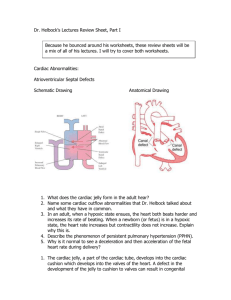
Ventricular Septal Defect
advertisement

Cardiovascular Stressors and Adaptation Common Cardiovascular Disorders in Children Congenital Heart Defects Congestive Heart Failure Acquired Heart Disease Review of Normal Circulation Fetal Shunts ductus venosus: accessory (extra) vein, carries oxygenated blood to fetal liver from umbilical vein foramen ovale: shunts oxygenated blood from right atrium to left atrium (hole in the atrial septum) ductus arteriosus: accessory (extra) artery, shunts deoxygenated blood away from lungs to descending aorta to umbilical cord to placenta Fetal Circulation of Oxygenated Blood Oxygenated blood flows from placenta into the umbilical vein to fetal liver through ductus venosus then inferior vena cava with the remaining unoxygenated blood from fetal legs & abdomen Fetal Circulation of Oxygenated Blood Inferior Vena cava empties into Right atrium Little oxygenated blood flows into right ventricle to be pumped through the pulmonary artery to the lungs (because the lungs are not inflating) Fetal Circulation of Oxygenated Blood Most of the oxygenated blood in the right atrium is shunted through the foramen ovale into the left atrium Then oxygenated blood travels from the left atrium, into the left ventricle, and pumped into the aorta to the body Fetal circulation of Deoxygenated blood Deoxygenated blood returns though the superior vena cava into the right atrium, right ventricle and into the pulmonary artery Because resistance is high in the pulmonary artery, blood flows through the opening in the pulmonary artery- the ductus arteriosus, into the aorta, into the fetal arterial system and into the 2 umbilical arteries back to the placenta How does the fetus receive sufficient oxygen from the maternal blood supply? Fetal hemoglobin carries 20-30% more oxygen than maternal hemoglobin Fetal hemoglobin concentration is 50% greater than mother’s Fetal heart rate 120-160bpm (increases cardiac output) What happens to the shunts after birth? Transition from intrauterine to extrauterine life Cord is clamped, neonate initiated respirations O2 levels rise = greater pressure in the left atrium, decreased pressure in the right atrium leading to an immediate closure of the foramen ovale Transition from intrauterine to extrauterine life After O2 circulates systemically, over 24 hours, the pressure in the left ventricle will become greater than the pulmonary artery and closes the ductus arterosis The absent flow of blood through the umbilicus gradually closes the ductus venosus over 12 hr to 2 weeks Cardiac Catheterization Primary method to measure extent of cardiac disease in children Shows type and severity of the CHD Insert tiny catheter through an artery in arm, leg or neck into the heart Take blood samples and measure pressure, measure o2 saturation, and as an intervention Sedation or anesthesia Outpatient vs Hospital Cardiac Catheterization Pre-Op NPO 4-6 hrs Check for known allergies, history of recent fever, signs and symptoms of infection Cardiac CatheterizationPost Op Monitor closely (cardiac monitor, continuous pulse ox) VS q 15 Assess dressing at insertion site for infection, hematoma Dressing must remain dry for 1st 4872 hrs No blood drawn from extremity used Palpate a pulse distal to the dressing to assure blood flow to extremity is not obstructed: keep extremity straight for 48 hrs after procedure Congestive Heart Failure heart doesn’t pump blood well enough –can not provide adequate cardiac output due to impaired myocardial contractility Causes in children: • Defects • Acquired heart disease • Infections Congestive Heart Failure Most common cause in children is congenital heart defects • Increased volume load or increased pressure in heart Excess volume and pressure builds up in lungs leading to labored breathing builds up in rest of body leading to edema (edema is a late sign in children) Congestive Heart Failure Symptoms 1st sign: tachycardia tire easily rapid, labored breathing decreased urine output fluid and sodium are retained increased sweating, pallor edema CHF Diagnosis and Treatment CXR- shows enlargement Echocardiogram- dilated heart vessels, hypertrophy, increase in heart size Tx-aimed at reducing volume overload, improve contractility May require surgery Congestive Heart Failure Medical Management 1. Digoxin- Helps strengthen the heart muscle, enables it to pump more efficiently 1st line tx Dosing depends on wt and age Need HR, EKG, drug levels Parent teaching 2. ACE (Angiotension-converting-enzyme) inhibitors- dilates the blood vessels making it easier for the heart to pump blood forward into the body Congestive Heart Failure Medical Management Diuretics- Helps the kidneys remove excess fluid from the body • Potassium sparing • Potassium wasting • Potassium supplements- given along with wasting diuretics Lasix-1st