Epinephrine Administration by the EMT Training Module 2013
advertisement

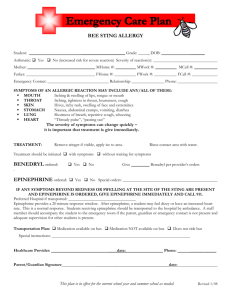
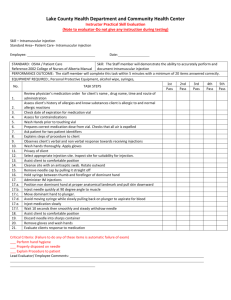
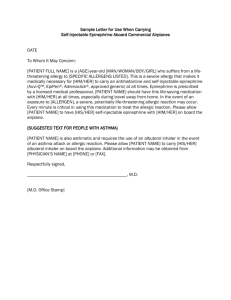
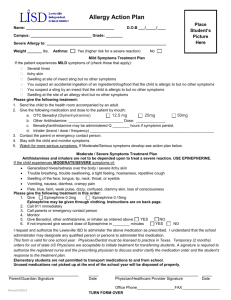
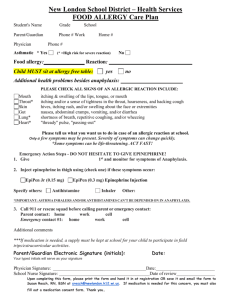
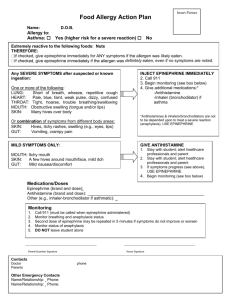
Epinephrine Administration by the EMT Training Module 2013 WVOEMS Approved Education MPCC addition of skill set and treatment options for EMT Protocol changes 02-01-2013 Learning Objectives With successful completion of this training module, the EMT will be able to describe and/or correctly demonstrate … • Epinephrine identification as a medication • Identify steps in aseptic technique • Preparation Epinephrine for administration • Administer Epinephrine via the IM route • Evaluate the mechanism of action and effects of Epinephrine EMT Utilization of Epinephrine • 6501-Allergic Reaction (Anaphylaxis) • 6302-Respiratory Distress (Bronchospasm) • In both protocols Epi can be given by an EMT with Medical Command contact • Auto-injectors may be utilized in both protocols as well as IM Injection Key Terms Anaphylaxis - a life-threatening, hypersensitivity reaction of the immune system Aseptic technique - a procedure performed under sterile conditions Asphyxia - suffocation as a result of blockage of the airway Dyspnea - labored or difficult breathing Epinephrine - a hormone released from the adrenal glands that activates several tissues in the “fight-or-flight” response Histamine - one of several chemical messages released from immune cells that promote inflammation as a defense mechanism Intramuscular - a medication route by injection into the belly of a muscle which encourages rapid transport by the bloodstream Shock - a severe reduction in blood pressure (by any cause) that results in inadequate blood flow (oxygen & glucose) to tissues What is Epinephrine… • A synthetic reproduction of the naturally occurring hormone Epinephrine • Released during “fight or flight” responses – reflex stimulation of the adrenal gland – sympathetic division of the autonomic nervous system What is Epinephrine • A catacholamine, sympathomimetic • Acts on cardiovascular system – Increases the strength of heart muscle contraction – Increases heart rate – Increases systolic blood pressure • Acts on respiratory system – Bronchodilation Actions of Epinephrine • • • • Relaxes smooth muscle in the airways Counteracts histamine and other cytokines Raises blood sugar level Raises heart rate, blood pressure, and myocardial oxygen demand For Intramuscular injection of Epinephrine… Onset of effect: 3-5 min Duration of effect: 1-4 hours Epinephrine Precautions • DO NOT give epinephrine to these patients: – ONLY hives, flushing or itching – Ongoing chest pain • Use caution (contact Medical Command) when giving epinephrine to patients with a history of heart attack, angina, or stroke Epinephrine Considerations • Give epinephrine with a clear history of insect bite or sting, or history of other allergy • MUST have at least one of the below signs and symptoms of severe allergic reaction – Respiratory Tract • Wheezing, Stridor, Shortness of Breath – Skin • Facial swelling involving lips, tongue, mouth (airway involvement) – Cardiovascular • Dizziness, HR>120, BP <90, AMS Epinephrine Onset • IM/SC, 5-15 minutes • Danger: – IV onset immediate, however at the 1:1000 concentration can cause arrhythmia and death – This is the reason for drawing back on syringe prior to injection to ensure you are not in a vessel Side Effects of Epinephrine • • • • • • • • • Palpitations Tachycardia & arrhythmias Hypertension Headache Tremor, weakness Pallor, sweating Nausea & vomiting Nervousness & anxiety Pain, redness at the injection site Medication Packaging • Name of medication • Concentration (1:1,000 or 1mg/1ml) • Expiration date Indications for Use EMTs may administer Epinephrine for: • Allergic Reaction/Anaphylaxis • Respiratory Distress/Bronchospasm Dosage • Epi Pen Auto Injector Dosage: Adults - 0.30 mg of 1:1,000 Pediatrics - 0.15 mg of 1:2,000 • IM Injection Drawn Up Dosage: Adults - 0.30 mg of 1:1,000 Pediatrics - 0.30 mg of 1:1,000 • Is 0.3 mg of Epi ever too much? • Can you really overdose a child? Special Considerations SPECIAL CONSIDERATIONS Assessment 1. Known or suspected exposure to allergen. Sting? If unclear contact base. 2. History of allergic reactions 3. Medication use prior to arrival. AnaGuard/Epi-pen, Benadryl? 4. PMH: heart disease, stroke, hypertension? 