Morgan - symposium
advertisement

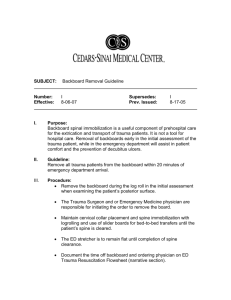
Package, Ship, & Scan? Immobilization and Imaging in the Pediatric Population Morgan Scaggs, NREMT-P KYEMSC Project Director Pediatric Emergency Care Applied Research Network • PECARN • The first federally-funded pediatric emergency medicine research network in the US • Conducts high-priority, multi-institutional research on the prevention and management of acute illnesses and injuries • Supported by cooperative agreements between six academic medical centers, HRSA, MCHB, and EMSC http://www.pecarn.org/ Objectives • discuss risks/benefits of ionizing radiation exposure for children • discuss challenges and potential risks associated with spinal immobilization of children • describe the factors associated with cervical spine injury in children after blunt trauma • discuss plain radiographs vs. CT for identification of cervical injuries • describe the validated prediction rules for identifying children at low risk of clinically important Traumatic Brain Injuries (ciTBI) Can we safely reduce unnecessary immobilization and imaging in the pediatric population without missing clinically significant injuries? We will look at research on: • Potential adverse effects of spinal immobilization in children • Factors associated with c-spine injuries in kids • Plain radiographs vs. CT for identification of c-spine injuries in kids • Identifying children at low-risk for clinically important TBI after minor blunt trauma to reduce CT use Potential concerns regarding immobilization and imaging? • Efficacy • Increased pain • Interference with assessment • Respiratory difficulty • Risk of aspiration • Airway management • Pressure ulcers • Increased intracranial pressure • Distraction forces • Additional forces to area of injury • Tissue hypoxia • Claustrophobia/anxiety • Delays in care/transport • Increased imaging rates • Increased admission rates • Increased risk of radiation induced malignancy Ionizing Radiation Benefits • noninvasive and painless diagnosis of disease and monitoring of therapy • support of medical and surgical treatment planning • facilitates interventional procedures Risks • tissue effects – cataracts – skin reddening – hair loss • a small increase in the possibility that a person exposed to X-rays will develop cancer later in life – Dose dependent – Age at exposure – Gender (women are more radiosensitive than men) – Target organ www.fda.gov/Radiation-EmittingProducts Pediatric Patients • are more radiosensitive than adults (i.e., the cancer risk per unit dose of ionizing radiation is higher) • have a longer expected lifetime for any effects of radiation exposure to manifest as cancer • use of equipment and exposure settings designed for adults may result in excessive radiation exposure if used on smaller patients www.fda.gov/Radiation-EmittingProducts FDA Initiative to Reduce Unnecessary Radiation Exposure from Medical Imaging • Justification: The imaging procedure should be judged to do more good than harm to the individual patient. Therefore, all examinations using ionizing radiation should be performed only when necessary to answer a medical question, help treat a disease, or guide a procedure. The clinical indication and patient medical history should be carefully considered before referring a patient for any imaging examination. • Dose Optimization: Medical imaging examinations should use techniques that are adjusted to administer the lowest radiation dose that yields an image quality adequate for diagnosis or intervention (i.e., radiation doses should be "As Low as Reasonably Achievable"). The technique factors used should be chosen based on the clinical indication, patient size, and anatomical area scanned, and the equipment should be properly maintained and tested. www.fda.gov/Radiation-EmittingProducts Spinal Immobilization in Penetrating Trauma • Haut et al. • The Journal of Trauma; 2010; 68, 1, 115-121 doi: 10.1097/TA.0b013e3181c9ee58 • Retrospective analysis of 45,284 penetrating trauma patients in the National Trauma Data Bank Spinal Immobilization in Penetrating Trauma • Twice as likely to die if immobilized • No benefit for any specific population group • Even with ISS<15, SI was independently associated with significantly decreased survival • GSW with hypotension - 3x increased risk of death with SI • Stab wounds - no statistical impact of SI on mortality Spinal Immobilization in Penetrating Trauma IMPACT: • 1,032 penetrating trauma patients have to be immobilized to potentially benefit 1 patient • For every 66 penetrating trauma patients immobilized, the immobilization potentially contributes to 1 death Spinal Immobilization in Penetrating Trauma Conclusion: pre-hospital spine immobilization is associated with higher mortality in penetrating trauma and should not be routinely used in every patient with penetrating trauma Potential Adverse Effects of Spinal Immobilization in Children • • • • Leonard, J., Mao, J., & Jaffe, D. Prehospital Emergency Care 2012;16:513–518 With the assistance of PECARN Prospective study of children presenting to the ED for evaluation following trauma • 173 Spine Immobilized Children • 112 