Tonsillitis and Adenoiditis
advertisement
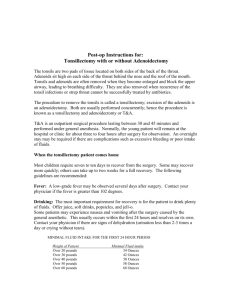
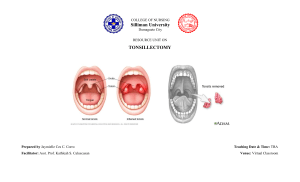
Tonsillitis and Adenoiditis Islamic University Nursing College Tonsillitis – Inflammation of tonsils. – Masses of lymphoid tissue in pairs – Often occurs with pharyngitis – Characterized by fever, dysphagia, or respiratory problems forcing breathing to take place through nose Nurse Alert! Key to understanding prevention of URI is careful hand-washing and avoiding exposure to infected persons. Nurse Alert! The nurse should remind the child with a positive throat culture for strep to discard their toothbrush and replace it with a new one after they have been taking antibiotics for 24 hours Causes • Viral. • Bacterial ( group A beta hemolytic streptococci (GABHS). Clinical Manifestations • Tonsillitis – – – – – – Fever Persistent or recurrent sore throat Anorexia General malaise Difficulty in swallowing, mouth breather, foul odor breath Enlarged tonsils, bright red, covered with exudate • Adenoiditis – Stertorous breathing - snoring, nasal quality speech – Pain in ear, recurring otitis media Surgical treatment • Tonsillectomy. If recurrent. • Not recommended before 3 years of age due to: • Excessive blood loss. • Tonsils grow back. Nursing Care for the Tonsillectomy and Adenoidectomy Patient Post-operative Care • Providing comfort and minimizing activities or interventions that precipitate bleeding – – – – – Place on abdomen or side until fully awake Manage airway Monitor bleeding, esp. new bleeding Ice collar, pain meds Avoiding fluids until fully awake --then liquids and soft cold foods. Avoid citrus juices, milk – Do not use straws or put tongue blade in mouth, no smoking (in teenagers). Nurse Alert for Post-Op T/A surgery • Most obvious sign of early bleeding is the child’s continuous swallowing of trickling blood. • Note the frequency of swallowing and notify the surgeon immediately Epiglottitis • Bacterial form of croup (H influenza) with unique symptoms and treatment • Bacterial infection invades tissues surrounding the epiglottis • Epiglottis becomes edematous, cherry red and may completed obstruct airway • Progresses rapidly, child is unable to swallow, drooling Cardinal signs and symptoms • May have had mild URI few days prior • • • • • Drooling Dysphasia Dysphonia Distressed respiratory efforts Tripod position: supported by arms, chin thrust out, mouth open ER Management • NEVER leave child unattended • Don’t examine or culture throat or start IV/Blood samples • Patent airway ASAP • Monitor oxygenation status, (continuous pulse ox, humidified O2) • Antipyretics suppository • Calm the parent! Explain what is going on…a calm parent=calmer child! • OR- intubation • Throat & blood cultures done after intubation • Usually extubated after 48h • Antibiotics for 7-10 days • Discharge Nursing Interventions on unit once stable • Continually assess for s/s of respiratory distress • Maintain pulse ox above 95% with PaO2 between 80-100mmHg • Maintain patent airway • Position for comfort (never force to lie down) • Relieve anxiety • Monitor temp (antipyretics, ABX)