orthopaedic emergencies
advertisement

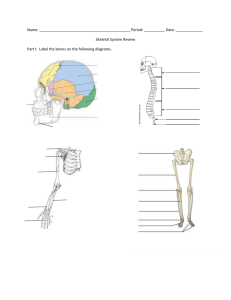
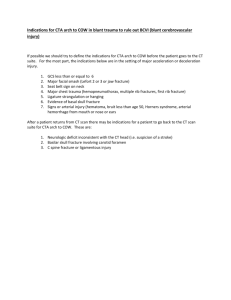
ORTHOPAEDIC EMERGENCIES Gede Chandra P. Yudha ORTHOPAEDIC EMERGENCIES • Definition : – Any musculoskeletal problem requiring emergency management – Life threatening – Limb threatening ORTHOPAEDIC EMERGENCIES 1. 2. 3. 4. 5. 6. Open fracture Compartment syndrome Dislocation Vascular injury Unstable pelvic fracture Septic arthritis OPEN FRACTURE • Definition : – Osseus disruption in which a break in the skin and underlying soft tissue communicates directly with the fracture and its hematoma • 1/3 of patients with open fractures are multiply injured • Any wound occuring on the same limb segment as a fracture must be suspected to be a consequence of an open fracture until proven otherwise OPEN FRACTURE • Mechanism of injury – High energy – In out – Out in OPEN FRACTURE PRIMARY SURVEY • AIRWAY • BREATHING • CIRCULATION • DISABILITY • ENVIRONMENT SECONDARY SURVEY • HEAD TO TOE EXAMINATION ASSES EXTREMITY INJURY • DEGREE OF SOFT TISSUE INJURY • DEGREE OF SKELETAL INJURY • NEUROVASCULAR STATUS OPEN FRACTURE • Radiographic evaluation – Trauma survey lateral view cervical spine, AP view of the chest and pelvis – Extremity radiographs are obtained as indicated by clinical setting, injury pattern, and patient complaints OPEN FRACTURE • Classification (Gustillo & Anderson) Open Fracture Grade I Open Fracture Grade II Open Fracture Grade III A Open Fracture Grade III B OPEN FRACTURE • Management – Emergency room management • • • • Perform careful clinical and radiographic evaluation Initiate parenteral antibiotics Symptomatic treatment Assess skin and soft tissue damage, place a salinesoaked sterile dressing on the wound • Perform provisional reduction of fracture and then splint • Antibiotics • Tetanus prophylaxis OPEN FRACTURE • Management – Operative treatment • Debridement – Irrigation – Removal of devitalized tissue – Removal of foreign bodies • Reduction • Fixation – Internal – External COMPARTMENT SYNDROME • Compartment : – groupings of muscles, nerves, and blood vessels in extremities, covered by fascia • Definition : – Increased intracompartment pressure to a level that can compromise tissue perfusion – May cause irreversible muscle and nerve damage – ICP (intra compartmental pressure) within 30 mmHg from diastolic pressure • Usually happen in leg, forearm, hand, foot • Causes : – Increased Volume - internal : hemorrhage, fractures, swelling from traumatized tissue, increased fluid secondary to burns, post-ischemic swelling – Decreased volume - external: tight casts, dressings COMPARTMENT SYNDROME • Patophysiology – “vicious cycle” – Muscle ischemia • 4 hours - reversible damage • 8 hours - irreversible changes • 4-8 hours - variable – Nerve ischemia • 1 hour - normal conduction • 1- 4 hours - neuropraxic damage - reversible • 8 hours - axonotmesis irreversible COMPARTMENT SYNDROME • Diagnosis – Clinical (5 P) • Pain early sign “pain on passive strech, out of proportion, progressive, not relieved by immobilization” • Paresthesia • Paralysis • Pallor • Pulselessness – ICP pressure measurement COMPARTMENT SYNDROME • Management – Remove any restricting bandages, cast – Symptomatic treatment – In doubt monitoring pressure every 4 hours, in 24 hours – Definite fasciotomy DISLOCATION • Joint moves beyond normal range, loss of contact of joint surface • May be complete or partial • Partial subluxation • Causes deformity, severe pain, rigidity, loss of function • Neurovascular compromise DISLOCATION • Clinical sign : – Look : deformity, shortening, rotation – Feel : pain, empty socket (eg : empty shoulder in shoulder dislocation), assess distal neurovascular – Move : decrease ROM • Imaging : – X-ray : loss of joint contact DISLOCATION • Management – Primary survey – Secondary survey – Definitive • Reduction under GA – May be closed or open – Must be done within 6 hours since injury • Immobilization after reduction VASCULAR INJURY • Vascular injury often follows fracture or dislocation • Important to always check the