1 Unit (250cc)
advertisement
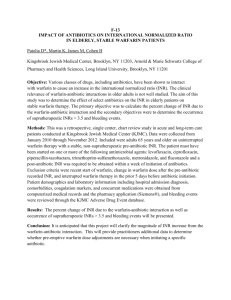
I have no financial disclosures or commercial endorsements to disclose Four ED cases encountered over the past year › Differential Diagnosis › Epidemiology › Pathophysiology › Emergency Management Not a “traditional” toxicology lecture Emergency care relevant to IM & pediatric office practices 59 yo F with a “nosebleed that won’t stop”. Pressure & anterior nasal packing fail despite clear bleeding site at Kisselbock’s After 3 hrs at home & 2 hrs of ED failed bleeding control she is tachycardic, hypotensive then has a syncopal event Vitals: HR 130s & irregular, BP 74/42, Sat 92% ra Differential diagnosis? In 1900s bis-hydroxycoumarin discovered after cows eat spoiled sweet clover & die of massive hemorrhage Warfarin derivatives used therapeutically as anticoagulants, commercially as rodenticides ~3000 accidental exposures annually › 79% in <6yo children In adults complications usually from incorrect dosing or diet / medication misadventures 1%-8% toxicity risk for each year of therapy › Bleeding risk elevates as INR increases; 50% bleeding episodes occur w/ INR <4.0 Inhibits synthesis of vitamin Kdependent coag factors II, VII, IX, X › No effect on established thrombus › Prevent progression / secondary thromboembolic complications Metabolized by hepatic CP-450 isoenzymes to inactive metabolites Abn metabolism alters physiology › Advanced age, hepatic dysfunction, diet, numerous meds ½ life 20-60 hrs, effect duration 2–5 days, peak concentration 4 hrs Reversal & stabilization › › › › Stable vs unstable? Acute vs chronic? Why anticoagulated? Why reversal? Exam: includes skin, neurological, rectal Rads: If AMS or trauma obtain CT / US of affected area Labs: › Type / cross, CBC, coags, LFTs, +/- tox screen › PT / INR (anticoagulant effect) › Vitamin K dependent factors If critical need for anticoagulation (i.e. mechanical heart valve), heparin temporizes while warfarin reversed INR BLEEDING PRESENT RECOMMENDATION >Therapeutic - <5 No Lower warfarin dose, or omit dose & resume at low dose; no reduction if minimally elevated >5-9 No Omit 1-2 doses, serial PT/INR, resume warfarin at lower dose; or omit dose & give 12.5mg vitamin K po >9 No Hold warfarin, give 2.5-5 mg vitamin K po, serial PT/INR, administer more po vitamin K prn; If prosthetic heart valves, FFP > vitamin K Any Serious or Life-threatening Hold warfarin. Vitamin K 10mg IV. FFP. Consider PCC, rfVIIa Ansell J. Pharmacology and management of the vitamin K antagonists: Chest 2008 Fat soluble vitamin required for protein modification, blood coagulation, & metabolic pathways Plant source (soy & green vegetables) Overcomes competitive blocks Clinical effect delayed for hours while liver synthesizes clotting factors & plasma factors II, VII, IX, X restored IM, IV & PO equivalent, SQ not recommended FFP contains plasma + coag factors › Free of RBCs, WBCs, PLTs › ABO compatible w/o rH considerations In a 70 kg Patient: › 1 Unit (250cc) FFP increases factors 2.5% › 4 Units (1000cc) FFP increase factors 10% › 10% increase of factor levels required for clinically significant change in coag status, so usual dose is 4 units Prothromin Complex Concentrate (PCC) › › › › › › No thawing Factors II, IX & X, minimal factor VII; new products include factor VII Some contain protein C & S, antithrombin II or heparin 4-factor products reverse coagulopathy within 30 mins Must add FFP for F VII if 3-factor products (Prothrombinex-HT®) Vitamin K1 to sustain reversal Recombinant Factor VIIa (rFVIIa / Novo7®) › No thawing › Less volume, ARDS, transfusion reactions & infection transmission › Vitamin K1 to sustaining