5. Medications: Beta-blockers (atenolol, propranolol)? May block effects of epinephrine 6. Vital signs including mental status 7. Respiratory status: Airway swelling? Wheezes? Stridor? Medication Issues Use epinephrine with caution in the following patients (contact base when possible but do not withhold if patient in severe distress and base contact cannot be made easily): Over 70 years of age History of heart disease, stroke or hypertension. Taking a beta-blocker (example: atenolol, propranolol) Transport Priorities: Any patient with signs or symptoms of a severe reaction requires immediate evacuation. Consider helicopter and/or rendezvous with higher level of care unless symptoms responding well to therapy. Anaphylaxis is an over-reaction of the Immune System • Sudden, severe allergic reaction involving the whole body (systemic) • multisystem involvement, including the skin, airway, vascular system, and GI • Most common allergens: insect sting, food, medication, latex • Widespread immune system response causes itching, hives & swelling • May also cause circulatory shock; tracheal and bronchial swelling resulting in asphyxia Allergic Reactions • Range from mild to life threatening • Early symptoms may be vague • Classic skin signs are urticaria, (hives) – Red, itchy raised welts anywhere on the body • Swelling of face, lips, eyes • Symptoms can occur seconds after exposure or up to 30 minutes Mild Reactions • Itching • Hives • Redness • Treatment is close observation and watching for progression of symptoms Severe Reactions • Respiratory Tract • Skin • Cardiovascular Respiratory Tract Signs and Symptoms • • • • • Wheezing Upper airway noisy breathing (stridor) Chest and throat tightness Shortness of Breath Nasal congestion* – *alone does not indicate a severe reaction Skin – Signs and Symptoms • Facial Swelling – Involving lips, tongue, mouth (airway involvement) • Redness* • Hives* • Itching* – *alone does not indicate a severe reaction Cardiovascular Signs and Symptoms • Decreased Blood Pressure (<90) • Increased Heart Rate (>120) • Severe Dizziness • Fainting • Decreased Mental Status – confusion, lethargy, coma EMT Treatment • Ensure an open airway • Administer oxygen • History and Physical • Vital signs • Epinephrine Intramuscular Drug Administration Intramuscular Drug Administration THE SIX “RIGHTS” 1. 2. 3. 4. 5. 6. Right person Right drug Right dose Right time Right route Right documentation Intramuscular Drug Administration Intramuscular sites allow a drug to be injected into the belly of a muscle so that the blood vessels supplying that muscle distribute the medication to its site of action via the bloodstream. First steps: 1. Prep the site with approved antiseptic by scrubbing vigorously and allowing to dry. DO NOT TOUCH, BLOW ON OR FAN THE INJECTION SITE! 2. Align the syringe and needle above the injection site at a 90 degree angle, with the bevel of the needle facing up. NOTE: IM Injections CANNOT be administered through clothing as the auto-injectors could. Intramuscular Drug Administration 90º Administration Sites Deltoid Dorsogluteal Ventrogluteal Vastus lateralis Needle Handling • Minimize the tasks performed in a moving ambulance. • Immediately dispose of used sharps in a sharps container. • NEVER recap needles. Ampules and Vials Store epinephrine AWAY from light; leave it in its carton until ready to use. Also keep away from extreme heat and danger of freezing. Ampules Vials Document all information concerning the patient and medication, including: 1. 2. 3. Indication for drug administration • include appearance, work of breathing, vitals, lung sounds, skin signs, and ability to speak Drug, dosage, and delivery site Patient response to the medication • include appearance, work of breathing, vitals, lung sounds, skin signs, and changes in ability to speak • both positive and negative responses Obtaining Medication from a Glass Ampule Common Packaging of Epinephrine • • • • Medication name Dosage (1:1,000 or 1mg/1ml) Expiration date Not cloudy; no color or precipitate Hold the ampule upright and tap its top to dislodge any trapped solution. Place Gauze around the neck Snap off the Top Draw up the Medication Using a 1cc syringe, insert the needle into the ampule and draw the plunger back on the syringe until you reach the correct dosage (0.30cc). Consideration WVOEMS does not require the use of a filtered needle when drawing from an ampule. Individual squads may have policies in place that require the use of a filtered needle. Please refer to your squad training officer. Obtaining Medication from a Vial Epinephrine in a Vial Medication name Dosage (1:1,000 or 1mg/1ml) Expiration date Not cloudy; no color or precipitate Prepare the syringe and hypodermic needle Clean the vial’s rubber top Insert the hypodermic needle into the rubber top and inject the