agent for children-lose K esp. when taken with digoxin Congenital Heart Disease 35 different types Common to have multiple defects Range from mild to life threatening and fatal Genetic and environmental causes Caused by: • Defect or • Failure of shunt closure Normal Blood Flow Pressure in left is higher than right side Types of CHD Acynotic defects • Septal defects • VSD • ASD • PDA Obstructive (Cyanotic) defects Cyanotic defects • Pulmonic Stenosis • Coarctation of the aorta • Transposition of the greater vessels • Tetrology of Fallot • Hypoplastic left heart Septal Defects- increased pulmonary blood flow Left to right shunting (acyanotic defect) • Increased cardiac workload • Excessive pulmonary blood flow • Right ventricular strain, dilation, hypertrophy • CHF, pulmonary HTN, bacterial endocarditis • Ventral Septal Defect • Atrial Septal Defect Ventricular Septal Defect Most common CHD High Pressure in LV forces blood back to RV Results in increased pulmonary blood flow (heart must pump extra blood), higher than normal artery pressure Ventricular Septal Defect S/S: vary with the size of the defect 4-8 weeks of age develop loud, harsh systolic heart murmur Right ventricular hypertrophy 20-60% close spontaneously cardiac cath shows: O2 level of RV higher than normal large defects: develop CHF, poor feeding, failure to thrive Ventricular Septal Defect Treatment: Small defects: followed by cardiologist, prophylactic ABX Large defect: open heart surgery with cardiopulmonary bypass, will suture or patch hole closed • If child is not stable for open heart surgery: pulmonary artery banding: narrowing of pulmonary artery to VSD Medical Management For infants not medically stable for surgery or awaiting surgeryDigoxin: to improve cardiac output; check apical pulse first, don’t give if HR < 100 bmp in infants and < 70 bpm in children Digoxin toxicity: vomiting, bradycardia Oxygen Atrial Septal Defect Pressure in LA is greater than RA (blood flows left to right) Oxygen rich blood leaks back to RA to RV and is then pumped back to lungs, results in ventricular hypertrophy Few if any symptoms, over time may experience fatigue and dyspnea on exertion Atrial Septal Defect Clinical Presentation Large defect may cause CHF Harsh systolic murmur Second heart sound is split: “fixed splitting” ** diagnostic of ASD pulmonary valve closes later than aortic valve Echocardiogram: shows enlarged right side of heart, increased pulmonary circulation ASD Management Nonsurgical management: prosthetic umbrella patch Surgical management: open-heart with CP bypass, edges are sutured or will use Silastic patch to cover hole Diuretics to control symptoms until repair is performed Patent Ductus Arteriosus Failure of ductus arteriosus to close completely at birth Blood from the aorta flows into the pulmonary arteries to be reoxygenated in the lungs, returns to LA and LV Not enough oxygenated blood is getting out o nourish the body More common in preemies Patent Ductus Arteriosus Preterm infants: present with CHF and respiratory distress Fullterm infants: may be asymptomatic with a continuous “machinery” type murmur Tire easily, growth retardation (shorter, weigh less, less muscle mass), prone to frequent respiratory tract infections Patent Ductus Arteriosus Chest radiographs (x-ray) show enlarged LA and LV Medical management: Indomethacin (prostaglandin inhibitor that stimulates ductus to constrict) Surgical management: ductus is divided and ligated (usually performed in first year of life to decrease risk of bacterial endocarditis Obstructive Defectsdecreased pulmonary blood flow Right to left shunt Defect present that obstructs LV flow Pulmonic Stenosis Coarctation of the Aorta Pulmonary Stenosis Obstruction of the right ventricular outflow tract Decreased pulmonary blood flow Right ventricular hypertrophy High ventricular pressure may cause blood to back up into right atrium and force foramen ovale to open to allow blood to flow from right to left atrium Pulmonary Stenosis Usually asymptomatic Systolic ejection murmur with a palpable thrill Enlarged heart on x-ray Severe: right ventricular failure, CHF, if there is right to left shunting through the foramen ovale, mild to moderate cyanosis Pulmonary Stenosis Medical Management: If asymptomatic: cardiac follow-up Prophylactic ABX Surgical Management: Pulmonary balloon valvuloplasty via cardiac cath if unsuccessful: valvotomy Coarctation of Aorta Localized constriction of the aorta at or near the insertion site of the ductus arteriosus Reduces cardiac output (impedes blood flow from heart to body) Aortic pressure is high proximal to the constriction and low distal to the constriction Coarctation of Aorta S/S: related to severity of the constriction and presence of associated cardiac defects Mild: asymptomatic, sys. murmur, diminished pulses in lower ext Severe: poor lower