B. anthracis
advertisement
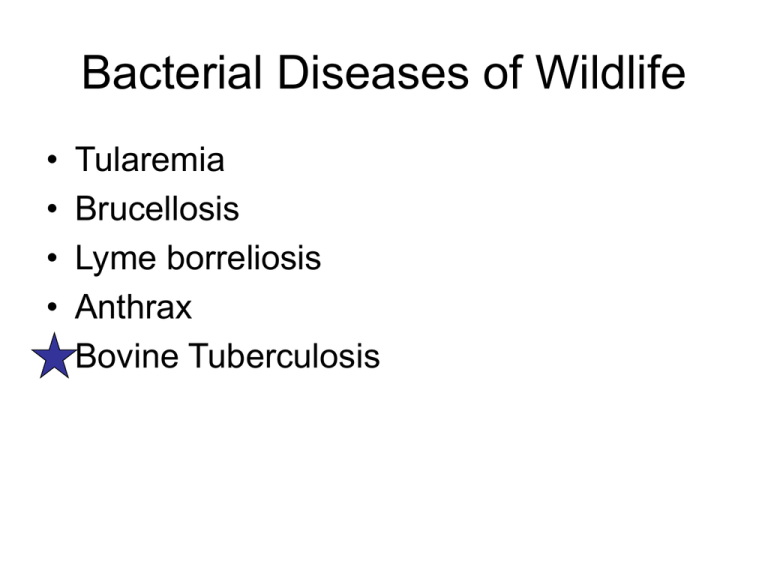
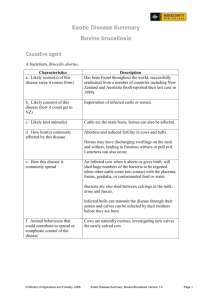
Bacterial Diseases of Wildlife • • • • • Tularemia Brucellosis Lyme borreliosis Anthrax Bovine Tuberculosis Tularemia – aka rabbit fever Basic Micro • Francisella tularensis • Gram negative • Phylum Proteobacteria Class Gamma • Obligate aerobic • Non-spore-forming • 4 known subspecies – Type A – more virulent – N. America – Type B – less virulent - Europe In liver cells Animal Clinical Signs Lagomorphs – very susceptible Depression, anorexia, ataxia, roughened coat, tendency to huddle, weakness, fever, ulcers, abscesses at site of infection, swelling of regional lymph nodes, sudden death caused by septicemia. Rodents – very susceptible Sheep - susceptible Depression, anorexia, ataxia, roughened coat, tendency to huddle. Dogs – fairly resistant Low fever, mucopurulent ocular and nasal discharge, abscesses at site of infection, axillary and inguinal vesiculopapular rash, loss of appetite, listlessness, lymphadenopathy, anorexia. Humans Fever, localized skin or mucous membrane ulceration, regional lymphadenopathy, and, occasionally, pneumonia. Sudden onset of fever, lethargy, anorexia, stiffness, reduced mobility, signs of septicemia, depression, dysnpnea, diarrhea, lag behind rest of the herd, coughing, pollakiuria, abortions, carry heads high when walking, weak or rapid pulse, frequent urination, death. Tularemia Pathogenic features • Pili (attachment to host tissue) • Capsule (protects against complement) • Facultative intracellular (cytoplasm of host macrophages) • AcpA – acid phosphatase, inhibits respiratory burst (avoid destruction by phagocytes) • Siderophore (small molecules that bind iron, then taken up by bacterium) • 30 kb pathogenicity island – iglC (escape), pdpD, pdpA - unknown Tularemia Transmission and Epidemiology • Can persist for long periods of time in moist environs (water, mud, decaying animal carcasses). • Reservoirs – Natural - small and medium-sized mammals • North America – leporidae, castoridae, muridae, sciuridae – Natural - Acanthamoeba – Incidental - humans, other mammalian species, some species of birds, fish, and amphibians. • Vectors – Hard ticks – primary vector of Type A - transovarian – Biting flies – Mosquitoes Tularemia Pathology • Infection – dose,10 cells • To regional lymph nodes – Engulfed by macrophages – Escape from phagosome into cytoplasm within 3-4 hours Lymph nodes show welldefined zones of necrosis, predominantly in the outer cortex. 100X 400X Tularemia Pathology • Hematogenic dissemination to liver, spleen, lungs The most common pulmonary histologic finding is suppurative pneumonia with areas of necrosis and hemorrhage. Sections of liver showed rounded microabscesses. Tularemia Pathology • Typical lesions are pale white to gray, often slightly raised necrotic foci, ranging in size from pin-point to a few millimeters in diameter. • Impairment of organ functions (liver, spleen, lungs) • Death in susceptible – 2-10 days Brucellosis – aka Malta fever, Bang’s disease, undulant fever Basic Micro • Brucella – – – – – B. abortus (cattle) B. melitensis (goats) B. suis (swine) B. ovis (sheep) B. canis (dogs) • Gram negative • Phylum Proteobacteria Class alpha • Aerobe • Non-spore-forming Animal Clinical Signs Domestic, feral, wild Abortion, retained placenta, enlarged testicles, pendulous scrotum Humans Acute febrile disease - fever 3840C. Unusually severe limb and back pain, sweating and fatigue are marked. On physical examination, splenomegaly may be the only finding. Untreated, symptoms may continue for 2 - 4 weeks. Persistent disease - arthritis, often sacroiliitis, and spondylitis (in about 10% of cases), CNS effects including meningitis (in about 5%). Brucellosis Pathogenic features • Lacks “classical” virulence factors • Facultative intracellular in monocyte-macrophages • Cell-wall polysacc protects cell from phagosome and inhibits apoptosis • Escapes phagosome, replicates in ER • Enterobactin (iron