickness of food by adding pectin or guar gum—plant extracts used as thickening agents .Some people find that lying down for 30 minutes after meals also helps reduce symptoms. 41 Octreotide acetate (Sandostatin) to treat dumping syndrome symptoms. The medication works by slowing gastric emptying and inhibiting the release of insulin and other GI hormones. Octreotide comes in short- and long-acting formulas. The shortacting formula is injected subcutaneously— under the skin—or intravenously—into a vein—two to four times a day. Complications of octreotide treatment include increased or decreased blood glucose levels, pain at the injection site, gallstones, and fatty, foul-smelling stools. 42 A person may need surgery if dumping syndrome is caused by previous gastric surgery or if the condition is not responsive to other treatments. For most people, the type of surgery depends on the type of gastric surgery performed previously. However, surgery to correct dumping syndrome often has unsuccessful results. 43 44