reversal Despite apparent advantages, no proven mortality benefit for rFVIIa or PCC > FFP Initial INR 6 / hemoglobin 7 required 2.5mg po vitamin K, 4 units FFP, 1 unit PRBC Hemorrhage controlled with bilateral RhinoRockets® Admitted for 23 hr obs, warfarin held x 2 dosages Determined pt accidentally doubling warfarin dosage due to pharmacy error 21 mo F presents because “she wouldn’t wake up from her nap”. Parents earlier noted child playing with grandma’s pill bottles; Grandma counted pills & thinks “1 or 2” missing Child floppy, minimally responsive, dilated pupils ABCs – airway patent, hypoventilation, thready pulse › IO, O2, monitor › HR 68, BP 92 palp, Sat 85% ra, T 96 pr Differential Diagnosis? 6,000,000 potentially toxic ingestions yearly › Most common age group: 1-5 yo Predominately accidental (toddlers), intentional (teens) MCC fatal poisonings: › › › › › Iron TCAs Cardiovascular medications Hypoglycemics Hydrocarbons MEDICATION / DRUG POTENTIALLY LETHAL DOSE (10KG) Codeine 3 60mg tablets Desipramine 2 75mg tablets Hydrocarbons 1 teaspoon (if aspirated) Imipramine 1 250mg tablet Iron 2 adult strength tablets Lindane 2 teaspoons Theophylline 1 500mg tablet Verapamil 1 240mg tablet Metoprolol 2 50mg tablets Sulfonylureas 2 5mg tablets AMS differential diagnosis In non-diabetics, hypoglycemia usually asymptomatic until glucose <40 mg/dL › › › › › › › › › Weakness Diaphoresis Tachycardia Tachypnea Transient neurologic deficit Pallor / Cyanosis Seizure / Tremor / Jitteriness Coma Hypothermia Miscellaneous › Sepsis › Malnutrition › Renal / Liver Failure Hyperinsulinemia › Beckwith-Weidman › β Cell Hyperplasia (Nesidioblastosis) Toxicity: › ETOH, Salicylates, Methadone, Hypoglycemics HPA Axis Abnormality Inborn Errors of Metabolism: Carnitine Deficiency Fructosemia Galactosemia Glycogen-Storage Disease Type I › Maple Syrup Urine Disease › › › › 1st generation sulfonylureas (i.e. tolbutamide), very potent, ½ life 3549 hrs 2nd generation sulfonylureas (glipizide, glyburide, glimepiride) less potent, shorter ½ lives Non-sulfonylureas: biguanides, aglucosidase inhibitors › High dosages do not significantly decrease serum glucose › “Anti-hyperglycemics” not “hypoglycemics” Sulfonamide derivatives w/o antibacterial activity Bind to K+ receptors sensitive to β cell membrane ATP resulting in Ca++ influx, K+ efflux, membrane depolarization & insulin release Decrease serum glucagon, potentiate insulin action in extrapancreatic tissues Effective if functional β cells ABC, IV, O2, Monitor IV / IO dextrose / glucose PO / IV glucagon › NPO if AMS IV octreotide or diazoxide Other than for glipizide (enterohepatic circulation) activated charcoal not beneficial >1 hr post ingestion No role for hemodialysis Dextrose (D-glucose) › Rapid serum glucose elevation › Monosaccharide absorbed from GIT then distributed to tissues Glucagon › Polypeptide hormone from beef or pork pancreas Islets of Langerhans alpha cells › ½ life 3-6 min › Gluconeogenesis & lipolysis by inhibiting glycogen synthesis & enhancing glucose formation from proteins & fat stores › Glycogenolysis by increasing liver hydrolysis of glycogen to glucose Diazoxide (Hyperstat) › Increases glucose by inhibiting pancreatic insulin release › Hyperglycemic effect within 1 hr, lasts 8 hrs Octreotide (Sandostatin) › Acts on somatostatin receptors › Hyperpolarization of β cells inhibits Ca++ influx & insulin release If 1st gen sulfonylurea admit for minimum 24 hrs regardless of symptomatology If 2nd gen sulfonylurea may discharge home if asymptomatic & euglycemic for 8-12 hrs If AMS, lethargic or seizure, admit to PICU Parental education! Patient known to EMS & ED for multiple visits