Document
advertisement

FUNCTIONAL ORGANISATION
OF CARDIOVASCULAR SYSTEM
BL Mtinangi. MD MSc PhD
Department of Physiology
HURBERT KAIRUKI MEMORIAL
UNIVERSITY
January 7th , 2016
1
2
THE CIRCULATORY SYSTEM
3
CONDUCTION IN THE HEART
4
CONDUCTION IN THE HEART
5
THE CIRCULATORY SYSTME
6
CIRCULATION IN THE HEART
7
•A circulatory system was discovered in
1628 by Sir William Harvey.
8
Who Was William Harvey?
• Born 1578 (England)
• Physician to King Charles I
of England
• Died 1657
• Discovered: Circulation of
blood
9
Before Sir William Harvey
• People believed in Galen’s theory
that blood was produced in the
liver. Galen believed that blood
was burnt up by the body. Other
writers had questioned this theory
but they had struggled to prove it
wrong.
10
Sir William Harvey
• Harvey proved that blood flows
around the body. He stated that blood
was carried away from the heart by
arteries and returns to the heart
through veins.
• Harvey proved that the heart is a
pump that recirculates the blood and
that blood wasn’t ‘burnt up
11
12
Harvey’s Methods
• Harvey was very scientific in his methods. These
included:
• Dissecting cold blooded animals (e.g. reptiles) to
observe the movement of muscle around the
heart.
• Dissected humans to gain a knowledge of the
heart.
• Used iron rods to prove that blood was pumped
through veins in one direction.
• He accurately calculated the amount of blood in
the body.
13
Nice One, Harvey.
• Harvey made predictions based on
his meticulous methods that were not
confirmed until after his death.
• An example of this was his prediction
of the existence of capillaries. Harvey
couldn’t see , but said they must
exist. With the invention of
microscopes he was proven right.
14
Opposition to Harvey’s ideas
• Just like Vesalius and Pare before
him, Harvey had to overcome
opposition from people who could not
believe Galen could be wrong.
• Harvey’s theories were slowly proven
right and Harvey died a wealthy
respected doctor with many important
patients.
15
What Does C-V System do?
• Circulate blood throughout entire
body for
– Transport of oxygen to cells
– Transport of CO2 away from cells
– Transport of nutrients (glucose) to cells
– Movement of immune system
components (cells, antibodies)
– Transport of endocrine gland secretions
16
• Two main system of blood
circulation:
1. Systemic blood circulation
2. Pulmonary blood circulation
17
18
SYSTEMIC CIRCULATION: Blood flow from the
Left Ventricles to the Right Atrium &
comprises:
• The heart with 360mls (7%) blood
• The arteries with 700mls (14%) blood
• Capillaries with 300m/s (6%)blood
• Veins with 3200mls {64%} blood
Systematic circulation is achieved by the
driving force of blood from LEFT
Ventricle (LV)
• Pulmonary circulation is achieved by
the contraction of Right Ventricle (RV).
19
20
The force or magnitude for systemic
circulation is 93.3mmHg, this is a
mean systemic pressure
• Mean systemic/arterial pressure is equal to
DBP+1/3 (SBP – DBP)
if Diastolic blood pressure (DBP) =80
Systolic blood pressure (SBP) =120
MAP = 80+1/3 (120-80)
= 80+40/3 (13.3)
= 80 +13.3
= 93.3 mmHg
21
Pressures in the systemic
circulation
LV - 120mmHg during heart
systole
- 0 mmHg during diastole
Aorta - 120mmHg during systole
- 80 mmHg during diastole
RA - 0mmHg during diastole
22
PULMONARY CIRCULATION
• Circulation from Right Ventrical
(RV) through the Pulmonary
Artery (PA) to the LUNGS then
into the Left Atrium (LA).
• The RV Contraction generates
the driving force of the blood.
