Drugs used to treat Bipolar Disorder
advertisement

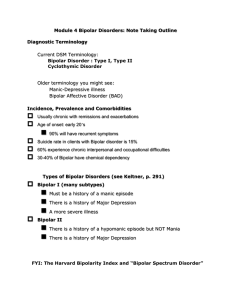
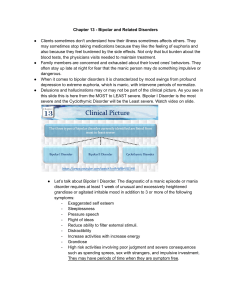
Drugs Used to Treat Bipolar Disorder Background Information Episodes of Mania and Depression Intervention when mood swings are severe, disrupt life of the patient and/or family 4 % population prevalence At least 1 manic,hypomanic,or mixed episode Types/Common Terms Bipolar I- Most severe, obscures normal functioning, hospitalization common Bipolar II- Hypomanic,Full manic episodes rare. Depression often still severe Cyclothymia- Milder form of BP II, “Bipolar Spectrum Disorder” “Rapid Cycling”- 4 or more episodes in a 12 month period,may not be permanent Effects: Estimated 1 out of 4-5 commit suicide from inadequate or no treatment Onset of illness around 25 yrs old and untreated, often results in loss of approx. 9 yrs of life, 14 yrs of activity, 12 of normal health Prime candidates for lifetime treatment express at least 2 episodes of mania Mania vs. Depression:Treatment options Manic Episode- anti-psychotics (ex. Zyprexa), or benzodiazepines (sedating) Depressive Episode- temporary coadministration with antidepressants As a whole- mood stabilizers, classicallyLithium. Anti-epileptics are also currently being used ( Tegretol, Depakote, Neurontin, Lamictal) Lithium Widely recommended treatment for Bipolar Disorder 60-80% success in reducing acute manic and hypomanic states However… issues in non-compliance to take medication, side effects, and relapse rate with its use are being examined in terms of being the best option History 1920’s- used as a sedative, hypnotic, and anti-convulsant 1940’s- investigated as a salt substitute for heart disease patients -How did this work out? - Poorly- many people died from toxicity - The Doctors decided that maybe it wasn’t such a good idea History Cont. 1949- experiments with animals led to lethargy, and use for acute mania. The logic was simply to make them too tired to run out and repaint the entire house, have wild sex and go shopping This is where non-compliance fits in (seen in up to 50% of patients)… the patient feels they are being robbed of their fun by taking meds, so they give them up. More On Non-compliance Other reasons patients refuse meds: -weight gain - less energy, productivity - feel disease has resolved, no longer need medication Relapse rate is high regardless of withdrawal being gradual or acute, suicide risk back up episodes are often worse than original symptoms, so treatment is often life-long So where does this leave us? Since its discovery, Lithium has been found to be superior to placebo In recent years though, efficacy is being questioned: -Long term results not as good as expected -28% discontinue use, 38% experience relapse on the drug *Even so, it is widely prescribed, demonstrates considerable efficacy, and reduction in mortality risks Pharmacokinetics: Peak blood levels reached in 3 hrs, fully absorbed in 8 hrs Absorbed rapidly and completely orally Efficacy correlates with blood levels Crosses blood-brain barrier slowly and incompletely Usually taken as a single daily dose Kinetics Cont. Approx. 2 wks to reach a steady state within the body ½ of oral dose excreted in 18-24 hrs,rest within 1-2 wks Recommended .75-1.0 mEq/L, optimum would be .5-.7 mEq/L, with 2 mEq/L displaying toxicity Metabolized b/f excretion Important: Because of its resemblance to table salt, when Na+ intake is lowered or loss of excessive amounts of fluid occurs, blood levels may rise and create intoxication Pharmacodynamics No psychotropic effect on non-Bipolars Affects nerve membranes, multiple receptor systems and intracellular 2nd messenger impulse transduction systems. Interacts with serotonin Potential to regulate CNS gene expression, stabilizing neurons w/ associated multiple gene expression change. How does a simple ion do all of this? Even as a simple ion, it has complex effects on multiple transmitter systems and mood stabilizing attributes This is due to a latter effect reducing a neuron’s response to synaptic input, and therefore stabilizing the membrane Side Effects and Toxicity Relate to plasma concentration levels, so constant monitoring is key Higher concentrations ( 1.0 mEq/L and up produce bothersome effects, higher than 2 mEq/L can be serious or fatal Symptoms can be neurological, gastrointestinal, enlarged thyroid, rash, weight gain, memory difficulty, kidney disfunction, cardiovascular Not advised to take during pregnancy, affects fetal heart development Combination Therapy Combination therapy with Lithium and anti-epileptics may demonstrate better protection against relapse, greater therapeutic efficacy, and studies support this as a rule vs. an exception Illegal Drug Use More than 55% of Bipolar patients have a history of drug abuse Some abuse might occur before the first episode, or after diagnosis Used by some as a way to self-medicate If Lithium Doesn’t Work 40% of Bipolars are resistant to lithium or side effects hinder its effectiveness Therefore, we must consider alternative agents for treatment Valproic Acid (Depakote) An anti-epileptic, it is the most widely used anti-manic drug Augments the post-synaptic action of GABA at its receptors (increasing synthesis and release) Best for rapid-cycling and acute-mania Therapeutic blood levels: 50-100 Mg/L Side effects include GI upset, sedation, lethargy,tremor, metabolic liver changes and possible loss of hair Can also be used for anxiety, mood, and personality disorders Carbamazepine (Tegretol) Superior to lithium for rapid-cycling, regarded as a second-line treatment for mania Correlation between therapeutic and plasma levels (estimated between 5-10 Mg/L) Side effects may include GI upset, sedation, ataxia and cognitive effects Gabapentin Primarily an anti-convulsant, yet also “off label,” or without FDA approval for treatment of Bipolar and many other anxiety, behavioral and substance abuse problems, possibly pain disorders GABA analogue not bound to plasma proteins, not metabolized, few drug interactions Half-Life is 5-7 hours Side Effects include sleepiness,dizziness,ataxia and double vision Lamotrigine Reported effective with Bipolar, Borderline Personality, Schizoaffective, Post-Traumatic Stress Disorders 98% of administered drug reaches plasma Half-Life is 26 hrs. Inhibits neuronal excitability and modifies synaptic plasticity Side Effects may include dizziness, tremor, headache, nausea, and rash Topiramate and Tiagabine Two newer anti-convulsants that have potential for use in the treatment of Bipolar disorder Atypical Anti-psychotics 3 types that may be used for BPClozapine, Risperidone, and Olanzapine Risperidone seems more anti-depressant than anti-psychotic Clozapine is effective, yet not readily used due to potential serious side effects Olanzapine is approved for short-term use in acute mania Acetylcholinesterase Inhibitors Potentiating the action of acetylcholine may exert relief from mania This potentiation is the result of inhibiting the enzyme acetylcholine esterase Omega-3 Fatty Acids Obtained from plant or marine sources Known to dampen neuronal signaling transduction systems in a variety of cell systems Being investigated as a treatment for Bipolar Disorder Psychotherapeutic and Psychosocial Treatments Combination drug and psychotherapeutic intervention is the most effective treatment Goals of Psychotherapeutic treatment are to reduce distress and improve function between episodes May include cognitive behavioral, psychodynamically oriented, family, couples, interpersonal, and self-help group therapies Thank You