distal vascular status! VASCULAR INJURY • Mainly arteries • Clinical signs : – Hard signs • Pulsating bleeding • Direct view of anterial injury – Soft signs • Hematome • Non pulsating VASCULAR INJURY • Management : – Early : • Primary & secondary survey • Stop bleeding apply external pressure – Definitive • Exploration • Further management depends on the findings during exploration : – Rupture repair, or vascular graft – Trombosis vascular graft – Reduction & stabilization (if fracture or dislocation present) UNSTABLE PELVIC FRACTURE • Pelvis – 2 innominate bones + 1 sacrum – Bond together by strong ligamentous complex maintain stability, vertically & horizontally – Major vessels close to the bone UNSTABLE PELVIC FRACTURE • Pelvic fracture (pelvic ring fracture) – Stable • Configuration • Hemodynamic – Unstable • Configuration • Hemodynamic • Mechanism of injury : – High energy trauma – Force direction (4) : • • • • Lateral compression Anterior Posterior compression Vertical shear Combined • Pelvic fracture classification (Young & Burgess) • Clinical evaluation : – Perform primary survey – Initiate resuscitation. Adress life threatening injuries – In suspicion of pelvic fracture, check : • • • • Leg length discrepancy Pelvic instability test can only be performed once Hematoma in flank, around iliac crest, perineum Urethral injury often accompanies pelvic fracture blood in MUE, butterfly hematoma, floating prostate • Vaginal or rectal perforation by fracture fragments • Pelvic AP X-ray using portable X-ray • FAST Focused Assesment Sonography for Trauma • Management : – Problem : hemorrhage – Primary survey & resuscitation • 2 large bore IV cath • IV fluids (crystalloids, blood) • urine production monitor – Other options : • • • • • Pelvic binder Pelvic sling Pelvic clamp External fixator MAST / PSAG Pelvic Sling & C-clamp Pelvic External Fixator Pneumatic Anti Shock Garments SEPTIC ARTHRITIS • Definition – Acute joint infection due to bacterial agents – Medical emergency • Epidemiology – Incidence: • • • • 40-68/100000/ yr in Prosthetic joint 28-38/ 100000/ yr in RA 5- 12/ 100000/ yr in Children 2-5/ 100000/ yr in GP – In Adult: 75% with risk factor SEPTIC ARTHRITIS • Risk factors: – Systemic: • • • • • • Old age (>80 Y) RA DM Immunosuppressive Hemodyalisis Malignancy – Local: • RA • OA • Prosthetic joint SEPTIC ARTHRITIS • Etiology (microbiology) – Microbial agent: • Staphylococcus aureus: most common (7580%) • Other organism in special patients: – Sexually active woman: Neisseria gonorrheae – Elderly, IV drug abuser, immunocompromised, UTI: Gram negative (p. aeruginosa and E.coli) – HIV: Pneumococci, Salmonella, H. influenzae – Alcoholism, Humeral immunity abnormality, Hemoglobinopathies: Pneumococcal infections SEPTIC ARTHRITIS • Root of infection: – Blood stream – Contiguous infection – Direct inoculation: • Injection: 0.0002 • Arthroscopic surgery: < 0.005 • Animal or human bite SEPTIC ARTHRITIS • Site of involvement: – Mono (80-90%) • • • • • • • • • Knee: 55% Ankle: 10% Wrist: 9% Shoulder: 7% Hip: 5% Elbow: 5% SC: 5%- IV drug abuser SI: 2%- IV drug abuser Foot joints: 2% – Poly (more than 1 joint): RA SEPTIC ARTHRITIS • Clinical manifestations – Fever (toxic) – Look : swelling, redness – Feel : warmth, pain, effussion – Move : limited ROM • Synovial fluid aspiration pus Acute Monoarthritis Sepsis workup Biochemist Positive B/C : 50-70% Leukocytosis ESR & CRP Synovial Fluid Aspiration Smear- Culture Light microscope Positive Gram stain: 75% in s. aureus 30-50% in gram (-) Positive Fluid culture: 90% PCR: partially treated or culture negative SEPTIC ARTHRITIS • Radiographic changes – Early: • Soft tissue swelling Joint space widening – Late (2-3 w): • Erosion • Joint space narrowing TREATMENT Supportive Bed rest IV Fluids Analgesics Antipiretics Antibiotic Empiric (IV): Smear Age or Risk factors Extra articular site Definitive therapy; based on culture Joint Drainage Closed needle Aspiration Arthrotomy: Hip, Shoulder Arthroscopic Drainage: Symptom S. fluid volume S. fluid WBC S. fluid smear & culture Empirical antibiotic