body perfusion, metabolic acidosis, CHF, systemic hypertension In both: BP is 20mmHg higher in arms than in lower extremities Coarctation of Aorta Diagnosis-clinical exam, echo Treatment is based on severity Treatment of Coarctation of Aorta Symptomatic newborn treated with: Digoxin diuretics to manage CHF may also receive PGE1 (prostaglandin) infusions to maintain ductal patency and improves perfusion to lower extremities surgical repair within first 2 years Cynaotic Defects Decreased pulmonary blood flow • Transposition of the greater vessels • Tetrology of Fallot • Hypoplastic left heart Tetralogy of Fallot Consists of 4 Parts: VSD RV hypertrophy Overriding aorta Pulmonic Stenosis: impedes blood flow to the lungs, forces unoxygenated blood through the VSD & into aorta S/STetralogy of Fallot The degree of pulmonic stenosis governs the onset and severity of symptoms. Mild: little to no right to left shunting infant has “tet spells” hypercyanotic episodes Mod-severe: some cyanotic at birth when PDA closes, other infants become increasingly cyanotic over the first few months of life Tetralogy of Fallot Tire easily especially with exertion, difficulty feeding and gaining weight, Other signs: chronic hypoxemia Management Tetralogy of Fallot Over time may have hypercyanotic episodes (tet spells) often preceded by crying, feeding or stooling, worsening cyanosis, increased respiratory rate, may lose consciousness Treatment of tet spells: calm infant, knee-chest position, O2 Do not leave alone- cyanosis can cause LOC, death Tetralogy of Fallot Medical management: Symptomatic newborn: PGE1 infusion to maintain ductal patency Older infants: close monitoring for worsening of hypoxia Surgical management: done at 3-12 months of age, in stages primary open-heart repair: close VSD, open pulmonary valve, remove obstructing muscle Hypoplastic Left Heart Syndrome pulmonary venous blood is shunted through foramen ovale into right atrium mixed blood travels through the right ventricle to the pulmonary artery, patent ductus arteriosus as ductus begins to close in first few days of life infant becomes symptomatic Hypoplastic Left Heart Syndrome symptoms: CHF hypoperfusion, shock grayish-blue color dyspnea hypotension Diagnosis Clinical presentation and echo (increased size in right side) Hypoplastic Left Heart Syndrome Medical Management: PGE1 to keep ductus arteriosus open Correct acid-base and electrolyte imbalances Surgical management: Heart transplant Three-stage repair Transposition of Great Arteries Aorta is connected to RV (unoxygenated blood goes to body) Pulmonary artery is attached to LV (oxygen rich blood is recirculated to lungs) Survival depends on mixing these two circulations through the fetal structures (foramen ovale and ductus arteriosus) Transposition of Great Arteries Cyanosis apparent at birth or shortly after, no response to oxygen Prompt diagnosis and treatment needed for survival Arterial switch procedure: redirects blood flow, may be done in stages within 1st year Caring for the Child with a Congenital Heart Defect Nursing Care: taking infant home before corrective surgery Provide parents with information about care Review steps for follow-up care, emergency management (s/s respiratory distress, CPR) Key: promote normalcy within the limits of the child’s condition Caring for the Child with a Congenital Heart Defect Preoperative:undergoing corrective surgery Explain procedures to parents and child, assure understanding Encourage child and parents to express fears Prepare child for surgery and postop, show models of equipment (chest tube) Caring for the Child with a Congenital Heart Defect Postoperative: Monitor cardiac output Support respiratory function Maintain fluid and electrolyte balance Promote comfort (IV morphine, sedatives) Promote healing and recovery Acquired Heart Diseae HTN Endocarditis Rheumatic Fever Kawasaki Disease Hypertension Primary HTN • Caused by increased body mass • Genetics Secondary HTN • Cause is from an underlying condition such as kidney disease or heart defects Hypertension No set systolic and diastolic number for diagnosis Need to compare to child’s age, gender and height If 3 different readings are above the 95th percentile for that child then diagnosis is confirmed Hypertension Managed by eliminating the primary cause if possible • Exercise, life style modification ACE inhibitors ARBs Beta-Blockers Ca Channel Blockers Infective Endocarditis Inflammation of the lining of the valves and arteries Caused by bacterial and fungal infections in the blood stream that infects an already existing injured endocardium Children at risk: cardiac defects, severe valve disorders Infective Endocarditis Symptoms: • Fever, fatigue, headache, N/V, new or changed murmur, CHF, dyspnea Treatment: • Antibiotics IV for 2-8 weeks, surgery to replace valves, treatment of CHF Rheumatic