23
Pulmonary blood vessels have about 440m/s
(9%)blood
Pressure in the pulmonary circulation
• RV = 22mmHg during systole
= 0mmHg during diastole
PA = 22mmhg during systole
= 8mmHg during diastole
Mean pulmonary pressure
= DBP+1/3 (SBP- DBP)
= 8+1/3 (22-8)
=8+14/3 (4.67)
=12.67 mmHg
24
Happy
New
Year
2016
25
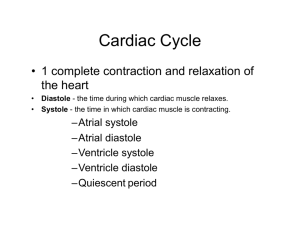
THE CARDIAC
CYCLE
26
THE CARDIAC CYCLE
Cardiac cycle is the period of the end of one cardiac contraction to
the next contraction ie involving SYSTOLE and DIASTOLE
One cardiac cycle is reflected by electrical and mechanical change.
1.Elecrical changes – recorded by ELECTROCARDIOGRAM (ECG)
2.mechanical changes are reflected by changes in
- PRESSURE
- VOLUME
- HEART SOUNDS
- MYOCARDIAL BLOOD FLOW
• One cardiac cycle consist of;
1.Ventricular systole or systolic phase (ie a period of contraction)
and
2.Ventricular diastole or diastolic phase (ie period of relaxation)
27
THE EVENTS IN THE CARDIAC
CYCLE
28
29
Electrical changes recorded
by ECG
- The electrocardiogram is a graphic recording
showing voltage or current variation in relation to
time.
- Current are generated by cardiac electrical activity
- The ECG is a clinical tool which has remain an
important art in cardiac electrical physiology
- ECG are clinically useful because certain ECG
waves a pattern frequent association with certain
specific types of heart disease.
- Hence ECG is part of the clinical evaluation of any
patient suspected of having heart disease.
30
31
ELECTROCARDIOGRAM
(ECG)
32
ECG RECORDS
• It records the electrical
currents generated by the
heart and recorded from the
surface of the body
• Waves recorded are P,QRS
complex and T waves
33
ECG RECORDS
34
The interpretation of an ECG waves
• A lead is a combination of two or more ELECRODES attached
to the recording galvanometer
• A starndard twelve {12} leads are used in routine CLINICAL
ELECTROCARDIAGRAPHY (ECG)
Three Bipolar or standard leads- leads I,II, III, these record the
potential difference between : Rt arm and Lt arm = I
Rt arm and Lt leg = II
Lt arm and Lt leg = III
Three unipolar limb leads these are exploring electrodes placed
at.
Rt arm = avR
-
Lt arm = avL
-
Lt foot = avF
-
35
CONVECTIONAL DIRECTION OF THE SIX LIMB
LEADS.
-150
Lead
avL
Lead avR
-30
Lead I
+-180
Lead III
0
Lead II
+60
+120
Lead avF
+90
36
PRECORDIAL LEADS
THESE ARE
• V1 4th Intercostal Space (ICS) to the Rt side of
sternum
• V2 4th ICS to the Lt side of sternum
• V3 positioned diagonally between V2 and V4
• V4 5th ICS mid clavicular line
• V5 anterior auxiliary line at the same level as V4
• V6 mid auxiliary line at the same level as V4
37
ECG INTERPRETATION
• P wave a normal P wave is a result of atria activation
due to a spread of depolarization from Sino Atrial
Node (SAN) through the atria leading to ATRIA
CONRACTION.
• PR interval, is the interval from the beginning of the P
wave to the beginning of the Q wave
• QRS complex – represents depolarization of the
ventricles leading to ventricular contraction
• QT is the interval from the beginning of the Q wave to
the end of the T wave (represent depolarization &
repolarazation period)
• ST segment is the segment from the end of the S
wave to the beginning of the Twave
• T wave –due to VENTRICULAR repolanzation ie
ventricular relaxation
38
ELECTROCARDIOGRAM
(NORMAL ECG)
39
Some useful information from
ECG
The ECG help us to interpret whether the
Heart: Rate is normal, Bradycardia/
tachycardia?
Rhythm -regular or irregular
-bundle branch block
Axis – normal or right or left axis deviation
Hypertrophy – LVH or RVH or both
Infarction/myocardial/injury through
changes in: - Q waves
- invented T waves
- elevated ST segment
40
MECHANICAL FUNCTION OF THE
ATRIA
THERE ARE TWO PHASES OF FUNCTION.
