Crtitical Care Case Study
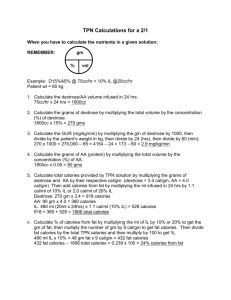
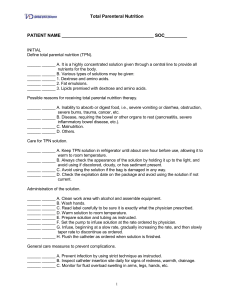
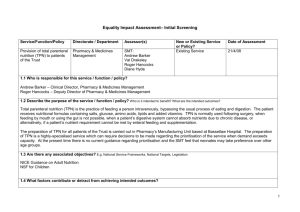
advertisement
Nate Medunick 91 YO female Dry weight – 121# (55kg) Height- 66” BMI-19.5 Admission diagnosis: POD#3Hiatal hernia repair, Nissen fundoplication and wedge resection (SLH), followed by a MI with a stent placed. Barium swallow showed a small perforation at the distal esophagus. Based on actual weight in recent PMH (54kg) Kcals 1350-1620 (25-30kcals/kg) Protein – 70-81g (1.3-1.5g/kg) Fluid 1620ml (30ml/kg) High Nutritional risk A surgeon wraps the part of the stomach known as the gastric fundus around the lower esophagus (including the LES) in a Nissen fundoplication. This helps to strengthen the barrier and prevent the back flow of acids into the esophagus Patients must make dietary and lifestyle adjustments for about six weeks following Nissen fundoplication surgery. Three days following surgery, most patients are on a clear liquid diet, which may include: apple juice beef broth chicken broth cranberry juice decaffeinated tea grape juice Jell-O After the clear liquid diet, most patients are put on a full liquid diet for an additional three days. This diet consists of anything on the clear liquid diet plus the following: Carnation instant breakfast (not chocolate) creamed soups (strained, no broccoli or tomato) cream of wheat (or cream of rice) ice cream (vanilla or strawberry) milk (no chocolate milk) sherbet yogurt (plain, blended, or custard with fruit or seeds) Seven days after surgery, most patients are able to tolerate a soft food diet. However, to heal properly, patients must keep their stomach from stretching. This will require them to eat small, frequent meals six to eight times per day A hiatal hernia is what doctors call it when a part of the stomach moves up into the chest area. Normally, the stomach sits below the diaphragm, the layer of muscle that separates the organs in the chest from the organs in the belly. The esophagus, the tube that carries food from the mouth to the stomach, passes through a hole in the diaphragm. In people with a hiatal hernia, the stomach pushes up through that hole, too. Burning in the chest, known as heartburn Burning in the throat or an acid taste in the throat Stomach or chest pain Trouble swallowing A raspy voice or a sore throat Unexplained cough 91 YO female Dry weight – 121# (55kg) Height- 66” BMI-19.5 Admission diagnosis: POD#3Hiatal hernia repair, Nissen fundoplication and wedge resection (SLH), followed by a MI with a stent placed. Barium swallow showed a small perforation at the distal esophagus. TPN initiated with Day 1 bag- 50g/AA, 100g/dextrose, and no lipids Recommendations Day 2/goal- 80g/AA, 250g/dextrose, providing 1170 calories 50 g lipids Monday and Thursday ( lipid shortage at the time) with lipids, provides 1670 calories Recommendations based on 25 kcal to 30 kcal per Kg for CCU Patient, not vented. Patient required intubation post op day exploratory laparotomy, drainage of mediastinal fluid collection, and placement of gastric and jejunal tubes Day 1 nutrition intervention followed initiating RD care plan: 50g AA, 100g dextrose, no lipids Day 2 Nutrition plan based on dry wt-121 Kcals 1200-1375 (22-25kcal/kg--intubated) Protein- 72-83g (1.3-1.5) wound healing Fluid – Per Intensivist Needs remained constant during care POD #1 S/P exploratory laparotomy, drainage of mediastinal fluid collection, and placement of gastric and jejunal tubes POD #5 hiatal hernia repair, Nissen fundoplication patient