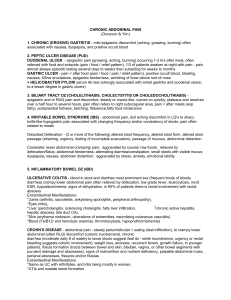
The Problem of Pain
advertisement
The Problem of Pain Approach to Abdominal Pain Jason Phillips, MD ER approach to abdominal pain Chief complaint: abd pain Labs: CBC, chem, LFTs, lipase CT abdomen History Possible PE How do you approach a workup for abdominal pain What are the most likely possibilities? How do you organize your thoughts? The Problem of Pain Neurologic basis of pain Why is it difficult to localize? Why does the intensity of the pain vary? General overview of approaching a patient with abdominal pain Pain syndromes Neurologic basis of abdominal pain Pain receptors respond to Mechanical stimuli Chemical stimuli Nociception mechanical receptors are located on serosa, within the mesentery, in the GI tract wall in the myenteric plexus (Auerbach plexus) submucosal plexus (Meissner plexus) Neurologic basis of abdominal pain Mucosal receptors respond to chemical stimuli Substance P, serotonin, histamine, and prostaglandins Chemical stimuli are released in response to inflammation or ischemia Two basic problems with abdominal pain Localization of visceral pain Intensity of pain response Localization of visceral pain Visceral pain localizes to midline Bilateral, symmetric innervation Afferent fibers celiac, superior mesenteric, or inferior mesenteric ganglion Localizes: epigastrium, periumbilical, and lower abdomen Localization of visceral pain Exceptions to the bilateral rule Gallbladder Ascending and descending colon Although bilaterally innervated, they have predominant ipsilateral innervation Localization of visceral pain Referred pain Somatic fiber “cross-talk” Activate same spinothalamic pathways referred pain as the cutaneous dermatome sharing the same spinal cord level (Gallbladder – scapula) Results in aching pain with skin hyperalgesia and rigidity Intensity of pain response Threshold for perceiving pain from visceral stimuli has marked individual variability Balloon distension experiment in IBS History MOST IMPORTANT CLUE to the source of abdominal pain Type of pain Visceral = dull, aching, poorly localized Parietal = sharp, well localized Referred pain History General location Generalized, RUQ, epigastric, LUQ, periumbilical, RLQ, LLQ, and ‘migratory’ General region localizes organs/structures to include in the DDX Radiation of pain (e.g., acute pancreatitis) History Onset of pain Most gradual, steady crescendo (e.g., cholecystitis) Abrupt, “10/10” – suggestive of perforation Quality of pain Colicky (comes and goes) – e.g., gastroenteritis Steady – (e.g., acute pancreatitis; biliary colic is a misnomer) Burning History Severity of pain Generally corresponds to severity of illness However, marked patient variability (“12/10 pain” is often functional or has functional overlay) Aggravating or Relieving factors Eating (mesenteric ischemia vs PUD) Position changes (acute pancreatitis, peritonitis) History Associated symptoms Nausea/vomiting Weight loss Changes in bowel habits Physical exam: Acute abdomen or not? General appearance and Vital signs Abdominal exam Auscultation Bowel sounds present? High pitched sounds of obstruction Stethoscope palpation Percussion Tympany = distended bowel Most humane test for rebound tenderness Physical exam: Acute abdomen or not? Palpation: Acute abdomen or not? Peritoneal signs Rebound tenderness Mass? Hernia Abdominal wall maneuvers Leg lift maneuvers (Carnett’s sign) Abdominal crunch Further evaluation Directed at pain syndromes Labs Imaging Is the pain functional or not? Functional abdominal pain Can be difficult to distinguish from organic pain Can only be labeled as functional when organic causes are excluded Can superimpose on organic pain Should not cause Weight loss, Anemia, GI bleeding, Fever, Night sweats Is it functional or not? Clues that are suggestive of functional Atypical history RUQ that lasts 20 sec is not biliary colic Dyspesia that worsens with a PPI Overly