Раптова втрата зору. Гострий приступ глаукоми. Емболія
advertisement

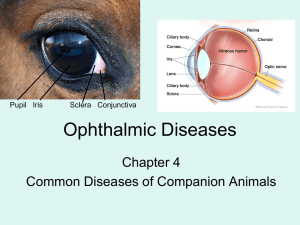
Lecture 2 «RED EYE» DISEASES Lecture is delivered by Ph. D., assistant of professor Tabalyuk T.A. TYPES of INJECTION of EYEBALL: 1. Superficial or conjunctival; 2. Deep or ciliary or pericorneal; 3. Mixt TYPICAL FOR ALL TYPES OF CONJUNCTIVITIS ARE THE NEXT SIGNS: 1. RED EYE (superficial injection); 2. CORNEAL SYNDROME (photophobia, profuse tearing, blepharospasmus); 3. DISCHARGE from the eye KEY SIGNS of BACTERIAL CONJUNCTIVITIS: purulent & sticky discharge from the eye; bilateral, but frequently asymmetrical ACUTE EPIDEMIC CONJUNCTIVITIS KOHA-UYIXA: oedematous & thicken bulbar conjunctiva form two triangules arround cornea; haemorrhages under bulbar conjunctiva GONOCCOCAL CONJUNCTIVITIS: usually bilateral in infants & monolateral in adults; first 3-4 days discharge with blood remainder, then profuse purulent discharge (gonoblennoreia); easy bleeding conjunctiva PNEUMOCOCCAL CONJUNCTIVITIS: membranes on palpebral conjunctiva, which are easy removed; conjunctiva does not bleed after membranes removing DIPHTERITIC CONJUNCTIVITIS: membranes on palpebral conjunctiva and eyelids edges, which are removed with difficulty; conjunctiva bleeds after membranes removing; on the places of membranes location star scars appears soon; combimation with diphteria of nose, throat, laryngs etc. KEY SIGNS of VIRAL CONJUNCTIVITIS: serous watery discharge; pink folliculae on lower eyelid conjunctiva; palpable prearicular lymph nodes; subconjunctival haemorrhages; infectuion usually begins in one eye & in 2-3 days spreads into the fellow eye general reaction of the organism (fever, sore throat etc.) or upper respiratory infection in anamnesis ALLERGIC CONJUNCTIVITIS: itching subjectivelly; papillae on upper eyelid conjunctiva; allergic anamnesis TRAHOMA (caused by Chlamydia trahomatis) chronic duration; four phases (infiltration, progression, regression, scaring); large yellow-gray folliculae on thicked conjunctiva of upper eyelid; typical corneal damage – pannus tracomatosus in upper part with superficial neovascularization; formation of large star scars Complications & outcome: trichiasis; madarosis; stricturae of lacrimal exretory system; symblepharon; xerosis etc. LOCAL ANTIBACTERIAL TREATMENT: drops - S.Sulfacili Na 30 %, S.Dimexidi 10 %, S.Gentamycini 0,3 %, S.Laevomycetini 0,25 %, S.Polymixini B 0,25 %, S.Tobramycini 0,3 %, S.Chlorhexidini 0,02 %, S. Ciprophloxacini 0,3 %, Сiloxani etc. ointments – Ung. Tetracyclini 1 %, Ung. Tobramycini 0,3 %, Ung. Erythromycini 1 % etc. LOCAL ANTIVIRAL TREATMENT: drops -Interferoni, Reaferoni, Laferoni, Viaferoni, Interlok IDU, S. Florenali 0,1 %, S. Oxolini 0,1 %, S. tebrofeni 0,1 % etc. ointments – Ung. Florenali 0,5 %, Ung. Oxolini 0,25 %, Ung. Tebrofeni 0,5 %, Ung. Acycloviri 5 % (or Zovirax or Verolex) etc. LOCAL ANTIALLERGIC TREATMENT: drops – S. Ca Chloridi 3 %, S. Dexamethasoni 0,1 %, «Lecrolyn» (Santen), «Alomid» (Alcon), «Emadin» (Alcon) etc. ointments –Ung. Maxidex & other corticosteroids. TYPICAL FOR ALL TYPES OF KERATITIS ARE THE NEXT SIGNS: 1. Red eye (deep injection, in severe cases mixt injection); 2. Corneal syndrome (photophobia, profuse tearing, blepharospasmus); 3. Reducing of visual acuity; 4. Lasting pain, more severe in daytime, when eye is open; 5. Inflammatory infiltrate in the cornea BACTERIAL ULSER caused by pneumococcus, pseudomonas, diplococcus, strepthococcus, staphylococcus etc. It is exogenis keratitis and always is a result of cornea microtrauma. The hallmark signs are: acute beginning, severe corneal syndrome, corneal ulcer with one progressive edge The lysis of cornea till Descemet’s membrane is called descemethocele. It is threat for corneal perforation. Bacterial ulser often is associated with pus in anterior chamber – a hypopion. The complications of bacterial ulser: corneal perforation, panuveitis, endophthalmitis, orbital