Culturally Competent Care
advertisement

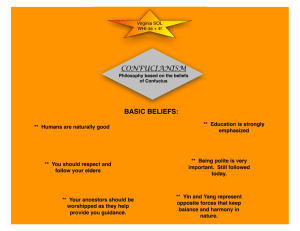
Keri Holmes-Maybank, MD March, 2013 Medical University of South Carolina Residents will learn the definition of cultural competency. Residents will learn the importance of cultural competency. Residents will learn questions to use to facilitate interviews in culturally diverse populations. Residents will identify pitfalls to avoid when practicing cultural competency. Minority populations receive a lower level of health care. Successful care of minority populations requires cultural competency. By recognizing cultural differences a respectful relationship between the provider and patient may begin. It is important to avoid stereotyping when practicing cultural competency. Culturally competent care leads to greater patient satisfaction and less errors. Different languages Different explanatory models of the cause and treatment of illness Religious beliefs Ways of understanding the experience of suffering and dying Misperceptions secondary to lack of cultural competence lead to ◦ ◦ ◦ ◦ Poor interactions Mistrust Anger with patients and their families Unwanted clinical outcomes Ethnic minorities ~30% of the population >329 languages 32 million do not speak English at home Foreign-born: 50% Latin America, 25% Asia, 25% Europe, Canada, etc. By 2050 ethnic minorities will be the majority Multi-factorial Minority communities ◦ ◦ ◦ ◦ ◦ ◦ More socioeconomically disadvantaged Lower levels of education Higher rates of occupational hazards Greater environmental hazards Overrepresented among underinsured Higher rates of disease, disability, death Quality of Care - even when adjusted for access (insurance and income) ◦ Utilization of cardiac diagnostic and therapeutic procedures ◦ Analgesia for pain control ◦ Surgical treatment of lung cancer ◦ Referral for renal transplant ◦ Treatment of pneumonia and congestive heart failure ◦ Immunizations ◦ Mammograms Cardiac procedures Analgesic prescriptions Cancer treatment Depression anxiety treatment HIV treatment Renal disease Asthma Pharmacies in Black neighborhoods are less like to stock and fill narcotics Lack of diversity in health care providers Systems of care poorly designed to meet needs of diverse patient populations Poor communication between providers and patients of different racial, ethnic or cultural backgrounds Lack of cultural competency Department of Health and Human Services’ Office of Minority health ◦ Culturally and Linguistically Appropriate Standards of Services(CLAS) Healthy People 2010 Task Force on Community Preventative Services Accreditation Council for Graduation Medical Education - “Tool for the Assessment of Cultural Competence Training” TACCT Liaison Committee for Medical Education “Faculty and students must demonstrate an understanding of the manner in which people of diverse cultures and belief systems perceive health and illness and respond to various symptoms, diseases, and treatment.” Cultural competence is a complex, life-long process. Describes the ability of systems to provide care to patients with diverse values, beliefs, and behaviors, including delivery to meet pts social, cultural, and linguistic needs. Cultural competence refers to knowledge, skills(communication, interpreters, attention to nonverbal communication), and cultural sensitivity. Capacity to identify, understand, and respect values and beliefs of others Consider how these factors interact at multiple levels of the health care delivery system Devise interventions that take these issues into account Expansion of cultural knowledge Disease prevalence, incidence, and treatment outcomes Be aware of how culture shapes patient values, beliefs, and world views Acknowledge that differences exist Respect the differences Maintain a non-judgmental attitude toward unfamiliar beliefs and practices Be willing to negotiate and compromise when world views conflict Differences are not accepted, appreciated, explored, or understood = disagreements, difficult interactions, or decisions the physician does not understand Creates barriers to accessing health care Patients may delay or refuse care ◦ ◦ ◦ ◦ Mistrust Perceived discrimination Negative experiences with health care system Historical events (slavery and abuses in research Comprehensive and compassionate care Reduces unnecessary test Reduces inappropriate use of services Reduces the incidence of medical errors Assures the provision of appropriate services Improves health outcomes Increases efficiency staff Increases adherence Greater patient satisfaction Trust is critical to cross-cultural cooperation Addressing and respecting cultural differences will likely increase trust Integrated pattern of learned beliefs and behaviors ◦ ◦ ◦ ◦ ◦ ◦ ◦ ◦ Language Thoughts Communication Ways of interacting Views on roles and relationships Actions Practices/Customs Values Race Ethnicity Nationality Language Gender Sexual orientation Socioeconomic status Physical and mental ability Occupation Influenced by religious or spiritual concerns Religious and medial perspectives are different and could come into conflict though they do not need to be contradictory Religious beliefs and practices vary from individual within same religion or denomination Only God has knowledge about and power over life and death Fundamentally shapes the way people make meaning out of illness, suffering and dying ◦ How symptoms are identified and communicated ◦ Beliefs about causality, prognosis, prevention, treatment options ◦ Threshold for seeking care ◦ Expectations of care ◦ Adherence ◦ Ability to understand the treatment strategy Family, social, and cultural networks reinforce Cultural system with specific language, values, and practices that must be translated, interpreted and negotiated with patient and families. Biomedical world view of