who met ACS criteria for SI but were not Potential Adverse Effects of Spinal Immobilization in Children • Immobilized children – Had higher median pain scores (3 vs 2) – More likely to undergo cervical radiography (56.6% vs 13.4%) – More likely to be admitted to the hospital (41.6% vs 14.3%) • Comparison groups had similar length of stay in the ED Potential Adverse Effects of Spinal Immobilization in Children • There were differences in between the groups which included age, mechanism of injury and proportion transported by EMS but the comparison groups had comparable PTSs and GCSs • Independent of markers of injury severity, spinal immobilization following trauma in children is associated in some way with increased pain, use of imaging studies to clear the cervical spine of injury, and admission to the hospital • Further study warranted A re-conceptualization of acute spinal care • Mark Hauswald • Emerg Med J 2012;00:1-4. doi:10.1136/emermed-2012-201847 • Analysis of basic physics, biomechanics and physiology • “Discarding the fundamentally flawed emphasis on decreasing post injury motion and concentration on efforts to minimize energy deposition to the injured site….” A re-conceptualization of acute spinal care – Authors Conclusions Specific treatments that are irrational and can be safely discarded include • The use of backboards for transportation • Cervical collar use except in specific injury types • Immobilization of ambulatory patients on backboards • Prolonged attempts to stabilize the spine during extrication • Mechanical immobilization of uncooperative or seizing patients and forceful in line stabilization during airway management NEXUS National Emergency X-Radiography Utilization Study A prospective, observational study involving 21 centers across the United States that evaluated 34,069 stable patients with blunt trauma who were at risk for cervical spine injury 1. Tenderness at the posterior midline of the cervical spine 2. Focal neurologic deficit 3. Decreased level of alertness 4. Evidence of intoxication 5. Clinically apparent pain that might distract the patient from the pain of a cervical spine injury The presence of any one of the above findings is considered to be clinical evidence that a patient is at increased risk for cervical spine injury and requires radiographic evaluation Canadian C-spine Study A prospective, observational study involving 10 centers across Canada that evaluated 8,924 alert and stable patients with blunt trauma who were at risk for cervical spine injury *Alert and stable trauma patients Challenges with Assessment of Children • • • • • Particularly those < 5 years Unreliable patient Communication barrier Fear/anxiety In cases where the child resists immobilization significantly there may be less risk in providing a gentle, comfortable ride. Forcing a fighting child into immobilization may cause greater harm. Factors Associated With Cervical Spine Injury in Children After Blunt Trauma • • • • Leonard et al. Ann Emerg Med. 2011;58:145-155 Cervical spine injuries in children are rare Immobilization and imaging for potential cspine injury after trauma are common • Risk factors for c-spine injury have been developed to safely limit immobilization and imaging in adults but not children Factors Associated With Cervical Spine Injury in Children After Blunt Trauma • Case-control study of children <16, with blunt trauma, who received c-spine radiographs at 17 hospitals in the PECARN Network • Reviewed records of – – – – 540 children with c-spine injury 1,060 random controls 1,012 mechanism of injury controls 702 EMS controls • Identified an 8-variable model for cervical spine injury in children after blunt trauma Predictors of Cervical Spine Injury In Children • • • • • • • • Altered Mental Status Focal Neurological Findings Neck pain Torticollis Substantial torso injury Conditions predisposing to cervical spine injury Shallow-water diving accidents High-risk MVCs (ejections, high speeds, etc.) Predictors of Cervical Spine Injury In Children • • • • • • Altered Mental Status Focal Neurological Findings Neck pain Torticollis Substantial torso injury Conditions predisposing to cervical spine injury • Shallow-water diving accidents • High-risk MVCs • 98% sensitive for injury – One indicator present in 98% of cervical spine injuries • 26% specific – Presence of one indicator signifies only a 26% chance of injury Child Safety Seats • • • • Are not spinal immobilization devices Prevent complete assessment May prevent proper positioning May not be possible to properly secure within the ambulance • May not be safe to use after a crash Utility of Plain Radiographs in Detecting Traumatic Injuries of the Cervical Spine in Young Children • Nigrovic et al. for the PECARN Cervical Spine Study Group • Pediatric Emergency Care, Volume 28, Number 5, May 2012 • Retrospective cohort of children <16 with blunt trauma-related bony or ligamentous cervical spine injury evaluated at 1 of 17 PECARN hospitals Utility of Plain Radiographs in Detecting Traumatic Injuries of the Cervical Spine in Young Children • Cervical injuries in children are rare • Ionizing radiation exposure 30x higher in CT vs