Genital-Urinary System
advertisement

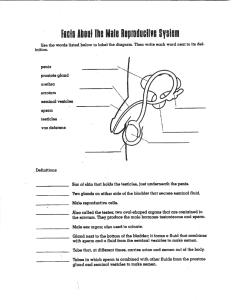
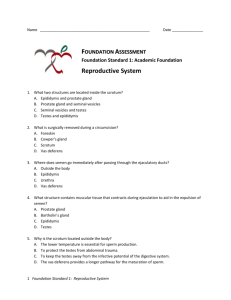
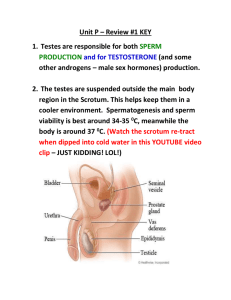
Genital-Urinary System Male Reproductive System Behavioral Objectives By the end of this lecture the student will be able to: • Review the anatomy and physiology of the genito-urinary systems • Describe the physical assessment of the GU systems • Discuss the application of the nursing process as it relates to patients with disorders of the GU system • Describe etiology, pathophysiology, clinical manifestations, nursing management and patient education for the following GU disorders: – – – – Prostatitis, Orchitis Prostaic hypertrophy Prostatic neoplasms • Discuss the nursing interventions in pre and post-operative care of patients undergoing the following GU system surgeries: – Prostatectomy Introduction – – Several organs are both urinary tract and reproductive system Disease of male reproductive system are usually treated by an urologist. Anatomy & Physiology • Brunner and Suddarth’s Medical Surgical Nursing – Volume 2 – Ch. 49 – pg 1739 - 1776 Testes • Descend into peritoneum in the last month of fetal life, – – – – • Paired Ovoid Smooth Firm – not soft Encased in the scrotum – i temp Spermatogenesis • What is Spermatogenesis? – Formation of Sperm • Spermatozoa – Immature sperm • Collecting tubules – Transmit the spermatozoa in the epididymis Testes • Testes have two functions • Formation of spermatozoa • Secretion of the male sex hormone testosterone Vas deferens (ductus deferens) • Tube – – upward abd. cavity downward base of the bladder Seminal vesicles • • • It acts as a reservoir for testicular secretions The tract is continued called the ejaculatory duct – Passes through the prostate gland and enters into the urethra Accessory glands • Prostate gland – Location: • • below the neck of the bladder Surrounds the urethra – Function: • Secrets chemicals to help spermatozoa Accessory glands • Cowper’s gland / bulbourethral gland – Location • Below the prostate – Function • Lubrication for sperm Penis • Dual function – Copulation – Urination • Urethra – Tube carries urine & semen – Opens at the tip of the glans Penis • The glans – Covered penile skin – foreskin – Retracted to expose the glans. • Circumcision – Foreskin removal Physical Assessment • Brunner and Suddarth’s Medical Surgical nursing pg 1742-1744 Health History Evaluate urinary & sexual function • Frequency • Force of stream, • “double” or “Triple” voiding • Dysuria • Hematuria • Hematospermia – • Medications – – – • Diuretics Psychotropic agents Anti-hypertensives Diagnosis – – • blood in the ejaculate semen/sperm DM HTN Smoking Physical Assessment Digital Rectal Examination (DRE) – – – > 40 yrs Annually Prostate gland • Size, shape and consistency Physical Assessment Testicular exam • Monthly (self) • Abnormalities & masses Physical Assessment Prostate Specific Antigen • h PSA level is = ?prostate Cancer? • h PSA Prostate pathology screen – – – – BPH Prostatitis Foley catheter DRE does not cause Increase in PSA Small group questions: 1. Describe the path a spermatozoa takes from formation to ejection 2. What are the male sex hormones and where are they formed? 3. What type of doctor would a man see if he is having sexual dysfunction? 4. While assessing the testes what would be normal findings? 4. What are the male accessory glands and what are their purposes? 5. Describe the purpose of a DRE, Testicular exam and PSA screen. How often should men have these screens done?