dramatic descriptions of pain “It feels like a knife stabbing me over and over and then something is pushing inside out” Hyperbolic intensity “11/10 exam epigastric pain” with a benign abd Is it functional or not? Clues that are suggestive of functional Absence of nocturnal symptoms Exacerbated by stress Distractible exam “Gut feeling” Pain syndromes Irritable Bowel Syndrome Prevalence: 10-15% of overall population Only ~15% of patients seek medical care 25-50% of gastroenterology visits Annual healthcare cost: $1.7 billion Irritable Bowel Syndrome ROME criteria: 12 weeks or more of abdominal pain/discomfort in the last 12 months (does not have to be consecutive) Two or more features: 1. 2. 3. Relieved with defecation Change in frequency of stool Change in appearance of stool Irritable Bowel Syndrome 3 types of IBS patients Constipation-predominant Diarrhea-predominant Alternating Irritable Bowel Syndrome What is the normal range for frequency of bowel movements? Rule of 3s: - Normal = Anywhere from 3x per week to up to 3x per day Irritable Bowel Syndrome Pathophysiology Alterations in motility Visceral hyperalgesia Postinfectious IBS – lymphocytic infiltration of myenteric plexus? Irritable Bowel Syndrome How do you prove its only IBS? Rome criteria positive for IBS No alarm features and mild symptoms, reassurance and treatment of symptoms Alarm features or severe symptoms, consider referral to GI Upper abdominal pain Biliary disease Dyspepsia Pancreatitis Gastroparesis Other Upper abdominal pain: Biliary disease 1. 2. 3. Most common location – epigastric NOT RUQ Steady onset; last hours (not minutes or seconds) Can radiate to right scapula Biliary colic Cholecystitis Acute cholangitis Upper abdominal pain: Biliary disease Workup: Labs: When are liver tests abnormal? Imaging: What is the most sensitive imaging study for biliary tract disease? What are its limitations? Upper abdominal pain: Biliary disease Labs: LFTs increase with choledocholithiasis (first transaminases, then AP/T Bili) Ultrasound: Sensitivity Cholecystitis HIDA Gallstones Biliary dilation Choledocholithiasis dilated CBD) Specificity 88% 89% 97% 90% 84% 99% 55-91% 50 vs 75% (nondilated vs Upper abdominal pain: Dyspepsia Dyspepsia = “persistent or recurrent abdominal pain or discomfort in the upper abdomen.” Vague diagnosis that includes a long DDX Upper abdominal pain: Dyspepsia 80-100% of ‘dyspepsia’ is a acid-related phenomenon or functional Usually an outpatient problem Peptic ulcer pain = epigastric, burning or hunger-like, worse between meals, relieved with food, nocturnal pain, associated nausea Upper abdominal pain: Dyspepsia GERD = heartburn (retrosternal burning), water brash (acid taste in mouth), regurgitation, and sensation of dysphagia Upper abdominal pain: Dyspepsia Functional dyspepsia = same symptoms but no organic etiology can be found 12 weeks over last 12 months Not relieved with BM or associated with alterations in BMs (i.e., NOT IBS) Upper abdominal pain: Dyspepsia Best test? 3 strategies Empiric PPI H pylori – test and treat EGD Gastroparesis Often overlooked as a cause for epigastric pain Gastroparesis symptoms Nausea 93% Abdominal pain 90% Epigastric burning, vague, cramping Early satiety 86% Vomiting 68% Gastroparesis 60% report pain is worse after eating 80% reports pain interrupted sleep Vomiting food hours later Look for important historical clues Diabetes Meds (narcotics, anticholinergics) Recent viral gastroenteritis CNS disease Amyloid, scleroderma Gastroparesis Workup EGD or UGI – rule out GOO Gastric emptying scan Upper abdominal pain: Pancreatitis Acute Pancreatitis = acute epigastric pain that radiates to back, constant, severe, rapid onset within 1 hour, lasts days, associated nausea/vomiting, relieved with sitting forward; assoc restlessness Rarely diffuse pain, RUQ, or LUQ Upper abdominal pain: Pancreatitis Diagnosis is made when you have at least 2 of the 3 criteria: - Typical pancreatitic pain - Elevation in amylase and lipase - Abnormal imaging Upper abdominal pain: Pancreatitis Chronic pancreatitis = similar pain, less severe and onset 20-30 minutes after a meal, can be episodic (early in disease course) or constant (late finding) Associated malabsorption (pancreatic exocrine insufficiency) and diabetes (endocrine insufficiency) Steatorrhea does not occur until 90% or more of pancreatic function is lost Upper abdominal pain: Other causes Acute MI Pneumonia Splenic abscess or infarct Lower abdominal pain Appendicitis Diverticular disease IBS Crohn’s disease Hernia Other Lower abdominal pain Appendicitis = begins as periumbilical pain that localizes to RLQ (McBurney’s point) Initially visceral pain (superior mesenteric ganglion) RLQ when inflammation extends to peritoneal surface (parietal pain) Pain evolves over hours Exam: peritoneal irritation (rebound) + fever Labs: Elevated WBC Lower abdominal pain Diverticulitis = usually LLQ abdominal pain Constant w insidious onset Worsening over days Associated symptoms of fever and worsening constipation Lower abdominal pain Exam: spectrum of severity Mild LLQ tenderness Severe LLQ rebound Labs: Elevated WBC Imaging Lower abdominal pain 70% of diverticulitis in Western countries in left sided. What group of patients usually have right sided diverticultitis (~75%)? Do seeds cause diverticulitis and should they be avoided? Lower abdominal pain IBD can give lower abdominal pain with diarrhea, weight loss, hematochezia, fever These clues are more obvious However, 10% of patients with Crohn’s disease will NOT have diarrhea and can present with abdominal pain RLQ ileocecal CT, colonoscopy, SBFT Lower abdominal pain Hernia = weakness or disruption of the abdominal wall Indirect: at the internal ring Direct: Hesselbach’s triangle Umbilical Epigastric Incisional Lower abdominal pain Groin hernias pain or dull pressure with lifting, straining, or increasing intrabdominal pressure; worse with prolonged standing and at end of day Physical exam is crucial Outright pain at rest is concerning for strangulation Lower abdominal pain If in doubt, consult surgery for an opinion If a hernia is bright red and impossible to reduce, call a surgeon immediately Lower abdominal pain: Non-GI causes Nephrolithiasis Colicky pain (spasms lasting 20-60 mins) Site depends on location of stone (flankgroin) UA: hematuria (neg in 20-30% of cases) CT renal stone protocol Lower abdominal pain: Non-GI causes Pelvic inflammatory disease Pelvic pain during menses or coitus Onset during of shortly after menses Bilateral Usually less than 2 weeks Exam critical: speculum and bimanual exam Diffuse abdominal pain Gastroenteritis IBS Obstruction Mesenteric ischemia Diffuse abdominal pain Viral gastroenteritis = colicky abdominal cramps, watery diarrhea, and nausea/vomiting Incubation 24-48 hours Symptoms begin with abdominal cramps and/or nauseamost have vomiting and watery diarrhea Mild fever, myalgias Lasts 48-72 hrs Diffuse abdominal pain Obstruction Periumbilical pain with paroxysms of cramps occurring every 4-5 minutes Abdominal distension Nausea Obstipation may be delayed up to 24 hours History of abdominal surgery or malignancy Diffuse abdominal pain Obstruction Exam: distended appearance, tympanic, high pitched tinkle or large bowel sounds NGT decompression Abdominal x-rays – supine and upright Ischemia Acute mesenteric ischemia Embolism Thrombosis Vasospasm Chronic mesenteric ischemia Intestinal angina Can be difficult to diagnose Acute mesenteric ischemia Embolic sudden onset of severe, diffuse pain Writhing in pain Abdominal exam feels benign - :pain out of proportion to exam” Be suspicious in the right patient: atrial fibrillation, mechanical heart valves, age Acute mesenteric ischemia Thrombotic and non-occlusive insidious onset of pain Labs: nonspecific until late in the course Imaging: mesenteric angiogram Questions?