The Occupational Therapy Clinical Driving Assessment
advertisement
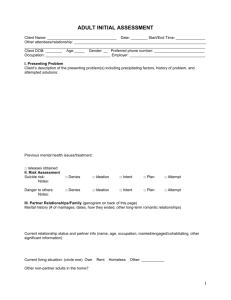
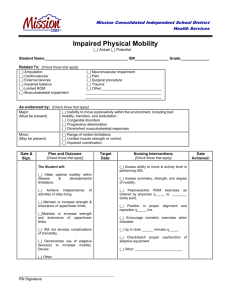
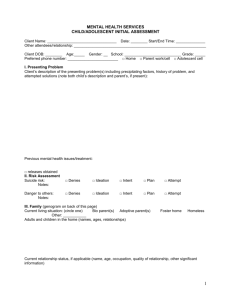
The Occupational Therapy Pre-Driving Clinical Assessment Judith Joseph, OTR, MA, CDRS jajoseph@houstonmethodist.org TOTA MCC November 6, 2014 Objectives • Develop an occupational profile that addresses the client’s driving needs. • Select specific evidence-based assessments and assessment methods to assist in determining driving readiness. • Using the information gathered from the occupational profile, assessments, and goals determine the need to refer client’s to the DRS. • Gain knowledge in the laws and agencies in the state of Texas that determine driving fitness to assist OT practitioners in establishing treatment plans and goals. About the speaker • Introduced to clinical driving evaluations in 1987 • Attended my first ADED conference in 1989? • Developed a pre-driving clinical screen and evaluation in 2010 • Passed CDRS exam August 2013 “So, what are you going to do about driving?” Why should occupational therapist evaluate fitness to drive? Things to consider • • • • There are 20 million drivers in the U.S. 70 and older. Every year, more than 795,000 people in the United States have a stroke. 400,000 individuals estimated to have MS. Approximately 60,000 Americans are diagnosed with Parkinson's disease each year, and this number does not reflect the thousands of cases that go undetected. • One in four adults−approximately 61.5 million Americans−experiences mental illness in a given year • Approximately two million Americans have mild low vision which affects driving and reading. Why Should OT evaluate fitness to drive? • Because driving is an instrumental activity of daily living within the domain of occupational therapy practice. • practitioners should be able to accurately determine who is a safe driver, who is at risk for unsafe driving, and who needs further evaluation by a driving rehabilitation specialist (DRS). AOTA Driving and Community Mobility Occupational Therapy Roles • Generalist: general knowledge and understanding of performance and processing skills related to driving. • Advanced Training: Further education to evaluate the integration of sub-skills associated with driving and provide specific sub-skill training • Specialized Training: Received specialized education, examination, and/or certification. University of Florida What is in our domain of practice? • Musculoskeletal disorders • Neurological impairments • Cognitive impairment • Memory disorders • Visual impairments • Perceptual impairments • Mobility • Mental impairment Consider the diagnosis and resulting impairment Medical condition examples Diagnosis/condition • Sleep apnea • TBI • CVA • Dementia/Alzheimer’s • MS Impairment Risk • Impaired arousal, responsiveness, daytime sleepiness • Attention, orientation, visual field • Visual, cog, motor, visual field • Executive functions • Muscle weakness, sensory loss, fatigue, cognitive or perceptual deficits, symptoms of optic neuritis Sherrilene Classen, Miriam Monahan ADED Conference 2013 Let’s Start with the law! Texas MAB Texas Medical Advisory Board (MAB) • The Texas Medical Advisory Board (MAB) for Driver Licensing was established in 1970 to advise the Texas Department of Public Safety (DPS) in the licensing of persons having medical limitations which might adversely affect driving. • Guidelines established using the following: AMA Physician’s Guide for Determining Driver Limitation Driver Fitness Medical Guidelines (NHTSA) The American Association of Motor Vehicle Administrators Texas Medical Advisory Board/DPS • The ultimate goal is to allow all who can drive safely to do so and to continue to reduce the number and severity of motor vehicle accidents in Texas Functional Ability Profiles • • • • • • • • • • General Debility Cardiovascular disease Syncope Neurological Disorders Psychiatric Disorders Excessive Alcohol use/abuse Drug use/abuse Metabolic Diseases Musculoskeletal Defects Eye Defects • • • • • • • • • Aging Recurrent syncope CVA, Seizures, Dementia MS, Parkinson's, Peripheral neuropathy PTSD DM CP, MD Diplopia, Peripheral vision Visual acuity Where do I start? The Association For Driver Rehabilitation Specialists (ADED) ADED Mission Statement Promoting excellence in the field of driver rehabilitation in support of safe, independent community mobility ADED Best Practices For The Delivery of Driver Rehabilitation Services • Section 1: • Section 2: • Section 3: • Section 4: Interview/Medical History Clinical Visual Assessment Clinical Physical Assessment Clinical Cognitive Assessment www.ADED.net Interview/Medical History • History of Present Illness • Past Medical History • Determine medical consent • Review current medications (side effects) • Assess communication status • Review driving history • License status • Driving goals • Vehicle availability Clinical Visual Assessment ADED recommendation • Visual history • Visual acuity • Field of vision • Other visual skills Possible Deficits • Cataracts, glaucoma, HH, etc. • Feinbloom eye chart, BiVaba, Snellen • Scatomos, HH • Visual short term memory, figure ground, form constancy, visual discrimination, visual scanning skills, High/Low contrast sensitivity Visual Assessments and Observations Assessments • biVABA Brain Injury Visual Assessment Battery for Adults • The cover test • UFOV Useful Field of View • Dynavision • Motor Free Visual Perception Test (MFVPT) • Clock drawing test • Trails B • Pursuits and Saccades Observations • Bumping into walls, furniture, etc. • nystagmus • Head tilting or position • squinting • Position of test paper • Visual