chelator) • Stimulates polyclonal B cell activation entering a macrophage massive proliferation in macrophage Brucellosis Transmission and Epidemiology • Transmitted via ingestion of contaminated feed, licking infected fetus, calf, placenta; also conjunctival, inhalation • Reservoirs – various wild, feral and (particularly) domestic animals. In ruminants, enormous numbers of bacteria are shed widely from infected products of conception, whether aborted or born at term. Brucellae frequently invade the mammary gland of infected ruminants. • Individuals are infected for life, and herds are chronically infected Brucellosis Pathology • Invades from point of entry • Bacteremia + entry into phagocytes • Initial localization in regional lymph nodes and spleen. • Invasion of reproductive organs • Severe inflammation of the placenta prevents oxygen and nutrient delivery to fetus and removal of waste products fetal death • Alternately – hormonal dysregulation results in premature delivery. Lyme Most prevalent tick-borne disease of humans in US – 20,000/yr Basic Micro • Borrelia burgdorferi • Gram negative • Spirochete Lyme Pathogenic features • Erp outer membrane lipoproteins (protect from complement-mediated killing) • One of the few pathogens that does not require iron. • Different genes expressed in tick vs mammal. Lyme Transmission and Epidemiology • Natural reservoir – white-footed mouse • Vector – ticks in the genus Ixodes Lyme Nymph Eggs Eggs Larva Adult Lyme Pathology Deposited in skin by ticks during feeding Replicate in dermis for ~ 1wk Disseminate to distant cutaneous sites, organs, joints Localized inflammatory response triggered by surface antigens w/ unusual prod. of interleukin and interferon Anthrax One of oldest diseases known – account in the book of Exodus Basic Micro • Bacillus anthracis • Gram positive • Phylum Firmicutes Class Bacilli • Obligate aerobe • Spore-forming Anthrax Pathogenic features • Capsule • Toxin complex consisting of: – Cell-receptor binding protein called protective antigen – Two separate toxins • Edema factor (EF) • Lethal factor (LF) • Toxin complex works to: – prevent apoptosis – increase capillary permeability – reduce blood clotting Anthrax • Symptoms that may appear immediately before death are high temperatures, bloody discharge, and swelling in the neck and shoulder areas. • Carcasses – dark blood, not clotting. Bloody serous discharges from nose, etc. Anthrax Transmission and Epidemiology • Persistence depends on extreme virulence, death of the host, and survival of highly resistant spores in the environment for prolonged periods. • Infects a wide range of homeothermic species (body temp is critical). • Carcasses of dead animals attract scavengers that free vegetative cells and disperse them over a wide area. • Herbivores are much more susceptible than carnivores – but carnivores and scavengers are carriers of spores, transmitted in feces. Anthrax Complicated “life cycle” • Vegetative B. anthracis require aerobic and high nutrient conditions. • When host dies, tissues become anaerobic. • B. anthracis are held in stasis, unable to replicate or sporulate • Anaerobic bacteria from GI, esp. Clostridium spp. decompose carcass. • Carcass is opened and vegetative B. anthracis dispersed. Anthrax Complicated “life cycle”. • In the environment, low nutrient conditions and dehydration stimulate sporulation. • Spores resistant to extremes of temp., UV, desiccation, chemicals… • Epidemics tend to occur in moist lowland areas where soil is high in organic content, in dry summer months following period of heavy rain or floods – role of water. Anthrax Pathology • 3 routes of entry 1. 2. 