Emergency Procedures
advertisement

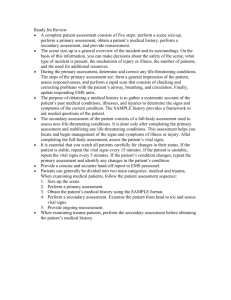
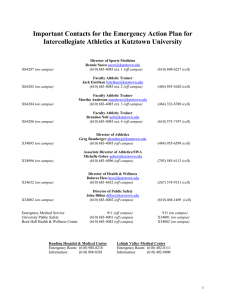
Plan your work….and work your plan! Describe the emergency plan Discuss the components of the emergency plan Define an emergency and provide examples of emergency situations Understand and explain a plan for handling emergency situations EMERGENCY Role of the certified athletic trainer 1. Evaluate the situation 2. Assess extent & seriousness of injury 3. Recognize life-threatening situations 4. Provide immediate emergency care 5. Initiate emergency procedures (plan) Emergency action plan • To provide care to athletes w/potentially life- altering or life-threatening injuries • To minimize the time needed to provide response to a medical emergency Development of an EAP Proper coverage of athletic events & practices Maintenance & upkeep of emergency supplies Selection of personnel for team Continuing education in emergency care Development & implementation of the EAP Personnel available Initial assessment & care Emergency communication Emergency equipment & supplies Venue locations Emergency transportation Location of emergency care facilities Legal need & documentation Developed by institutional personnel in consultation w/local emergency services Personnel Communication Documentation EAP Emergency facilities Venue location Equipment & supplies Transportation EAP implementation • Documentation of plan • Education of those involved • Frequent practice Venue specific copy of EAP by phone or other prominent location Team make-up varies depending on availability All should be first responders • First aid • CPR • AED • BBP Roles within the emergency team 1. Immediate care of the athlete 2. Emergency equipment retrieval 3. Activation of the EMS system 4. Direction of EMS to the scene CHECK • The scene for safety • The scene for evidence on the MOI • The patient for ABC’s, fractures & bleeding CALL • 911 or emergency mgt services • Give proper directions to site • Meet ambulance and direct to patient CARE • Calm and reassure injured athlete • Reassess & monitor all vital signs • Control any bleeding • Immobilize injured body part • Provide CPR/AED and first aid as needed Activate EMS • Make the call (911) • Identify yourself! Provide name, title and • • • • telephone number. Number of athletes involved in the emergency Suspected condition of the athlete(s) Treatment initiated and by who Specific directions to location (accessibility) Check communications before each practice or event Always have a back-up plan! Know location of working land line phone Post list of emergency numbers Include directions w/posted numbers On hand for all practices & events Know location & function Inventory annually Check periodically Equipment Supplies • AED unit • First aid kit • Immobilization splints • Sterile bandages • Stretcher/spine board • Tape and elastic wraps • Airway bag – valve • Bloodborne pathogens mask supplies (PPE) EAP is specific to each venue • Examples? Communicate to visiting team personnel • Personnel, communications, equipment Neutral sites??? By emergency personnel Availability of emergency services at high risk activities Communication strategy with on-site emergency personnel Required by risk management offices Should be a part of p/p manuals Should be posted in each venue Documentation: • Emergency information • Injury evaluation forms • Delineation of responsibility • Documentation on rehearsal of EAP • Equipment/supply inventory, purchases Evident & recognizable as lack of breathing or absence of pulse 1. Primary survey - ABC’s: ??? - determine responsiveness - determine needed actions - other conditions may cause condition to deteriorate slowly 2. Secondary survey - more detailed, hands-on, head to toe assessment - detect non-life-threatening conditions, left untreated could become serious State of consciousness - level of responsiveness - respond to your voice? - withdraw from painful stimuli? - totally unresponsive? Airway Breathing Circulation Vital signs 1. Pulse (HR) - normal adult rate - children - technique - irregularities Vital signs 2. Respiration (BR) - adult rate - children - technique - irregularities Vital signs 3. Blood pressure (BP) - definition - systolic pressure (normal) - diastolic pressure (normal) - irregular conditions : Systolic Blood Pressure (SBP) mm Hg Diastolic Blood Pressure (DBP) mm Hg Normal Prehypertension Stage I Hypertension <120 120–139 140–159 <80 80–89 90–99 Stage II Hypertension >160 >100 Other vital assessment areas 1. Skin color (3 for assessment) a. red b. blue c. white/pale 2. Pupils - sensitive to nervous system conditions - PEARRL - deviations from normal - constricted - unequal - dilated Decision making time 1. Seriousness of injury 2. First aid &/or immobilization necessary? 3. Immediate referral to MD? 4. Manner of transportation? Personnel Communiation Equipment Who’s in charge? (respect others) Access to areas? Ambulance coverage at high risk activities? Who calls the ambulance? Components • Emergency personnel • Emergency communication • Emergency equipment • Response plan Coverage based on sport/activity, setting, type of training/competition NCAA requirements for athletic personnel Requires team approach Roles of team • Care of the athlete • Equipment retrieval • EMS activation • Directing EMS to scene Access to phone? (check before every practice) Who makes the call? Review information All equipment should be at the site! Be familiar with equipment Equipment in good condition Readily available Plan same at all locations? Others aware of the plan? Others aware of their role? - coaches, equipment people, managers Work Your Plan Common Athletic Injuries - strains & sprains - overuse - neurological conditions Exam #2: Monday, October 26