Chapter 1 The Injury Evaluation Process
advertisement
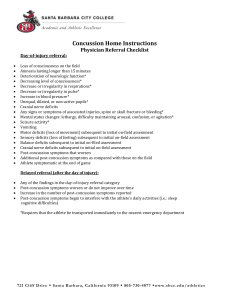
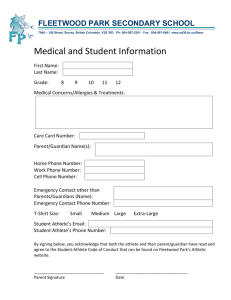
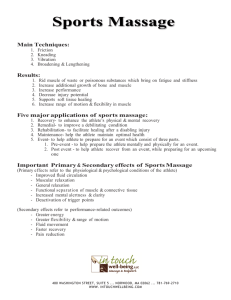
Chapter 1 The Injury Evaluation Process Introduction Accurate initial assessment is essential for successful management and rehabilitation of an injury Evaluation process is ongoing throughout all phases of recovery A systemic and methodical evaluation model leads to efficiency and consistency in the evaluation process Systemic Evaluation Technique Figure 1-1, page 2 The Role of the Noninjured Paired Structure – Table 1-1, page 3 Clinical Evaluations History Most Important portion of examination Communication is key Cultural Considerations, page 4, Box 1-1 Information that should be obtained: • • • • • Mechanism of injury Relevant sounds/sensations at time of injury Location of symptoms Onset and duration of symptoms (Table 1-2, Pg 5) Description of symptoms Information that should be obtained cont.: • • • • Changes to symptoms Previous history Related history to the opposite body part General medical health NCAA Guideline 1B – page 6, Box 1-2 Inspection Gross deformity Swelling (Girth measurement pg 9, volumetric measurement pg 10) Bilateral symmetry Skin (figure 1-4, page 10) Infection Palpation Point tenderness Trigger points Change in tissue density Crepitus Symmetry Increased tissue temperature Range of Motion Bilateral comparison, normative data Goniometric evaluation – pg 11, Box 1-4 Planes of the body Active range of motion (AROM) Passive range of motion (PROM) Resisted range of motion (RROM) • Break tests • Manual muscle testing • End -feels Ligamentous and Capsular Tests Grading System – pg 15, Table 1-7 Laxity vs. instability Special Tests Neurologic Tests Sensory Testing Motor Testing Reflex Testing Activity-Specific Functional Testing On-Field Evaluation of Athletic Injuries Ambulatory vs. athlete-down On-field evaluation must rule out: Inhibition of the cardiovascular and respiratory systems Life-threatening trauma to the head or spinal column Profuse bleeding Fractures Joint dislocation Peripheral nerve injury Other soft tissue trauma Disposition of condition Communication plan/emergency action plan Sport specific rules On-Field Relatively brief On-Field Inspection Is athlete moving? Position of athlete Primary/secondary survey On-Field History Palpation Findings may warrant transporting athlete to hospital On-Field Range of Motion Testing AROM first Weight-bearing status On-Field Ligamentous Testing On-Field Neurologic Testing Removal of Athlete From the Field Termination of the Evaluation Table 1-9, page 25 Standard Precautions Against Bloodborne Pathogens Table 1-10, page 26 The Roles of Different Health Care Professionals Athletic Trainer Physical Therapist School Nurse Emergency Medical Technician Physician Documentation