3. • • Gastrointestinal – across intact mucous membranes or defects in epithelium of oropharynx or GI Cutaneous – spores enter through cuts and abrasions Inhalational – spores inhaled to alveoli of lungs Spores germinate into vegetative cells Carried to lymph nodes Anthrax Pathology • Cross into bloodstream and disseminate via circulation • Terminal blood concentration greater than 107 CFU/mL. • Produce toxins – – – – – Edema Shock Acute renal failure Terminal anoxia Death In bovine blood Bovine tuberculosis Mycobacterium bovis is the causative agent of tuberculosis in a range of animal species and man, with worldwide annual losses to agriculture of $3 billion. Basic Micro • • • • • Mycobacterium bovis Gram positive, rods Acid-fast Phylum Acintobacter Aerobic Bovine TB Pathogenic features • Intracellular in macrophages – Prevent phagosome-lysosome fusion Bovine TB Transmission and Epidemiology • M. bovis can be transmitted by the inhalation of aerosols, by ingestion, or through breaks in the skin. The importance of these routes varies between species. • Bovine tuberculosis is usually maintained in cattle populations, but a few other species can become reservoir hosts. Most species are considered to be spillover hosts. Bovine TB Transmission and Epidemiology • Natural, primary host – cattle • Maintenance hosts - brush–tailed opossums (and possibly ferrets) in New Zealand, badgers in the United Kingdom and Ireland, bison and elk in Canada, and kudu and African buffalo in southern Africa. White-tail deer in MI and MN. • Spillover - sheep, goats, horses, pigs, dogs, cats, ferrets, camels, llamas, many species of wild ruminants including deer and elk; elephants, rhinoceroses, foxes, coyotes, mink, primates, opossums, otters, seals, sea lions, hares, raccoons, bears, warthogs, large cats (including lions, tigers, leopards, cheetahs and lynx) and several species of rodents. • Most mammals may be susceptible. Bovine TB Transmission and Epidemiology • Cattle shed M. bovis in respiratory secretions, feces and milk, and sometimes in the urine, vaginal secretions or semen. Large numbers of organisms may be shed in the late stages of infection. • Some animals become infected when they ingest the organism; this route may be particularly important in calves that nurse from infected cow. Bovine TB • The symptoms of bovine tuberculosis usually take months to develop in cattle. Infections can also remain dormant for years and reactivate during periods of stress or in old age. • Similarly, severe disease can develop in some deer within a few months of infection, while other deer do not become symptomatic for years. Bovine TB Symptoms • Tuberculosis is a chronic, progressive disease that can cause gradual debilitation and is manifest as emaciation, depression, and intolerance to exercise. • Because infection often involves the lungs, coughing, nasal discharges, and difficulty breathing can occur in severe cases. • In some instances, superficial lymph nodes in the neck will develop large abscesses that may rupture and drain through the skin. Bovine TB Pathology • tiny droplets containing 1-3 bacteria reach the alveoli (10-200 droplets) phagocytized by unactivated alveolar macrophages M. bovis survive • • – – • impair normal phagocyte functions multiply young phagocytes are actively recruited but don’t kill Bovine TB Pathology • • local infection spread via lymphatics to regional nodes then thru blood to any other organ • – • spread to CNS, spongy bone, liver, kidney, genitals host immune response usually kills infected macrophages and halts infection Bovine TB Pathology • • At necropsy, tuberculosis lesions are variable in appearance and size. Subclinically infected animals may have one or a few small necrotic nodules that usually are associated with the lymph nodes of the head and neck or the lungs. Bovine TB Pathology • More severely infected cervids can have multiple pea-sized nodules or large cheesy or pus-filled masses in the same areas. The classical tubercle, which is firm, white or pale yellow, and gritty when cut, does occur in cervids, but many M. bovis lesions in these animals are filled with pus. • In cervids, tuberculous lesions are most often seen in the lymph nodes of the head and neck or in lung tissue; however, lesions can occur throughout the chest cavity, under the skin of the chest, and in the abdominal cavity as well.