- Integration of Psychiatry into Primary Health Care
advertisement
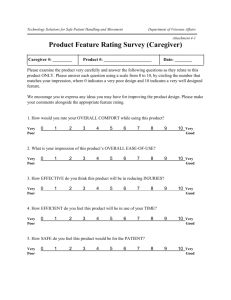
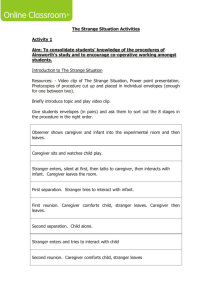
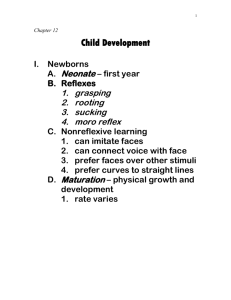
When the bough breaks: Mental Illness in the Pregnant and Postpartum Woman Dr.Mariam Alawadhi MD,FRCPC Assistant professor-Department of Psychiatry,Kuwait University Head of consultation liaison unit-KCMH Agenda Review the epidemiology and clinical presentation of perinatal mood and anxiety disorders in perinatal women. Understand the psychiatric, obstetric and pediatric implications of a mother’s untreated illness. Discuss a bio-psychosocial approach to the management of these disorders. Depression is “the most common complication of childbearing.” Wisner, 2002 1 in 5 mothers will experience a mental health disorder during their pregnancy or the year after they deliver. Pregnancy and the transition to parenthood is considered to be one of life's major transitions. Women are at an increased risk of developing mental health issues due to physiological and psychological risk factors. Challenging the myths... Media images of pregnancy and motherhood Pregnancy was planned, so why do I have the “blues”? Work-life balance Relationships (couple, extended family) ...and facing reality Tired, home alone, lots of care for baby, no time for self, complete loss of control over time Wide range of positive and negative emotions Adjustment and adaptation to pregnancy and motherhood is dynamic pregnancy alters a woman’s life irreversibly Women need accurate information (e.g, pregnancy, labour, delivery) = power, control Shame & stigma Perinatal mental health Pregnancy related Antepartum Depression Antepartum anxiety Postpartum related Baby Blues Postpartum Depression Postpartum Psychosis postpartum anxiety Let’s define the terms first... Antepartum depression Antepartum depression Depression vs. pregnancy? affect cognition functional impairment Associated with: Poor prenatal care (e.g., nutrition; substance use) Changes in cortisol & HPA axis development Poor perinatal outcomes (e.g, abnormal fetal neurobehavioral; pre-term labour (Steele et al., 1992) Antenatal Depression Risk factors: low self-esteem low social support, low income antenatal anxiety, hx of depression, hx of abuse negative cognitive style hx of miscarriage/pregnancy termination pregnancy complications Confounds in diagnosing depression during pregnancy Overlapping symptoms: Sleep disturbances Increased/decreased appetite Decreased energy Changes in concentration Illnesses with similar symptoms: Anemia Thyroid dysfunction Gestational diabetes mellitus Perinatal Anxiety Generalized Anxiety Disorder = 4-8% Panic Attacks = 1-3% Obsessive Compulsive Disorder = 0.2-1.2% Posttraumatic stress Disorder = 6%; 40% in loss Perinatal anxiety disorders Effects of maternal stress & anxiety during pregnancy – Altered fetal movement – Lower gestational age – Lower infant birth weight – Lower APGAR scores – Enduring changes in cortisol measures in offspring Postpartum blues Low-level symptoms: • Baby blues – Very common (50-80%) – Starts w/in 1 wk pp: peaks • Tearfulness • Irritability, reactivity • Insomnia • Anxiety • Poor appetite 3-5 days post-delivery – Unrelated to environmental stressors – Unrelated to psychiatric history – Present in all cultures Posited relationship between “Blues” and PPD • During pregnancy: – Increase oestrogen, progesterone (placental production of hormones); beta-endorphin & cortisol (cortisol peaks in late pregnancy CRH), prolactin – Oestrogen enhances neurotransmitter serotonin (increases synthesis & reduced breakdown) • After delivery: – Drop in oestrogen/progesterone (removal of placenta at delivery); drop in cortisol & b/e – Decrease estrogen decrease serotonin – Prolactin levels return to normal in non-lactating women w/in weeks – Breastfeeding: prolactin levels remain high (induces release of oxytocin) Postpartum depression Postpartum depression DSM IV onset from within 4 wks. of delivery, “pp onset” Clinically, up to 1 y postpartum (DSM V to reflect this) Peaks at 3-6 mo pp Average PPD course is 7 mo Related to psychiatric history and environmental stressors Postpartum depression Added clinical features: Obsessive traits (e.g., name of baby, harming baby) Depressed, despondent, emotionally numb Ambivalence toward baby (bonding) Grief for loss of self Feelings of inadequacy, guilt* Feeling