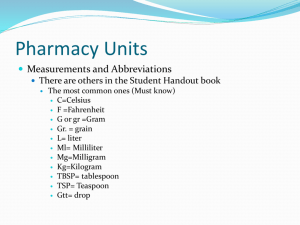
Renal Emergencies: Fluids and Electrolytes
advertisement

Caroline Straatmann, MD ¼ Plasma (Intravascular) 1/3 ECF ¾ Interstitial Fluid 0.6 x weight 2/3 ICF Intracellular (mEq/L) Extracellular (mEq/L) Na 20 135-145 K 150 3-5 ____ Cl 98-110 HCO₃ 10 20-25 PO₄ 110-115 5 Protein 75 10 A 12 year old boy with chronic renal insufficiency secondary to obstructive uropathy is admitted for pancreatitis. He cannot tolerate enteral feeds and is on TPN. He complains of his legs feeling weak. Labs show 144 7.4 120 15 60 4.7 What do you do first? EKG EKG shows peaked T waves What do you do next? Give calcium gluconate Stop his TPN, which has K in it! In addition to this treatment, which one of the following would be the most effective therapy for his hyperkalemia? Subcutaneous insulin and slow infusion of glucose Intravenous beta – 2 agonist Intravenous insulin Intravenous sodium bicarbonate Oral sodium polystyrene sulfonate Growing child requires 1-2 mEq/kg/day Avoid potassium deficiency Cellular growth Serum potassium concentration does not reflect total body potassium content Ex: Diabetic ketoacidosis Disturbance in serum K⁺ can affect cell membrane resting potential Muscle paralysis Ventricular arrhythmias Serum K >5 mmol/L (5 meq/L) Kidney failure is the leading cause Can be life-threatening due to risk of ventricular arrhythmias Normal renal response to hyperkalemia Stimulate aldosterone secretion which then stimulates urinary potassium excretion Symptoms Skeletal muscle weakness Paralysis Parasthesias Respiratory failure Decreased renal excretion Reduced GFR Reduced tubular secretion Increased intake Transcellular shifts Common Drugs Metabolic acidosis Tumor Lysis Syndrome Rhabdomyolysis Aldosterone deficiency or resistance Amiloride Spironolactone Cyclosporine/Tacrolimus Heparin ACE inhibitors/ARBs Pentamidine TrimethoprimSulfamethoxazole 3 Na ECF ICF Na= 150 mmol/L K=4 mmol/L Na= 10 mmol/L K=140 mmol/L 2K Reason for K to have shifted outside the cells? K shift to outside the cell after the blood was collected? Hemolysis Tissue hypoxia distal to tourniquet Heel stick Are the kidneys excreting K appropriately? GFR Drugs Aldosterone Excessive dietary K intake contributing to the problem? IVFs and TPN!!! Repeat serum K EKG stat If EKG shows changes, start treatment immediately Progression of changes Peaked T waves-Prolonged PR interval-ST depression-Widened QRS-Ventricular fibrillation Peaked T waves Loss of P wave Widening of QRS ST depression Prolonged PR interval Ventricular dysrhythmias Cardiac arrest Eliminate source of potassium intake or offending drugs K⁺ < 6 mEq/L Low potassium diet Diuretics K⁺ > 6 mEq/L Cation exchange resin: SPS EKG changes = EMERGENCY Stabilize myocardium IV calcium chloride or calcium gluconate (10%) Shift potassium into cells Beta agonists, insulin/glucose, sodium bicarbonate Remove excess potassium from the body Sodium polystyrene sulfonate (SPS) Furosemide Hemodialysis Weakness or paralysis Ileus Cardiac dysrhythmias Delayed depolarization Flat/absent T waves U waves U WAVES BMP Hypernatremia Alkalosis Bartter’s Renin Aldosterone Cortisol If > 2.0 mEq/L and no EKG changes, treat orally with KCl, minimum 2 mEq/kg/day If < 2.0 and/or EKG changes, treat intravenously, with KCl 40 mEq/L into IV fluids “Potassium runs”: not recommended unless cardiac/ICU patient Monitor potassium values until normal value is established A 7 yo male with cystic fibrosis and obstructive lung disease is admitted for a 2 week h/o progressive lethargy. He is obtunded. Labs: Na=105, K=4, Cl=72, HCO3=21 Plasma osmolality= 222mOsm/kg H20 Urine osmolality= 604 mOsm/kg H20 Urine Na= 78 mEq/L What is the most likely diagnosis? Pseudohyponatremia SIADH Psychogenic polydipsia Hypoaldosteronism How would you raise the plasma