Fever Acute RF is leading cause of acquired heart disease (but has decreased in US b/c abx) Inflammatory autoimmune condition Seen in children age 5-15 Usually follows untreated strep A infection (pharyngitis) Causes scarring of the mitral valves Rheumatic Fever S/S: Polyarthritis Carditis Chorea Erythema marginatum Subcutaneous nodules Rheumatic Fever Diagnosis- clinical symptoms and +ASO titer Rheumatic Fever Management: Treat infection Treat other symptoms Streptococcal prophylaxis • PCN IM every month or • PCN PO BID (if allergic Sulfadiazine PO QD) Kawasaki Disease Acquired heart disease in children under age 5 Boys>girls Asian decent Multisystem vasculitis (inflammation of blood vessels) 3 stages of illness Affects the coronary arteries Occurs due to antibody vascular injury post infection Kawasaki Disease first stage day 1-14 Prolonged fever Bilateral, nonpurulent conjunctivitis Changes in mouth (erythema, fissures, crusting of lips, strawberry tongue) Induration of hands and feet Erythema of palms and soles Erythemous rash Enlarged cervical lymph nodes Kawasaki Disease second stage day 15-25 Fever and most of the previous symptoms resolve Extreme irritability develops Anorexia Lip cracking and fissuring Desquamation of fingers and toes Arthritis Vascular changes in myocardium and coronary arteries Kawasaki Disease Third phase- day 26-40 Lasts until erythrocyte sed rate returns to normal and all symptoms disappear Beau’s lines may appear Management Prevent or reduce coronary artery damage Gamma-globulin IV in a dosage of 2gm/kg over a 12h infusion High dose aspirin therapy at same time (80-100mg/kg/day once daily), continued through weeks 6-8 of disease Kawasaki Disease Nursing care: Administer meds Comfort measures Hydration Parental support A parent of a toddler with Kawaski’s disease tells the nurse “I just don’t know what to do with my child. He’s never acted like this before.” The nurses best reply is: 1. 2. 3. 4. Don’t worry. This type of behavior is typical for a toddler Irritability is part of Kawasaki’s disease. Please don’t be embarrassed Perhaps your child would benefit from stricter limits You seem to be in need of a referral to our Child Guidance Center When assessing a child for signs and symptoms of rheumatic fever, which symptoms should the nurse anticipate? 1. 2. 3. 4. Tachycardia and joint pain Bradycardia and swollen joints Loss of coordination and pruritic rash Bradycardia and fever Which nursing intervention is most effective in preventing rheumatic fever in children? 1. 2. 3. 4. Refer children with sore throats for a throat culture Include an ECG in the child’s yearly physical examination Assess the child for a change in the quality of the pulse Assess the child’s blood pressure Which is most beneficial in achieving the goal of preventing infection in a child with cardiac disease? 1. 2. 3. 4. Give the child extra immunizations Keep the child on daily prophylactic antibiotics Keep the child away from others who are ill Place the child in protective isolation A newborn with patent ductus arteriousus is scheduled to receive indomethacin. The nurse administers this medication to: 1. 2. 3. 4. Open the ductus arteriosus Close the ductus arteriosus Enlarge the ductus arteriosus Maintain the size of the ductus arteriosus Which congenital heart defect necessitates that the nurse take upper and lower extremity blood pressure readings? 1. Coarctation of the aorta 2. Tetralogy of Fallot 3. Ventricular septal defect 4. Patent ductus arteriosus An infant with ventricular septal defect develops congestive heart failure and is placed on digoxin therapy twice a day. The infant vomits the morning dose of digoxin. The most appropriate nursing intervention is to: 1. 2. 3. 4. Notify the pediatrician as soon as possible Take the infant’s pulse for 1 minute and repeat the dose of digoxin Skip the dose and give twice the amount at the next dose Repeat the dose and chart that the infant vomited the first dose The parents of a newborn with ventricular septal defect ask why their baby is being sent home instead of undergoing immediate open heart surgery. The nurse’s best response is: 1. 2. 3. 4. Your baby’s condition is too serious for immediate open heart surgery Ventricular septal defects are not repaired until the infant is older Your baby has a small defect, and we hope that is closes spontaneously Your baby must be fully immunized before surgery When reviewing the chart of an infant with tetralogy of Fallot, the nurse should anticipate which laboratory findings? 1. Anemia 2. Polycythemia 3. Increased white blood cell count 4. Decreased hematocrit An infant with tetralogy of Fallot becomes hypoxic following a prolonged bout of crying. The nurse’s first action should be to: 1. Administer oxygen 2. Administer morphine 3. Place the infant in the knee-chest position 4. Comfort the infant