continued on mechanical ventilation without sedation, but high doses of neosynephrine lab values include: WBC 17.3 trending up (TU), total bilirubin 1.5 - TU, urine outputapproximately 10 – 33 cc/hr (intubated) Custom TPN- 1500ml-80gm/AA, 115gm/dextrose + 90 gm dextrose from D5 containing IVF, no lipids. Total: 1017 calories Reviewed with Intensivist and asked if IVF would be adjusted Plan moving forward: increase dextrose in TPN because D5 1/2NS was transitioned to NS lipids would be added Monday and Thursday due to national shortage nutritional monitoring and evaluation: tolerance of TPN with goal of 80gm/AA, 200gm/dextrose, transition to jejunal tube feeding when appropriate per surgery recommendations PES P-Inadequate energy intake(improvement shownunresolved) E- S/P exploratory laparotomy (2/18) S-TPN prescribed GI assessment abdomen-distended and soft Bowel Sounds-hypoactive Emesis color- tan Skin 2+ General edema wounds-six total wounds including surgical wounds, Jackson Pratt, and G tube fluid balance-2411.1ml pharmacy-calcium chloride repletion POD#2 S/P exploratory laparotomy. Diet: NPO, TPN, and trophic feeding jevity 1 cal@ 10ml/hr (254kcal, 11gm/protein) prescribed by Thoracic surgeon (jevity 1 cal was MD preferred) labs included: phosphorus 3.0 trending down (TD), potassium 4.1 stable, calcium 7.6 stable, magnesium 2.0 (TD), CO2/PCO2 38 (TD) TPN order and discussed with Intensivist1500ml, amino acids-80gm (320kcal), dextrose140gm (476kcal), lipids-40gm (400kcal)- no MVI, no trace elements, with trophic feeding, total calories/protein: 1450 total kcals, 91 gm protein Custom electrolytes K acetate 40mEq (potassium stable), Na phosphate 25 mEq ( repletion), Na acetate 22, Ca gluconate 9(stable), Mg sulfate 7(repletion) the original electrolyte plan - K acetate 40mEq , Na phosphate 25 mEq , Na acetate 22, Ca gluconate 9, Mg sulfate 7 Plan changed following a discussion with the Intensivist - concern was- Although; CO2 was TD, pH-7.38 Slightly more Acetate would possibly increase pH over 7.38 Acetate is added to correct Acidosis; Intensivist felt that the Patient was not trending toward acidosis at the time POD#3 S/P exploratory laparotomy. Diet: NPO, TPN, and trophic feeding jevity 1 cal @ 10ml/hr (254kcal, 11gm/protein) patient continued on mechanical ventilation with propofol sedation and Neo-Synephrine weaned to lower dose IVF-NS @ 50ml/hr continued Labs include: Ca 8.0, Cl 112, Mg 2.0, Phos 1.8, and Potassium 3.7 nutritional intervention-TPN – 1500ml: 80gm/amino acids (320kcal), 165 gm /Dextrose (561kcal) 6 ml/hr propofol (158 calories ) trophic TF (254 calories, 11 gm protein) D5 carriers with multiple antibiotics (127 kcal) Total ~1420 calories, 91 gm protein TPN electrolytes 40mEq K acetate, 15 mEq K phosphate, 25 mEq Na phosphate, 9 mEq Ca gluconate, 7 mEq Mg sulfate. TPN discussed with Intensivist JH was in poor condition toward the end of my nutritional care rotation: Patient was requiring multiple antibiotics, including zyvox LFTs/renal labs were elevating, multisytem organ failure ensued I found out that JH soon expired due to poor condition and advanced age I would not have changed anything with my nutritional plan of care What I learned What I learned: TPN and electrolyte needs pH and acid/base balance Intensivists are approachable and a great information source RD’s recommendations can show direct results in lab work http://www.healthline.com/health/gerd/nis sen-fundoplication#2 http://www.uptodate.com/contents/hiatalhernia-thebasics?source=search_result&search=Hiatal+h ernia&selectedTitle=2%7E75