plain radiography • Adult studies demonstrated a sensitivity for Cspine injury of 80% for single cross-table view and >90% for a 3-view series • Is this applicable in children? (different injury patterns and greater anatomic variability) Utility of Plain Radiographs in Detecting Traumatic Injuries of the Cervical Spine in Young Children Specifically excluded SCIWORA • 206 patients enrolled – 186 had adequate plain radiographs – 168 had definite or possible cervical spine injuries identified by plain radiographs for a sensitivity of 90% (95% CI, 85%-94%) – C-spine radiographs failed to identify 15 children with fractures and 3 with ligamentous injury Utility of Plain Radiographs in Detecting Traumatic Injuries of the Cervical Spine in Young Children • Of those “missed” – Half (9) had either altered mental status or focal neurological findings – 8 children had fractures and 1 had isolated ligamentous injury, none required neurosurgical intervention or were left with persistent neurological deficits • Conclusion: Plain radiographs had a high sensitivity for cervical spine injury in this pediatric cohort • Advanced imaging likely provides a higher sensitivity, it often comes with increased costs and significantly higher radiation exposure, need further study to determine which children will benefit Identification of children at very low risk of clinicallyimportant brain injuries after head trauma: a prospective cohort study • Kupperman et al. for PECARN • Lancet 2009; 374:1160-70, published online September 15, 2009 doi:10.1016/S0140-6736(09)61558-0 • Goal – to identify those at low risk for ciTBI and validate a prediction rule to guide decision for CT Identification of children at very low risk of clinicallyimportant brain injuries after head trauma: a prospective cohort study • Prospective cohort study of patients younger than 18 years presenting within 24h of head trauma with GCSs of 14-15 in 25 EDs in the pediatric research network • Enrolled and analyzed 42,412 children – 25% (10,718) were < 2 years of age • Derived and validated age-specific prediction rules for ciTBI Identification of children at very low risk of clinicallyimportant brain injuries after head trauma: a prospective cohort study • Severe mechanism of injury – MVC with patient ejection, death of other occupant, or rollover – Pedestrian or bicyclist without helmet struck by a motorized vehicle – Falls of more than 3 feet (< 2 yrs) or 5 feet (2+ yrs) – Head struck by a high-impact object Identification of children at very low risk of clinicallyimportant brain injuries after head trauma: a prospective cohort study Suggested CT algorithm for children younger than 2 years Negative predictive value for ciTBI of 1176/1176 (100.0%, 95% CI 99.7-100.0) And sensitivity of 25/25 (100.0%, 86.3-100.0) of 694 CT-imaged patients in this low-risk group Identification of children at very low risk of clinicallyimportant brain injuries after head trauma: a prospective cohort study Suggested CT algorithm for children aged 2 years and older Negative predictive value for ciTBI of 3798/3800 (99.95%, 99.81-99.99) And sensitivity of 61/63 (96.8%, 89.0-99.6) of 2223 CT-imaged patients in this lowrisk group Identification of children at very low risk of clinicallyimportant brain injuries after head trauma: a prospective cohort study • ¶ Risk of ciTBI exceedingly low, generally lower than risk of CT-induce malignancies, CT scans are not indicated for most patients in this group • Neither rule missed neurosurgical need in validation populations • These validated rules identified children at very low risk of ciTBI for whom CT can routinely be obviated Do Children With Blunt Head Trauma and Normal Cranial Computed Tomography Scan Results Require Hospitalization for Neurologic Observation? • Holmes et al. and the TBI Study Group for PECARN • @2010 by the ACEP doi:10.1016/j.annemergmed.2011.03.060 • Prospective, multicenter observational cohort study of children <18 yrs. with blunt head trauma, GCSs of 14-15 and normal ED CT scan results • 13,543 children enrolled Do Children With Blunt Head Trauma and Normal Cranial Computed Tomography Scan Results Require Hospitalization for Neurologic Observation? • Of the 11,058 patients discharge home from the ED – 197 (2%) received subsequent CT or MRI – 5 (0.05%) had abnormal CT/MRI results – None (0%; 95% CI 0%-0.03%) received a neurosurgical intervention Do Children With Blunt Head Trauma and Normal Cranial Computed Tomography Scan Results Require Hospitalization for Neurologic Observation? • Of the 2,485 hospitalized patients – 137 (6%) received subsequent CT or MRI – 16 (0.6%) had abnormal CT/MRI scan results – None (0%; 95% CI 0%-0.2%) received a neurosurgical intervention Do Children With Blunt Head Trauma and Normal Cranial Computed Tomography Scan Results Require Hospitalization for Neurologic Observation? • The negative predictive value for neurosurgical intervention for a child with an initial GCS score of 14-15 and a normal CT scan result was 100% (95% CI 99.97%-100%) • Hospitalization of children with minor head trauma after normal CT scan results for neurological observation is generally unnecessary morgan.scaggs@kctcs.edu