air from the syringe into the vial. Withdraw the appropriate volume of medication Using a 1cc (ml) syringe, insert the needle into the vial or ampule, draw the plunger back on the syringe until you reach 0.3cc (ml) mark on the syringe. Administration • Prepare the site – – Vigorously rub an alcohol prep in a circular motion – Allow to air dry – Use your fingers to stretch skin and make it taut • Insert needle at a 90 degree angle • Draw back slightly to insure you have not cannulated a vessel. • Push slow and steady until medication is administered • Remove needle and cover puncture site • Dispose of needle properly Assessment of Medication Response Document patient’s response to treatment: • LOC, behavior, breathing effort, lung sounds, skin signs, vital signs, and changes in ability to speak • Document adverse effects, if any The body’s stress response causes the normal release of epinephrine to maintain homeostasis during vigorous activity: “fight or flight”. These same actions of epinephrine counteract e.g. the bronchoconstriction and low blood pressure of anaphylaxis when administered by medical personnel. Airway dilation Breathing rate increases Blood flow to skeletal muscles increases EPINEPHRINE Blood pressure increases Heart rate increases Pupils dilate Blood sugar level increases Document Vital Signs before and after treatment with Epinephrine Because epinephrine is expected to cause widespread changes in function, it is important to frequently monitor and document vital signs: • HR, RR, BP • include general appearance, work of breathing, lung sounds, skin signs, and ability to speak Always Wear PPE • Wear gloves and goggles when assessing the patient, preparing the medication, cleaning the site of injection, and administering the drug. Vastus lateralis (lateral thigh) is the approved site for administration Vastus lateralis (lateral thigh) is the approved site for administration • Good site for all ages • Far from major blood vessels & nerves • Medical Command may authorize other sites If no significant improvement within 10 minutes, consider second dose • If patient is wheezing consider, Albuterol nebulizer 2.5 mg with oxygen 8-10 LPM per order of MCP • Second dose of Epinephrine requires consultation and order of MCP. It is indicated if patient remains in moderate distress Equipment Size • Syringe – The EMT should chose a 1 cc (ml) syringe – DO NOT select a 1cc (ml) insulin syringe with a subcutaneous injection needle attached • Needle Size - Adult – Hypodermic needle 21 to 23 gauge – 1 to 1.5 inches long • Obese patients may require a 2 inch long needle • Needle Size - Pediatric – Hypodermic needle 25 to 27 gauge – 1 inch long EMT Epinephrine Administration Scope: Indications: Equipment: EMT Anaphylaxis (allergic reaction with respiratory distress); Bronchospasm Epinephrine kit containing:1, 1 ml ampule of epinephrine 1:1000, 1 tuberculin syringe with needle, alcohol prep Procedure: 1. Refer to Allergic Reactions and Respiratory Distress Protocols for detailed assessment. 2. Ask patient if they have any drug allergies. 3. Confirm medication, concentration, dose and clarity of liquid in vial 4. Tap ampule to get medicine down from top, break top off ampule with gauze 2x2, place top in sharps container. 5. Draw up 0.3cc (ml) of epinephrine 1mg/ml 1:1000, syringe approximately 1/3 full. 6. Pointing syringe up, expel all air. 7. Inform patient they are going to receive an injection, side effects may include feeling shaky or heart racing. 8. Select and cleanse area for Intramuscular injection, primary is the thigh unless directed otherwise by medical command. 9. Keeping the skin taut, insert needle at 90 degrees into administration site and draw back checking for blood return. If there is blood return, select a different site, and insert needle, again check for blood return. 10. If no blood, administer 0.3 cc (ml) of epinephrine (1/3 of syringe) for any patient. 11. Discard needle properly in sharps container. 12. Observe patient for improvement or deterioration of condition. Repeat exam and vitals after each dose. 13. Document procedure, vitals and response to treatment. 14. If an additional dose is required consult Allergic Reactions and Respiratory Distress Protocols. 15. If indicated by protocol, begin again from step 5. Potential Pitfalls • Dose Error – Drawing up epinephrine can potentially result in over or under dosing – Concentration error – (1:10,000) vs (1:1000) since both drugs are available – Administration error – epinephrine given IV instead of IM/SQ • Drug Error – Giving the correct dose of the wrong drug – Who stocks the EMT drugs? • Potential to stock the wrong drug Questions ?