sodium concentration? Normal=280-295 mOsm/kg Osmotic equilibrium tightly regulated between ECF and ICF compartments Water moves between compartments in response to alterations in osmolality of either compartment 2 [Na⁺] + [BUN] + [Glucose] 2.8 18 • Serum osmolality is tightly regulated • Sodium is the major determinant of serum osmolality • Sodium balance is regulated by the kidney • Serum sodium does not reflect total body sodium content • Na requirements in growing child • 2-3 mEq/kg/day Drawn from an indwelling catheter Hyperlipidemia Normal plasma Osm Hyperglycemia Drives water into extracellular space, diluting the Na concentration ▪ Plasma osm will be high ▪ Na decreases 1.6 mEq/L for each 100 mg/dL rise in glucose Serum Na < 130 mEq/L Loss of sodium Gain of water Most common cause is intravascular volume depletion from gastroenteritis After volume expansion, will be able to regulate free water excretion Lose more salt relative to water but still hypovolemic Hyponatremic dehydration GI losses (prolonged AGE/hypotonic intake) Renal losses Chronic diuretic therapy Salt wasting nephropathy Adrenal insufficiency Skin losses Cystic fibrosis (hyponatremic/hypochloremic) Hypervolemia Fluid overload Congestive heart failure Water intoxication Diluted formula Hypotonic fluids SIADH History and Physical Determine volume status Estimate sodium intake and output If hypovolemic: Renal or Extrarenal losses? Urine Na⁺ Does kidney respond appropriately to hypovolemia? Urine specific gravity Urine osmolality Correct underlying cause Hyponatremic dehydration SIADH ▪ Fluid restriction (insensible water losses) until Na levels normalize Rate of correction depends on how quickly it developed Acute hyponatremia is more dangerous Increased risk of herniation or apnea from increased ICP from rapid, unbalanced water movement into brain cells In general, correction with hypertonic saline in unnecessary unless there are neurological manifestations of hyponatremia Sodium deficit (mEq) = Fluid deficit (L) X 0.6 X [Na⁺] in ECF (mEq/L) PLUS Excess sodium deficit = (Desired Na⁺ - Actual Na⁺) X (0.6 L/kg) X Wt (kg) Desired Na⁺ is 135 mEq/L Maintenance and ongoing losses Replace over 24 hours As sOsm falls, water moves into cells, and risk of cerebral edema If severe (<120 mEq/L), may observe seizures, altered mental status, vomiting For Na⁺ < 120 mEq/L, raise Na⁺ to 125 mEq/L by giving 3% saline Rapid correction of hyponatremia : central pontine myelinolysis EARLY ADVANCED Headache Nausea and vomiting Lethargy Weakness Confusion Altered consciousness Agitation Gait disturbances Seizures Coma Apnea Pulmonary edema Decorticate posturing Dilated pupils Anisocoria Papilledema Cardiac arrhythmias Central diabetes insipidus 2 ml/kg bolus of 3% NaCl, max 100 ml over 10 min Repeat 1-2 times until symptoms improve Goal of correction is 5-6 mEq/L in first 1-2 hours Recheck sNa q 2 hours Moritz et al. Pediatr Nephrol (2010) 25: 1225-1238 Insufficient Correction Cerebral Edema Too aggressive Correction Demyelination •Acute hyponatremia=Most dangerous •Symptomatic hyponatremia = Medical Emergency A 9 yr old boy who has cerebral palsy is admitted to CHNOLA following 4 days of diarrhea. His initial serum Na level is 174mEq/L. Once circulatory volume is restored, the primary focus of the fluid management must be to provide appropriate amounts of: Chloride Free water Glucose Phosphate Potassium Serum sodium >150 mEq/L Always abnormal and should be evaluated Free water deficit Increased sodium intake/retention Increased serum Osm Does not imply total body sodium overload Rarely develops in those who have access to free water Most often from inability to access free water At risk Ineffective breastfeeding Critically ill patients Infants Neurologically impaired Children who have hypernatremic