• PASSIVE PHASE: where 75% of blood flows
directly and continuously from the great veins
through the ATRIAL into the VENTRICLES.
even before the atria contract.
• ACTIVE PHASE: This is due to ATRIA
contraction which causes an additional 25%
filling of the ventricles.
• NB. The heart can continue effectively without
this additional 25% unless a person exercises.
41
PRESSURE CHANGES IN THE ATRIA
• The 3 major pressure elevation are:
a, c and v atrial pressure waves.
The a wave is caused by atrial contraction.
Ordinarily Rt atrial pressure increases to 4
to 6 mmHg during atrial contraction
Lt atrial pressure increases to about 7 to 8
mmHg.
42
ATRIAL PRESSURE CHANGES
CONT.
• The c waves occurs when the ventricles
begin to contract mainly by bulging of the
A-V valves.
• The v waves occurs towards the end of
the ventricular contraction as a result of
some blood flow from the veins while the
A-V valves are closed.
43
MECHANICAL FUNCTION OF THE
VENTRICLES
1. VENTRICULAR FILLING
1.1 passive phase – 70% of blood passes directly to the
ventricles
1.2 active phase 20-30% of blood enters the ventricles
due to atria contraction
Three stages of ventricular filling
2.1 rapid filling – first 1/3 rd
2.2 Diastalsis phase – middle 1/3 rd
2.3 Additional filling – last 1/3rd due to atria
contraction
44
3. EMPTYING OF VENTRICLES
(ventricular systole)
The A –V valves closes and the semi lunar valves
opens causing;
3.1 Rapid ejection of blood 70% of blood in ejected
rapidly
3.2 slow ejection of blood 30% of blood in ejected
slowly
-time for ventricular filling (diastole) = 0.5 sec
-time for ventricular emptying (systole) = 0.3 sec
-total time for diastole and systole one cycle = 0.8 sec
Cardiac circles in one minute (60 sec)
60/0.8 = 75 cycles or heart beat/min
45
ISOVOLUMERTIC CONTRACTION
4.THE ISOVOLUMERTIC CONTRACTION
• Contraction or systole is occuving but NO EMPTYING ie a
period between Mitral and opening of Aortic and pulmonary
valves ie
ONLY TENSION in increasing but shortening of muscles
5.THE ISOVOLUMETRIC RELAXATION
• Relaxation or diastole is occurring but no FILLING of the
ventricles
i.e. a period between aortic and pulmonary valves closure and
opening of A – V, valves ONLY TESNSION is decreasing but
no lengthening of muscles
46
VENTRICULAR VOLUME CHANGES
• Volume at the end of diastole (end
diastolic volume ie EDV) 120 – 130
mls
• Volume at the end of systole (end
systole volume ie ESV) 50 – 60 mls
EDV – ESV = SV
e.g. 120 – 50 = 70 mls
or 130 – 60 = 70mls
47
STROKE VOLUME (SV)
• Stroke volume (SV) is the amount of blood
ejected from the ventricle during a single heart
beat
• Cardinal output (CO) is the amount of blood
pumped out of the heart per minute.
CO = SV X HR
= 70X75 = 5250 mls/min ie about 5L/min
Stroke volume depends on
-preload
-after load and contractility.
48
DETERMINANTS OF SV CONT.
•
Pre load is the volume in the ventricle at the
end of diastole – Ventricular End Diastolic
Volume (VEDV)
An increase in VEDV increases SV ( obeys frank
starling law of the heart)
An increase VEDV increases myocardial
stretching this increases myocardial contractile
power.
• Afterload is an expression of the resistance
which the ventricles must overcome in order to
eject the stroke volume.
49
FACTORS THAT AFFECT
AFTERLOAD
The factors that affect the AFTERLOAD are:
• The resistance in the Aorta
• The peripheral resistance
• The viscosity of the blood
Increases of the above factors WILL
INCREASE the AFTERLOAD.
50
DETERMINANTS OF SV CONT
• CONTRACTILILY is the force of the
ventricular contraction and it is
independent of ventricular loading but
depends on the interaction of myosin and
actins found in the thick and thin filaments
51
THANK YOU
52