professional training creates values, perspectives, and biases. Traditional H&P does not facilitate learning how patients make decisions Right of patient to be informed about condition, possible treatments, ability to choose or refuse life –prolonging medical care, advance directives Truth-telling is not the norm in much of the world Can be seen as cruel and potentially harmful May lose hope and suffer unnecessary physical and emotional distress Some believe hastens death Disease is the objective, measurable pathophysiology that creates the illness Illness includes the assumed etiology—be it natural (fall that breaks a bone), supernatural (God’s will, witches, or malevolent spirits), or metaphysical (bad airs or seasonal changes for which one is unprepared) The assumed etiology establishes the groundwork for negotiating objectives of care Develop communication skills Aware of the specific beliefs and practices Be sensitive cultural differences Accept the patient values and world views as starting points for the MD-PT relationship Humility and genuine concern Friendly and helpful Avoid medical jargon Checking for understanding Use translator Ask specific questions - Inquire about values Self-reflection to address own bias = barriers Respect = trust = confide Respectful emotionally supportive dialogue can overcome racial barriers Disregarding importance of culture to patient’s view and beliefs “Cultural imperialism” - giving greater meaning to values and disregard patient’s MD’s may misinterpret non-verbal cues without knowing cultural context Family/untrained interpreters may misinterpret medical phrases, censor sensitive or taboo topics, or filter/summarize discussion Interrupting Failing to maintain appropriate physical distance Failing to listen Assuming words mean the same to patient Stereotyping Appearing disrespectful Great diversity with in ethnic and cultural groups Individuals w differ socio-cultural factors: ◦ ◦ ◦ ◦ ◦ ◦ ◦ ◦ Gender Socioeconomic class Education Immigrant status Acculturation Religion Personal psychology Life experience Elicit patient perspectives on illness and their expectations Ask patient if they have a certain belief Open-ended questions Empathic comments Increase awareness of racial and ethnic disparities in health and the importance of socio-cultural factors on health beliefs and behaviors Identify the impact of race, ethnicity, culture and class on clinical decision-making Develop tools to assess the community members’ health beliefs and behaviors Develop human resource skills for crosscultural assessment, communication and negotiation Excellent evidence - improves knowledge of health care professionals Good evidence – improves attitudes and skills of health professionals Good evidence –impacts pt satisfaction Poor evidence training impacts pt adherence Poor evidence - training cost No studies - health outcomes What do you think caused your sickness? Why do you think it started when it did? What do you think your sickness does to you? How severe is your sickness? What are the biggest problems your sickness has caused for you? What do you fear most about your sickness? What are the most important results you hope to get from treatment? Kleinman What do you think might be going on? Would you like me to tell you the full details of your condition? Is there someone else you would like me to talk to? What language are you most comfortable speaking? What are your greatest concerns now that you have this illness? Who can help you with physical care, emotional support, transportation? Where do you go for religious or spiritual strength, or solace? What kind of assistance is available to you in your community that might be helpful during this time? Where were you born and raised? When did you emigrate to the U.S.? Understanding patients as individuals in context of culture does not prevent conflicts over differing beliefs, values, or practices Does serve to identify areas of negotiation and create atmosphere of mutual respect Ventilation and cardiopulmonary resuscitation hasten death Nodding indicates politeness and respect not agreement May seek aggressive treatment bc value sanctity of life not bc misunderstand limits of technology History of poor access to care may feel palliative care = giving up or poor care American Islamics expect broader issues of faith and belief to be addressed in clinical encounter Black women who think God is controlling health less likely to get mammograms Some black communities believe suffering is redemptive, must be endured, stopping life support to avoid pain and suffering may be seen as failing a test of faith Family is decision maker - responsibility to protect the sick from burden Hospice is failure of the caretaker Filial piety – expectation children will care for their parents How well fulfill their filial duties is open to community scrutiny and judgment Reflect poorly on parenting abilities “Face” – indirect communication ◦ never put pt in a position of embarrassment or loss of honor by directly asking a sensitive questions ◦ preservation or family and community honor (Chinese American) Allows ambiguity and allows to save face and possibility of hope Can offer patient opportunity to know “informed refusal” Statements of family are indirect questions – acknowledges families fears, respects need for indirect discussion, invites further questions Feel western MD seems to be giving negative info through informed consent, truth telling, advance care planning Home or natural remedies Religion is a source of enormous emotional support More likely to want aggressive care at end of life Less likely to have DNR and advance care plans Less likely to trust the motives of md Mistrust is a barrier to organ donation Mistrust is barrier to participating in medical research More blacks fear inadequate