isolated/misunderstood Suicidal ideation/Ego-dystonic thoughts of harming baby Biological history of depression or affective disorders •Previous PPD or depression •Low self-esteem •Lack/poor •Perfectionist, dysfunction •Hormones •Feelings •Relationship problems (couple, extended family) •Difficult baby (feeding, colic) •Separation function •Role •Stressful •Sleep •Attitude immune toward pregnancy (ambivalence, unwanted) (Kendler, 1993; Wisner, 2002) disturbances conflict •Trauma/abuse •Unresolved grief (death of child) from baby live events (move, job change, illness) •Economic •Recent Obstetric •IVF (fertility drugs) •Difficult of inadequacy •Altered social support •age neuroticism, high/unrealistic expectations of self/baby •Thyroid Social stress loss •Childcare stress (# of children at home) Risk factors •Family Psychological delivery •Medical complications of pregnancy •Health problems of infant •Lack of readiness for hospital discharge Postpartum psychosis Heterogeneous group of disorders BAD (35% with bipolar diathesis) MDD w/ psychotic features SZ-spectrum disorders Medical conditions (e.g., thyroid, low B12) Drugs (e.g., amphetamines) Bizarre symptoms: • Delusions (e.g., baby possessed) • Hallucinations (e.g., seeing s/o else’s face) • Mood swings (more than non/pp psychosis) • Confusion & disorientation • Erratic behaviour • insomnia •Waxing & waning Risk for suicide and infanticide Psychiatric emergency Postpartum psychosis Rare (1-2/1000 women) Most commonly 2-4 wks/pp Risk Factors Family hx of BAD Early onset depression History of PPD Agenda 2.Understand the psychiatric, obstetric and pediatric implications of a mother’s untreated illness. Economic & health care burden • Yearly estimated costs of depression $14.4 – 44 billion dollars annually (Greenberg, 1993; Stephens, 2001) • The rate of depression among Ontarians is about 4.8% (Statistics Canada, 2003), with women more than twice as likely as men to be depressed (Statistics Canada, 1996-97). • 50% of OB/GYN patients have a significant emotional disturbance • Women with PPD access more community services, make more frequent non-routine visits to the pediatrician; costs are higher for women with an extended duration of illness (Ballinger, 1977; Bryne, 1984; Worsley, 1977) (Petrou, 2002; Chee, 2008) • Peak prevalence of ♀ psychiatric contact (in & outpatient) occurs in the first 3 months after childbirth (Kendall, 1987; Munk-Olsen, 2008) Maternal Risks from A/PPD Coronary artery disease Cancer Hypertension Overactive bladder urinary incontinence Poorer maternal health practices Complications after childbirth Fetal Risks from A/PPD Poorer maternal health practices Elevated cortisol levels Preterm delivery Small for gestational age Low birth weight Schmeelk 1999, Lundy 1999, Hoffman 2000, Adewuya 2007, Hedgaard 1993 Adverse parenting outcomes Depressed mothers: Perceive their infants as more bothersome and make harsher judgments of them Are more irritable and spend less time looking, touching, and talking to their infants Are more likely to neglect/abuse their children Whiffen 1989, Cohn 1990, Chaffin 1996 Adverse parenting outcomes These effects are moderated by: Timing of depressive episode Age of children SES of family Lovejoy, 2000 Attachment Definition : A strong emotional and social bond between infants and their caregivers JOHN BOWLBY (1907-1990) British Child Psychiatrist & Psychoanalyst. He was the first attachment theorist describing attachment as a "lasting psychological connectedness between human beings". Bowlby believed that the earliest bonds formed by children with their caregivers have a tremendous impact that continues throughout life. John Bowlby (1969) Argued babies are born equipped with behaviors (crying, cooing, babbling, smiling, clinging, sucking, following) that help ensure that adults will love them, stay with them and meet their needs. Bowlby (cont’d) Believed quality of early attachment influences future relationships (friends, romantic partners, own children). HARLOW & ZIMMERMAN A famous experiment was conducted by Harlow and Zimmerman in 1959, Which showed that developing a close bond does not depend on hunger satisfaction. They conducted the experiment where rhesus monkey babies were separated from their natural mothers and reared by surrogates- terry cloth covered and other was wire mesh. Babies cling to terry cloth mothers even though wire mesh had bottle. This