cellulitis Bacretiological and bacteriscopical researching are necessary. The treatment is performing in clinic CLINICAL FEATURES of ADENOVIRAL KERATITIS: many punctate subepithelial solitary round infiltrates (like a coin) not juting out; decreasing of corneal sensitivity on the hole surface not only above the infiltrate; folliculular conjunctivitis; palpable prearicular lymph nodes; general reaction of the organism (fever, sore throat etc.) or upper respiratory infection in anamnesis CLINICAL FEATURES of HERPES KERATITIS: unilateral, less corneal syndrome, bilateral decreasing of corneal sensitivity, prolongated duration, recidivation Imunodiagnostic is necessary. It may be primary (in age 5 month-5years) in first virus penetration and postprimary in inficated person. The clinical forms of secondary herpes keratitis: superficial (vesiculous and dendritic) & deep (like disc, methaherpetic and deep stromal). SYPHILITIC PARENCHYMATOUS KERATITIS – the late (often in 6-20 years old) appearence of congenital syphilis. The diagnosis is confirmed by positive serological reaction (RW). The three cardinal symptoms of congenital syphilis are the next: keratitis, deafing, special teeth The cyclic duration is typical for this keratitis: phase of infiltration (3-4 weeks) – less corneal syndrome, the dissemination of punctate infiltrates in corneal stroma from periphery (limbus area) to the center; phase of vascularusation (6-8 weeks) – intensive infiltration and deep vascularization, express corneal syndrome; regressive phase (1-2 years) – the regression of infiltrates from the center to the periphery. For syphilitic parenchymatous keratitis is not typical ephithelium defect (fluorescein test is negative). The disease is bilateral. The inflammation of second eye usually occurs in two or more years. The specific treatment: Extencillini (Penicillini G) 2.4 mln. OD for injection. The injection is repeated in 7 days. HAEMATOGENIC TUBERCULOTIC KERATITIS caused by mycobacterium tuberculosis Clinical peculierities: large isolate yellow infiltrates in deep layers at any part of cornea; mixt (superficial and deep) vascularization; torpid recurrent duration, without acute inflammation; scleritis may occur; unilateral; positive tuberculine tests Imunodiagnostic is necessary. The treatment includes general and topical usage of antituberculotic drugs (isoniazidi, streptomycini); imunomodulators; vitamins. TUBERCULOTIC ALLERGIC KERATITIS is a local reaction of sensilization. It is usually occurs in children with nonactive primary lung tuberculosis and peripheral lymph nodes tuberculosis. Permanent symptoms: flictena (gray small focus in superficial corneal layers) superficial vessels are companions of flictena corneal syndrom is extensive Mantoux’s test is positive X-ray examination and blood analysis are necessary. The treatment includes corticosteroids and desensilization drugs, not antituberculotic. MANAGEMENT PRINCIPLES in KERATITIS • Specific treatment: antibacterial, antiviral, antifungal etc. medicines generally (intravenous, intramuscular injections, per os) and locally (in drops, ointments, subconjunctival and parabulbar injections). • Mydriatics to prevent uveitis. • Stimulators of corneal regenerations (1 % chinini hydrochloridi, 4 % taufoni, emoxipini, solcoserili, actovegini, corneregel, dexpanthenol, methyluracili, vitasik). • Proteolytic ferments locally for infiltrate lysis (fybrinolysini, lidasae, collalysini). • Desensilization therapy (Diazolini, Tavegili, Klaritini). • Imunocorrection (Decaris, Timalini, Taktivini, Chigaini) • Vitamins (B1, B2, C etc.). OUTCOME of KERATITIS is corneal opacity, which includes: nubecula – it can be seen only by special examination macula – it can be seen without special examination by our eye, but the iris and pupil are seen through it leucoma - it can be seen without special examination, but the iris and pupil can’t be seen through it