for hypoglycemia Presents via ambulance with AMS. FSBG 120 “but we already gave an amp of D50 because that what he always needs” Patient remained altered during transport, did not respond as usual. Upon arrival, lethargic, maintaining gag, FSBG 135 IV, O2, monitor placed & following noted: • Vitals: HR 28, BP 64/34, T 98, Sat 82% NRB • Differential Diagnosis? Dependent on history + vitals Bradycardia pathway if cannot obtain history Beta Blockers › Lipophillic, large VOD › Wide variations in pharmakokinetics, but generally absorbed in GIT, eliminated hepatically or renally (atenolol, nadolol, esmolol) › Inhibit β adrenergic stimuli with (-) inotropy & chronotropy Calcium Channel Blockers › Highly protein bound, large VOD › 1st pass effect via hepatic metabolism (low bioavailability) › Decreased calcium influx, causing (-) inotropy, chronotropy, dromotropy & vasodilation (decreased PVR) Narrow therapeutic to toxic ratio Most common features: hypotension + bradycardia EKG: sinus bradycardia with PR prolongation › BBs > CCBs cause QRS prolongation BBs cause additional symptoms due to effects on systemic beta receptors: › › › › Bronchospasm Hypoglycemia Hyperkalemia CNS toxicity Regulatory hormone with (+) inotropic & chronotropic effects on myocardium via increasing cAMP Effects independent of betaadrenergic stimulation Reverses hypotension, bradycardia & myocardial depression Does not significantly reverse conduction disturbances (i.e. QRS prolongation) Epinephrine › β adrenergic to treat hypotension+ bradycardia Calcium Gluconate or Chloride › 30 mL gluconate =1 gm of calcium › Rapid contractility improvement, limited effect on nodal depression or PVR › If critical hyperkalemia, chloride > gluconate NaHCO3 › Treatment of QRS prolongation Dopamine › a & β adrenergic actions Magnesium › Hypocalcemia refractory to treatment if hypomagnesemia ABC, IV, O2, Monitor Central line › › › › Glucagon CaCl MgSO4 Epinephrine gtt RSI: vecuronium & etomidate Ventilation with low PEEP Atropine Med Flight to MGH External pacing D/C at day 7…to be seen at Tobey 10 days later with ~ hypoglycemia! 42 yo WF presents via police with SI. Arguing with husband, stated SI including driving off a cliff. Calm & forthcoming during interview, denying current SI Tox screen: negative Crisis arrived 3 hrs after interview to find pt unresponsive, “twitchy” with “odd jerking motions”. Tech noted pt restless x 30-45 mins MD called to room to find patient seizing Airway controlled, ativan given, placed on monitor › HR 120, BP 90/60, Sat 90%ra, T not done Differential Diagnosis? IV, O2, Monitor 2 large bore IVs, 2 L NS bolus 2 amps NaHCO3. then NaHCO3 drip 2 grams MgSO4 Partially awake intubation, followed by vecuronium Ventilation w/ low PEEP Dopamine CNS Catastrophe Heatstroke Metabolic: › › › › › › › › › › Hyperkalemia › Hypocalcemia › Hyponatremia Status Epilepticus Arrythmias: › Sinus Brady › Heat Block › WPW › VF / VF / Torsades OD: Anticholinergic Antidepressant Antihistamine Digitalis INH Local Anesthetic Salicylate TCA Antiarrythmic Withdrawal Syndromes Metabolic Acidosis en 1 isch 674 1024 Extensively protein bound, large VOD Hepatic metabolism, excreted as active metabolites with long ½ life Toxic effects mediated through: › Anticholinergic › a 1 blockade › Class 1a quinidine-like effects › Postganglionic norepinephrine reuptake blockade Narrow therapeutic index Rapid onset of CNS & CV effects Unlikely to develop life-threatening events 6 hrs post ingestion May appear to have a pure anticholinergic toxidrome Sinus tach 1st sign of toxicity Class 1A antiarrhythmic effect decreases Na+ influx through fast Na+ channels Decreased phase 0 slope