Y. pestis
advertisement

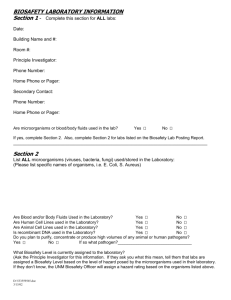
Bioterrorism Agent Case Studies Beth Schweitzer MT(ASCP), SM Microbiology Specialist Website: www.nphl.org NPHL Nebraska Public Health Lab Case Format Lack of pertinent patient information Travel history Occupation Symptoms Duration of Illness Case Format Cultures are set according to NPHL Operating Procedures BAP Chocolate MacConkey Thioglycolate Broth Zoonotic Diseases Naturally occurring Cases in NE Safety concerns for laboratorian Manuel’s Mystery Blood Cultures drawn on 16 y/o Hispanic male Instrument flags bottles positive at day 4 Gram stain: NOS Bottles blind subbed and placed back on machine Bottles discarded on day 5 (standard operating procedure) Con’t BAP and Choc show a haze of growth at 48 hours ( 6th day of original Blood culture) Gram stain: tiny gram- negative coccobacilli What organisms should you be thinking!!! Haemophilus Pasturella Oligella Bordetella Brucella Francisella Acinetobacter Psychrobacter Think Biosafety In a biosafety cabinet you perform following: Identification for Haemophilus Rapid NH Quad/Tri Plate Staph streak Think Biosafety Reactions do not fit the pattern for Haemophilus!! What now? Think Biosafety Do not perform automated commercial identification on slow growing-GNCB that do not grow on MAC/EMB. The risk of aerosols is too high! Think Biosafety In a biosafety cabinet you perform following: Urease slant (Pos in 2 hours) Tube motility (Neg at 48 hours) TEST Oxidase Motility Urease Nitrate BAP X/V Brucella Bordetella Acinetobacter Psychrobacter Oligella Haemophilus + 95% + + + V + V - + + V + + V + + V + + + + + + + - + What organism can’t we rule out? Brucella spp. Brucella spp. - Biosafety Alert: Brucellosis was the most commonly reported laboratory-associated bacterial infection. Cases have occurred in clinical laboratory settings by “sniffing” cultures, direct skin contact with cultures, and aerosol generating procedures (e.g. culture manipulation) Brucellosis: Infective dose:10 -100 organisms Incubation period: 5 days - > 6 months Duration of illness: weeks to months Fever, profuse sweating, malaise, headache and muscle/back pain. NO Person to person transmission Mortality: <5% Persistence of organism: very stable Brucella spp.-Specimen Selection: Serum Blood or bone marrow The diagnosis of brucellosis is frequently achieved by serology. An acute & convalescent phase specimen should be collected (21 days apart) Most often isolated from these Tissue (spleen, liver) Occasionally isolated Brucella spp. – Technical hints Oxidase positive, rapid urease positive, non-motile, slow growing gram negative-coccobacillus Naturally occurring Patient was a visitor from Mexico and had ingested unpasteurized goat cheese Loretta’s Lymph Lymph node aspirate from a 35 y/o female Gram stain: Moderate WBC’s Few Gram- negative rods Growth at 24 hours Tiny (1-2 mm) grey colonies on BAP and Choc Non-lactose fermenter on Mac Biochemical tests Oxidase (-) Indole (-) Use commercial ID system What organism could it be? Fits Enterobacteriaceae pattern Without patient history hard to create a differential Y. pestis – commercial ID systems Included in the data base of MicroScan, Vitek, and API 20E.. etc True accuracy not yet determined 60% of California’s Y. pestis ID’s are from commercial systems Y. pestis – commercial ID systems If ID as Y. pestis – send to NPHL May ID as Shigella ssp, H2S- negative Salmonella, Acinetobacter, or Y. pseudotuberculosis Biochemically inert nature of organism Y. pestis –commercial ID systems How do we know when to question ID results?? Source Colony morphology H2S neg Salmonella Shigella characteristics Inpatient/outpatient status-nosocomial infection. Plague Epidemiology: During 1988-2002, 112 human cases were reported from 11 western states 30% of cases are in Native Americans in the Southwest. 