We try to treat corneal opacity during one year with the help of proteolytic ferments (fibrinolysini, lidasa, kolallisini) in drops, subconjunctival injections and physiotheraputic procedures. If the scarring is axial in the cornea, the vision of the eye may be permanently impaired. In these circumstances, some improvement may be obtained with spectacles, but a contact lens may give better vision. In severe cases, a corneal graft will be required in order to improve the sight. DIFFERENTIAL DIAGNOSIS of CORNEAL INFILTRATE & OPACITY Sign Red eye Corneal infiltrare Corneal opacity + _ + _ Limits irregular regular Cornea not glassy glassy fluorescein test positive negative Corneal syndrome The anterior uveitis is inflammation of iris and ciliary body. Thus its another name is “iridocyclitis”. The mixt injection, corneal syndrome, pain, which increases at the night, and decreasing of visual acuity are typical. Aethiology: commonly idiopathic but numerous systemic causes – HLA-B27associated (ankylosing spondylitis, Reiter’s syndrome, psoriatic arthritis); juvenile idiopathic arthtritis (especially high risk if pauciarticular-onset and ANApositive); inflammatory bowel diseases (ulcerative colitis,Crohn’s disease); noninfectious systemic diseases (sarcoidosis, Behchet’s disease, Vogt-KoyanagiHarada syndrome); infections (herpes zoster and simplex, syphilis. tuberculosis). Clinical features of iritis: pain increases in lighting; changing of iris picture (another colour, oedema, vessels are seen); small pupil (miosis) and its weak reaction on light; posterior synechiae (iris-lens adhesions) Clinical features of cyclitis: pain increases in palpation (ciliary pain) and accommodation; keratic precipitates; vitreous opacities; changes of intraocular pressure (usual first increasing then decreasing) Сomplications of anterior uveitis: panuveitis, endophthalmitis, panophthalmitis Outcome of anterior uveitis: secondary glaucoma, complicated cataract, vitreous opacity, hypotonia, eye atrophy Management: Topical steroids and mydriatics are the mainstay of treatment Periocular steroid injection Systemic steroids, immunosuppressive agents and antibiotics for the infections (e.g. tuberculosis, syphilis) First aid in iridocyclitis: Mydriatics Steroids Diuretics In posterior uveitis or choroiditis the eye is quiet (not red), pain doesn’t disturb, corneal syndrome is not typical. The visual functions are decreased. Patches are seen in ophthalmoscopy. Aethiology: toxoplasmosis, toxocariasis, cytomegalovirus, histoplasmosis, tuberculosis, syphilis etc. For central choroiditis metamorphopsia, photopsia, central scotoma and loss of visual acuity are typical. For peripheral choroiditis peripheral scotoma and narrowing of visual field are typical. Management: antimicrobial or antiviral agents administered systemically and topical. DIFFERENTIAL DIAGNOSIS between NEW & OLD FUNDUS PATCH Sign colour new patch old patch pink white or yellow limits irregular regular pigmentum in the center on periphery oedema + - CLINICAL FEATURES of ENDOPHTHALMITIS: + red eye (mixt injection); corneal syndrome; reducing of visual acuity; pain hypopion (pus in the anterior chamber); abscess of vitreous (yellow fundus reflex) CLINICAL FEATURES of PANOPHTHALMITIS: + red eye (mixt injection); corneal syndrome; reducing of visual acuity; pain; hypopion; abscess of vitreous imbibition of cornea by pus purulent choroidoretinitis (with visual field defects & fundus patches if seen) DIFFERENTIAL DIAGNOSIS of INFLAMMATORY DISEASES OF EYE ANTERIOR SEGMENT Sign red eye conjunctivitis + (superficial injection) keratitis + (deep or mixt injection) iridocyclitis + (deep or mixt injection) corneal syndrome + + + pain - + + (in daytime) (at night, incresing in lighting & palpation) decreased visual acuity - + + peculierities discharge corneal infiltrate keratic precipitates, posterior synechiae, miosis, vitreous opacities THANK YOU FOR ATTENTION!