prolongs QRS / QT / PR Delays myocardial & conducting tissue depolarization QRS >0.16 with predicts seizures / arrhythmias > drug levels › >130 msec, 90% required mechanical ventilation › >120 msec, 1/3 seized › >160 msec, 75% VT / VF aVR terminal R >3mm better predictor of seizures or arrhythmias than QRS duration Right axis shift in last 40ms of QRS, deep S wave in lead 1, large R wave in aVr suggestive of TCA cardiotoxitiy TCA anti–a adrenergic effects Negative inotropy Peripheral vasodilatation (decreased PVR) Inhibition of Na+ flux into myocardium depresses inotropy CARDIOVASCULAR CNS ANTICHOLINGERGIC Sinus Tachycardia Drowsiness Dry Mouth Prolonged PR/ QRS/ QT Opthalmoplegia Blurred Vision ST Wave Abnormalities Seizures* Dilated Pupils Heart Blocks Pyramidal SSX Urinary Retention Vasodilation Rigidity Absent Bowel Sounds Hypotension Delirium Pyrexia Cardiogenic Shock Respiratory Depression Myoclonic Twitching VT / VF Coma Asystole *Serotonin or norepinephrine mediated effects ABC, IV x 2, O2, Monitor, EKG Correcting hypotension, hypoxia, acidosis reduces cardiotoxicity & arrhythmias Unlike pure anticholinergic toxicity, no physostigmine (decreases seizure threshold, arrythmogenic) ICU admission Many common meds have “TCA-Like” toxicity QRS >100 ms, seizures, acidosis, hypotension, ventricular arrhythmias, cardiac arrest Corrects acidosis by increasing extracellular Na+ › Narrows QRS › Stabilizes Na+ channels › Raises BP even if no acidosis › Increases TCA plasma protein binding › Improves inotropy Patient decompensated en route to Boston At MGH, placed on epinephrine gtt, Swan-Ganz placed, intralipids started Hemodialysis initiated when creatinine bumped to 5 & potassium elevated After 4 days in the ICU, extubated › OD cocktail: amitriptyline, flexeril, diphenhydramine Discharged to psychiatric rehab on day 7 of hospital stay www.emedicine.com~“INRReversal”, “Sulfonylurea Toxicity”, “TCA Overdose” 2011. Leissinger CA, Blatt PM, Hoots WK, et al. Role of prothrombin complex concentrates in reversing warfarin anticoagulation: A review of the literature. Am J Hematol. 2008;83:137-43 Weber JE, Jaggi FM, Pollack, CV. Anticoagulants, antiplatelet agents, and fibrinolytics. In: Tintinalli JE, Kelen GD, Stapczynski JS, eds. Emergengy Medicine: A Comprehensive Study Guide. 6th ed. McGraw-Hill; 2004: 1354-60 Hirsh J, Guyatt G, Albers GW, et al. Executive Summary: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 2008;133:72S-3S Poison Control Center Data. 2010 AHA Cardiovascular Care Recommendations; Warfarin reversal: consensus guidelines, on behalf of the Australasian Society of Thrombosis & Haemostasis. Circulation. 2010. Baker R. Wood; the Warfarin Reversal Consensus Group recommendations. MJA 2004; 181 (9): 492-497 Bonow RO, Carabello BA, Chatterjee K, et al. 2008 Focused update incorporated into the ACC/AHA 2006 guidelines for the management of patients with valvular heart disease”. Circulation 2008; 118(15):e523-661. Tintanelli. “Emergency Medicine”. 2009. www.cdc.gov~Poisoning statistics 2010. www.aapcc.org~American Association of Poison Control Website. 2011. www.toxicology.org~Toxicologyand Critical Care Management Updates. 2011 Carr D. Successful resuscitation of a doxepin overdose using intravenous fat emulsion (IFE). Clinical Toxicology 2009; 47(7): 710. Review of the epidemiology, pathophysiology, differential diagnosis & emergency management of four common overdoses Implications for internal medicine & pediatrics Importance of a broad differential diagnosis & early recognition and aggressive emergency management Questions? Thank you for your time ~ find me nights at Tobey ED or at Amy.Gutman72@gmail.com