15% case fatality rate 80% of cases occur in summer and near the patient’s residence- FLEAS Y. pestis - Specimen Selection: Specimen selection is important Bubonic Bubo - lymph node aspirate Septicemic - blood - organisms may be intermittent. Take three specimens 10-30 minutes apart Pneumonic Sputum/throat Bronchial washings Y. pestis - Gram stain from sputum Small, gram-negative rods Y. pestis - Direct Culture Growth on Agar Plate: Y. pestis - Growth in Broth: Thioglycolate Broth (may see from original specimen set-up) Do not shake tubes Observe suspended flocculent clumps on side and bottom of tube. Broth remains clear May also happen with Y. pseudotuberculosis or S. pneumoniae Y. pestis – Growth in Broth culture: Y. pestis Y. pseudotuberculosis Y. pestis - Technical Hints: Small gram-negative, poorly staining rods from blood, lymph node aspirate, or respiratory specimens, BLOODY SPUTUM Naturally Occurring Couple from New York City infected by flea bites on trip to New Mexico Returned home to NYC before becoming ill Bob’s Booboo Aerobic culture is collected from wound on the hand of a 45 y/o male Gram stain: NOS Mod WBC Con’t At 48 hours there is slight haze growth on the BAP and Choc Gram stain: faintly staining gram- negative coccobacilli What organisms should you be thinking!!! Haemophilus Pasturella Oligella Bordetella Brucella Francisella Acinetobacter Psychrobacter Actinobacillus Think Biosafety Do not perform automated commercial identification on slow growing-GNCB that do not grow on MAC/EMB. The risk of aerosols is too high! Think Biosafety In a biosafety cabinet growth you perform the following: Oxidase (Negative) Manual commercial identification system No identification Reisolate to BAP and Choc No growth on BAP after reisolation What to do now???!?!?! Haemophilus is a likely organism Haemophilus quad plate is set for identification No growth is seen Its NOT Haemophilus… What Now? In a biosafety cabinet the following tests are performed: Motility (Negative at 24 hours) Urease (Negative at 24 hours) B-lactamase (+) What organism can’t we rule out? Francisella F. tularensis – Gram stain: Poorly staining, tiny Gram-negative coccobacilli Francisella/E. coli F. tularensis – growth characteristics: Will grow initially on sheep blood agar, chocolate agar and Thayer-Martin agar, but poorly or not at all on sub Grows slowly at 35oC, poorly at 28oC 24 hours on BAP and Choc gray-white, translucent colonies usually too small to be seen individually F. tularensis – growth characteristics: Thayer Martin is a good selective media from a mixed culture F. tularensis - Colony morphology F. tularensis SCHU strain on cysteine heart agar with 9% sheep blood (left) and chocolate agar (right), 72 hours F. tularensis - Colony Morphology F. tularensis NV972342 isolate on CHAB agar. Opalescent purplish sheen under oblique light F. tularensis: Infective dose: 10-50 organisms Very Low ! Incubation period: 1-21 days (average=3-5 days) Duration of illness: ~2 weeks NOT Contagious person to person Mortality: treated: low untreated: moderate Persistence of organism: months in moist soil Vaccine efficacy: good, ~80% Not presently available Francisella – specimen collection Serum- like Brucella most often diagnosed by serology testing, not by culture Ulceroglandualar Pneumonic Wound culture Sputum Lymph node aspirate Typhoidal Blood CSF sputum F. tularensis - Technical Hints: Tiny, gram-negative coccobacilli from blood, lymph node aspirate, or respiratory specimens Blood isolates that will grow slowly on chocolate agar but poorly or not at all on blood agar in 24 hours Naturally Occurring Patient is a veterinarian Gordo’s Glass Jaw Anaerobic culture received from jaw of 67 y/o male Gram stain: large chaining Gram- positive rods What could you do now? Visualize capsule Perform India Ink directly from sample to visualize capsule Will only see capsule directly from specimen It will not be visible upon sub-culture B. anthracis – Colony Morphology: Colonial morphology of 18-24hr @ 35 C: Well isolated colonies are 2-5 mm in diameter Flat or slightly convex, irregularly round Edges: slightly undulate, often curly tailing edges- “Medusa Head” Ground glass appearance “Sticky” or “Tenacious” consistency….stands up like beaten egg whites Presence of Spores Spores will only be seen after incubation in ambient conditions Capsule B. anthracis - colony on SBA Sticky colonies Bacillus anthracis – India Ink Anthrax: Inhalational Infective dose Naturally occurring= 8,000 - 15,000 spores Weaponized = ??? maybe 10 to 100 spores Incubation period = 1-6 days Duration of illness = 3-5 days Fever, malaise, and fatigue Short period of improvement = up to 2 days Abrupt respiratory distress…death <24hrs NO Person to person transmission Anthrax- Specimen Selection Inhalational: Sputum and Blood Cutaneous: Vesicles and Eschar Gastrointestinal: Stool and Blood B. anthracis- Technical Hints: Catalase positive, non-motile, spore forming Gram- positive rods Naturally Occurring Patient was a rancher from North Dakota that recently had 5 cows die of anthrax