shows 'contact comfort' is more important Attachment 'FEEDING IS NOT THE BASIS FOR ATTACHMENT' The central theme of attachment theory is that mothers who are available and responsive to their infant's needs establish a sense of security in their children. The infant knows that the caregiver is dependable, which creates a secure base for the child to then explore the world. Attachment When does it form? Usually within the first six months of the infant’s life Shows up in second six months through wariness of strangers, fear of separation from caregiver, etc. Attachment Babies are born equipped with behavior like crying, cooing, babbling and smiling to ensure adult attention & adults are biologically programmed to respond to infant signals. Bowlby viewed the First 3 years are very sensitive period for attachment Four Stages of Attachment Pre-attachment Attachment-in-the- making Clear-cut attachment Formation Of Reciprocal Relationship PREATTACHMENT PHASE Birth-6weeks Baby’s innate signals attract caregiver (Grasping, crying, smiling and gazing into the adult’s eyes) Caregivers remain close by when the baby responds positively The infants encourage the adults to remain close as the the closeness comforts them Babies recognize the mother’s smell, voice and face. They are not yet attached to the mother, they don’t mind being left with unfamiliar adults. They have No fear of strangers ATTACHMENT IN MAKING 6 Weeks – 6 to 8 Months Infant responds differently to familiar caregiver than to strangers. The baby would babble and smile more to the mother and quiets more quickly when the mother picks him. The infant learns that her actions affect the behavior of those around begin to develop “Sense of Trust” where they expect that the caregiver will respond when signaled The infant still does not protest when separated from the caregiver “CLEAR CUT” ATTACHMENT PHASE 6-8 Months to 18 Months -2 Years The attachment to familiar caregiver becomes evident Babies display “Separation Anxiety”, where they become upset when an adult whom they have come to rely leaves Although Separation anxiety increases between 6 -15 months of age its occurrence depends on infant temperament, context and adult behavior FORMATION OF RECIPROCAL RELATIONSHIP 18 Months / 2 Years and on With rapid growth in representation and language by 2 years the toddler is able to understand some of the factors that influence parent’s coming and going and to predict their return. separation protests decline. The child could negotiate with the caregiver, using requests and persuasion to alter her goals Attachment Just the mother? No Attachment to the mother is usually the primary attachment, but can attach to fathers and other caretakers as well. Mary Ainsworth Ainsworth came up with a special experimental design to measure the attachment of an infant to the caretaker The Strange Situation Test – procedure in which a caregiver leaves a child alone with a stranger for several minutes and then returns. STRANGE SITUATION 1. 2. Observer shows caregiver and infant into the experimental room and then leaves. ( 30 Seconds) Caregiver sits and watches child play. (3 mins) 3. Stranger enters, silent at first, then talks to caregiver, then interacts with infant. Caregiver leaves the room. (3 mins) 4. First separation. Stranger tries to interact with infant. (3 mins) 5. First reunion. Caregiver comforts child, stranger leaves. Caregiver then leaves. (3 mins) 6. Second separation. Child alone. (3 mins) 7. Stranger enters and tries to interact with child 8. Second reunion. Caregiver comforts child, stranger leaves. • All episodes except 1 last for 3 mins unless the child becomes very upset STRANGE SITUATION Video http://youtu.be/PnFKaaOSPmk Four Key Observations Exploration : to what extent does the child explore their environment Reaction to departure : what is the child’s response when the caregiver leaves The stranger anxiety : how does the child respond to the stranger alone Reunion : how does the child respond to the caregiver upon returning STRANGE SITUATION Findings Infants differ in quality or style of their attachment to their caregivers. Most show one of four distinct patterns of attachment: 1. Secure attachment 2. Insecure/Avoidant attachment 3. Insecure/ambivalent attachment 4. Disorganized/Disorientated attachment Secure Attachment Most infants (65-70% of 1 yr olds) Freely explore new environments, touching base