scanning efficiency Clinical Physical Assessment • Range of Motion • Strength • Grip strength • Prehension status • Sensation • Proprioception • Coordination (rapid pace walk) • Muscle tone (MAS) • Mobility status (TUG) • Balance (Berg, Teniti,) • Orthotic devices • Mobility aids • Transfer skills • Reaction times (Dynavision) Clinical Cognitive Assessment • Mini Mental State Exam (MMSE) • Short Blessed Test • Clinical Dementia Rating Scale • Montreal Cognitive Assessment (MoCA) • Maze Navigation Test • Single Digit Modality Test (SDMT) • Assessment of Motor Processing Skills (AMPS) Case Study 1: CVA • 76 y/o male with R MCA infarct, s/p thrombectomy, left hemiparesis, DM-2, HTN, BPH, small tear in left supraspinatus. • + multiple falls • Poly pharmacy • Wants to run errands and drive to any appointments • h/o getting lost while driving when blood sugar is uncontrolled • Backed into parked car in grocery store parking lot • Totaled a vehicle 6-7 years ago • Has not driven since onset of stroke Case Study 1 continued: CVA test results • Impaired left peripheral vision • +nystagmus • Rapid pace walk= 10 sec. • Impaired head/neck flexibility • Visual closure, mild impairment • Trail Making B Test- 111sec. • UFOV- unable to complete. Could not see 2nd vehicle • Short Blessed=2 • Multiple angry outburst during testing Case Study 1: recommendations • Referred to U of H low vision clinic by Neuro-ophthalmologist • Complete program at U of H prior to attempting to drive or being referred to CDRS for BWT only after being cleared by Ophthalmologist • Consider driving cessation Case Study 2: Parkinson’s Disease • 91 y/o male with h/o Parkinson’s Disease, loss of balance, peripheral neuropathy, spinal stenosis, lumbar laminectomy • + multiple falls • Using walker with seat • Last eye exam 2-3 years ago • History of falling asleep spontaneously • “minor” accident in parking lot when he could not stop in time when another vehicle pulled out in front of him causing a rear end collision • Totaled a car 3 yrs ago when he backed out of the driveway • Wants to cont. driving without restrictions Case Study 2: Test results • • • • • • • • • • • High low contrast sensitivity intact +nystagmus Failed cover test Bells Test 3:57 sec. Trails B test 161 sec. Right ankle strength 2/5, hip/knee strength 3/5 Limited head/neck flexibility Unable to locate 50% items on UFOV Fell asleep during testing Rapid pace walk= 36 sec. Scored 100% on sign recognition, map reading (items 14-24 on MFVPT) Case Study 2: Recommendations • Patient should not resume driving without a BWT. • High risk for having a crash • Consider driving cessation Case Study 3: Left Hip fracture • 82 y/o female with dx of left hip fx • Has trouble looking over her shoulder, difficulty backing up, and has gotten lost while driving • Wants to be able to drive to the store, etc. She does not plan on driving on the freeway or at night. • She has not driven in 6 months since hip surgery Case Study 3: Test Results • Mild impairment of low contrast vision • Mild impairment of working memory • Impaired visual closure • Trails Making B test: 353 seconds • Impaired visual processing speed • Impaired UFOV • Rapid pace walk- 17 seconds • No errors on clock drawing test • Impaired head/neck flexibility Case Study 3: Recommendations • Further assessment through BWT • Referral to optometrist Case Study 4: MS • 57 y/o female diagnosed with MS. Referred due to recent black out. • h/o ventricular tachycardia, osteoporosis, cataracts, severe scoliosis • + falls • Wears built up right shoe for leg length discrepancy and R AFO • Gets lost while driving, trouble finding and reading signs in time to respond, feeling tired after driving, had “near misses”, bothered by head light glare, trouble looking over shoulder when backing up. • Recently hit a pole at the drive through bank and backed into trash cans at the end of her driveway. Case Study 4: Test Results • • • • • • • • • • • • Impaired visual acuity20/50 in left eye High low contrast intact No deficits noted with visual closure Trials Making B test 73 seconds Mild deficit with visual processing speed on UFOV Mild deficit with working memory No errors on clock drawing test Rapid pace walk 5.8 seconds Right shoulder flex limited to 90 Limited head/neck flexibility 3+/5 strength in Bil hips, and ankles Became fatigued during test Case Study 4: Recommendations • Begin to seek alternative transportation if deficits worsen • Use power chair instead of RW for appointments to conserve energy • Do not drive on unfamiliar trips • Do not drive when fatigued • Consult with MD • Referral to PT • Referral to CDRS for BWT Case Study 5: Impaired memory • • • • • • • • 73 year old female with dx of impaired memory. Cataract removal Currently driving Unable to recall last eye exam Had one speeding ticket Wears a hearing aid (not wearing during exam) No falls Admits to getting lost while driving, feels others drive too fast, being stressed out by driving, difficulty at busy intersections, friends will no longer ride with her. Case Study 5: Test Results • 20/25 binocular vision • Impaired horizontal fixation to right • Bells Test: 1:54, 3 errors • Rapid pace walk- 6 seconds • Scored 14 on the Short Blessed • Trials Making B Test 194 seconds • Intact visual closure, visual processing speed showed mild deficit Case Study 5: Recommendations • Driving should be restricted at best to her immediate neighborhood, however without being able to control what happens such as weather conditions, and changes in traffic volumes driving cessation may need to be considered. If family insist on pt. continuing to drive a referral to CDRS for BWT should be completed. I am not the decider! QUESTIONS?????