medical care Feel many unmet needs for communication Want to be informed of dx and prognosis to make informed decisions Anderson LM, Scrimshaw SC, Fullilove MT, Fielding JE, Normand J, the Task Force on Community Preventative Services. Culturally competent healthcare systems. A systematic review. Am J Prev Med 2003;24(3S):368-379. Back A, Arnold R, Tulsky J. Mastering Communication with Seriously Ill Patients. Balancing Honesty with Empathy and Hope 2009. Cambridge University Press. Beach MC, Price EG, Gary TL, et al. Cultural competency: A systematic review of health care provider educational interventions. Med Care. 2005 April;43(4):356-373. Betancourt JR, Green AR, Carrillo. Cultural Competence in Health Care: Emerging Frameworks and Practical Approaches. The Commonwealth Fund, Field Report 2002. Betancourt JR, Green AR, Carrillo JE, Ananeh-Firempong O. Define cultural competence: A practical framework for addressing racial/ethnic disparities in health and health care. Public Health Reports JulyAugust 2003;118:293-302. Betancourt JR, Green AR, Carrillo E, Park ER. Cultural competence and health care disparities: Key perspectives and trends. Health Aff March 2005;24:499-505. Carrese JA, Rhodes LA. Bridging cultural differences in medical practice. The case of discussing negative information with Navajo patients. J Gen Intern Med 2000;15:92-96. Crawley LM, Marshall PA, Lo B, Koenig BA. Strategies for culturally effective end-of-life care. Ann Intern Med 2002;136:673-679. Kagawa-Singer M, Blackhall LJ. Negotiating cross-cultural issues at the end of life. “You got to go where he lives”. JAMA 2001;286(23):2993-3001. Kleinman A. Patients and Healers in the Context of Culture. Berkeley, California: University of California Press, 1980. Levin SJ, Like RC, Gottlieb JE. ETHNIC: A Framework for culturally competent clinical practice. In: Appendix: Useful Clinical Interviewing Mnemonics. Patient Care 2000;34(9)188-9. Mull JD. Cross-cultural communication in the physician’s office. West J Med 1993;159:609-613. Steiner RP, Rubel AJ. Recommended core curriculum guidelines on culturally sensitive and competent health care. Fam Med 1996;27:291-297. R Resources for patients and families I Individual identity and acculturation S Skills of patient and family to adapt to disease K Knowledge ab health beliefs, values, practices, and cultural communication etiquette Resources for patients and families Tangible resources that the family can draw on, such as: level of education, socioeconomic status (including insurance), social support networks, in-language social service agencies, transportation, grocery shopping, etc. What kind of assistance is available to you in your community that might be helpful during this time?’’ ‘‘Do you know others in your community who have faced similar difficulties?’’ Individual identity and acculturation/ assimilation Questions about the patient, the context of his or her life, and individual circumstances, including place of birth, refugee or immigration status, languages spoken, and degree of integration within the ethnic community. ‘‘Where were you born and raised?’’ ‘‘When did you emigrate to the U.S. and how has your experience been coming to a new country?’’ ‘‘What languages do you speak and in which are you most comfortable talking?’’ What are your most important concerns now that you have this illness? Life history assessment: ‘‘What were other important times in your life and how might these experiences help us to know you?’’ Skills available to the patient and family to adapt to the disease requirements The actual ability of the patient and the family to navigate the health care system and cope with the demands of the disease itself—emotionally, physically, socially, and spiritually. ‘‘Who are the people in your support system that are helpful or harmful?’’ ‘‘Who is there to help you with physical care, emotional support, transportation, and care of loved ones.’’ ‘‘Who do you see or talk with, where do you go for religious or spiritual strength, or solace? Knowledge about the ethnic group’s health beliefs, values, practices, and Cultural communication etiquette Beliefs, values and practices associated with communication etiquette and health, including attitudes toward truth-telling, family-centered vs. individual-centered decision-making style, historical, social, and political issues that might affect relationships between the patient and elements of the dominant culture. Knows the dominant ethnic groups in practice. Reads about the different cultures. Attends continuing education programs about each culture—the beliefs, values, and practices surrounding health, including truth-telling. What is the symbolic meaning of the disease? Learns about surrounding death and dying; Does the patient/family adhere these beliefs and practices? How are decisions made in this cultural group? Does this family adhere to traditional cultural guidelines or do they adhere more to the Western model? A B C D E Attitudes Beliefs Context Decision making Environment E T H N I C S Explanation Treatment Healers Negotiate (mutually acceptable options) Intervention (mutually acceptable) Collaboration (patient, family, healers) Spirituality B E L I E F Beliefs What caused your illness/problem? Explanation Why did it happen at this time? Learn Help me to understand your belief. Impact How is this impacting your life? Empathy This must be very difficult for you. Feelings How are you feeling about it? L E A R N Listen to the patient's perspective Explain and share MD’s perspective Acknowledge differences Recommend a treatment plan Negotiate a mutually agreed upon plan Assessment – willing to participate in discussion Preparation - disclose potentially upsetting information Communication - caring, kind, respectful manner, do not rush, positive focus Follow-through