with caregiver periodically for security. May or may not cry when separated, when returned, crying ceases quickly. Avoidant Attachment 15% Don’t cry when separated React to stranger similar to their caregiver When returned, avoids her or slow to greet her. Ambivalent Attachment 10% Seeks contact with their caregiver before separation After she leaves and returns, they first seek her, then resist or reject offers of comfort Disorganized Attachment 5-10% Elements of both avoidant and ambivalent (confused) Agenda 3. Discuss a biopsychosocial approach to the management of these disorders. Detecting perinatal depression: why screen? High prevalence rate Risks of untreated symptoms Availability of effective treatment Availability of validated screening tools Edinburgh Postnatal Depression Scale (EPDS) 10-item self-report Adv: easy to score, designed for peripartum use, validated ante- and pp, cross-culturally validated Disadv: not linked to DSM-IV-TR criteria, validation studies do not provide definitive answer about optimal cut-off scores Guidelines: score 9-12 pp risk, 12> high risk (cut-off scores above 12 not sensitive in some studies) (Cox & Holden, 2003) Detecting Perinatal Depression Why Screen?? PKU A/PPD 1 in 12 000 babies 1 in 5 mothers Mod-severe MR Serious and lasting effects on mother/child health and family functioning $50/baby free Effective Rx Cost-effective Rx Prevalence Outcome Predictive Screen Cost to Screen Gestational diabetes: 3-10% pregnancies Gestational hypertension: 2-3% pregnancies Educate about self-care NESTS Proper Nutrition Exercise Rest (Sleep protocol) Time for yourself Circles of Support Educate about self-care Sleep SLEEP PROTOCOL: 5h of uninterrupted sleep per night Breaks from baby Enjoyable activities Decrease isolation Spend time with friends, family, other mothers Protect yourself and your energy Limit visitors, lighten chores Treatment Screening and invesigations Check for other diseases Thyroid disease Anemia Diabetes Vitamin deficiencies Treatment Therapy Cognitive Behavioral Therapy Interpersonal Psychotherapy Couple therapy Group therapy Medications Risks of medication 1) to mother 2) to fetus 3) to newborn Risks of disease 1) to mother 2) to fetus 3) to child 4) to family Suicide and homicide -Is there an increase risk of spontaneous abortion/miscarriage? -Is there an increase in the risk of congenital Malformation? -Is there an increase in the risk of adverse outcomes for the neonate? -Is there an increase in the risk of adverse outcomes from breastfeeding? Effects of pregnancy on pharmacokinetics Delayed gastric emptying Decreased gastrointestinal motility Increased volume of distribution Decreased protein binding capacity Increased hepatic metabolism SSRIs Absolute risk of exposure in pregnancy is small. • Paxil Health Advisory • Poor Neonatal Adaptation Syndrome • Persistent Pulmonary Hypertension • Current U.S. Lawsuits Louik 2007, Einarson 2008, Alwan 2008, Greene 2007, Hallberg 2005, Wogelius 2006, Oberlander, Levinson-Castiel 2006, Chambers 2006, 2009, Kallen 2008, Andrade 2009 Mood stabilizers High risk for relapse into bipolar depression with discontinuation Lithium may be the safest alternative Valproic acid: teratogenicity neurobehavioral toxicity • CBZ and LTG lower risk than VPA Folic acid supplementation Li non-responders: consider LTG +/- antipsychotic vs. atypical across pregnancy Wyszynski 2005, Morrow 2006, Cunnington 2007, Meador 2006, Holmes 2004, Cohen 2007 Breastfeeding “It is when the socioeconomic situation is the worst that breastfeeding has the greatest benefit.” Dr. Jack Newman Nutritional advantages Infection, allergy, Ca, diabetes protection Bonding, developmental benefits Postpartum recovery, Ca (breast, ovarian), osteoporosis Free and easy! Mother’s bias Women receiving chronic therapy tend to initiate breastfeeding much less often If they do initiate, they discontinue it much earlier • Continuation of breastfeeding correlates with cumulative amount of reassuring counseling advice women receive from health professionals Moretti et al, 1995, 1998 From Koren 2007 Breastfeeding Generally, excretion rates < 10% into breast milk are considered safe by the American Academy of Pediatrics. [milk]/[plasma]: Molecular size, protein-binding, acidity,lipophilicity • Nursing infant: absorption from GI tract ability to detoxify, ability to excrete . Nothing trumps maternal euthymia Thank you!