dehydration often appear minimally dehydrated on exam. This is due to maintenance of: Extracellular fluid volume Intracellular fluid volume Total body glucose Total body sodium concentration Total body water balance Water Deficit Renal loss Diuretic use Nephropathy with renal concentrating defect Diabetes insipidus Extrarenal loss Vomiting/Diarrhea Skin losses Increased Sodium Intake/Retention Salt poisoning Exogenous sodium Hypertonic feeding/saline NaHCO3 administration Mineralcorticoid excess Hyperaldosteronism Determine volume status Blood pressure Renal water loss Kidney does not appropriately respond to hypovolemia Low urine s.g and osmolality High urine Na⁺ Extrarenal water loss Kidney responds appropriately to hypovolemia High urine s.g. Low urine Na⁺ Treat cause Correct volume disturbance if present Replace free water deficit 4mL/kg x (desired change in serum Na (mEq/L)) Risk of cerebral edema from rapid correction Stones Renal calculi Bones Bone pain Moans Depression Groans Constipation Symptoms Weakness, irritability, abdominal cramping, n/v, polyuria, polydipsia, renal stones, pancreatitis, shortened QT interval Differential diagnosis Hyperparathyroidism, excessive calcium intake, malignancy, thiazides, prolonged immobilization, sarcoidosis Most hypercalcemic patients are also volume depleted Hydration to increase UOP and Ca excretion NS with potassium at 2-3x maintenance if renal function and BP allow Forced diuresis Furosemide Calcitonin Bisphosphonates Dialysis A 18 month old with ESRD secondary to renal dysplasia on chronic peritoneal dialysis has a serum Mg of 3.2. He is asymptomatic. All other values are normal except his BUN/Cr. What is your next step in management? Change to hemodialysis Increase phosphate binders Increase vitamin D Continue peritoneal dialysis Etiologies Renal failure ▪ Common in CKD due to decreased excretion ▪ Levels in AKI parallel potassium and are derived from the intracellular pool ▪ Rapid cell lysis Excessive administration Symptoms Decreased DTRs, lethargy, confusion Hypocalcemia (hypermagnesemia suppresses PTH) Rarely of clinical significance Treatment Stop supplemental Mg Diuresis Dialysis You are called to the floor at 2 am to see a 16 yo orthopedic post-op patient because his BP is 160/100 What do you do? A 5 yo boy is brought to the ER because of new-onset generalized seizure which has subsided by the time he arrives. He is postictal with BP of 160/100. What do you do? Is this HTN urgency or emergency? HTN Emergency is elevated SBP and DBP with acute end-organ damage Stroke (ischemic/hemorrhagic) Pulmonary edema HTN encephalopathy HTN urgency does not have end organ damage. HA, Nausea, Blurred vision In children, 75% of cases of HTN emergency will be secondary to renal or renovascular causes What do you need to do before treatment? Rule out increased ICP as etiology of HTN Get plasma renin activity level If the patient is bleeding or coagulopathic, treat the elevated BP urgently Worry about hemorrhagic stroke ICU Don’t lower BP too rapidly Lower no more than 20-25% in 1st 8 hours Preserve cerebral perfusion Acute goal is a mildly elevated BP A 5 yo boy is brought to the ER because of new-onset generalized seizure which has subsided by the time he arrives. He is postictal with BP of 160/100. What would you start? What would be your immediate BP goal? Goal around 130/85 (20% reduction) Nitroprusside Arterial and venous vasodilator Very short-acting Easily titrated Cyanide toxicity Don’t use in renal or liver failure IV Calcium channel blockers Nicardipine Can cause increased ICP IV Labetalol Alpha and beta blocker: decreases peripheral vascular resistance Continuous or intermittent dosing Do not use in asthmatics, lung disease, CHF, diabetics IV Enalapril (Enalaprilat) IV hydralazine Potent arterial vasodilator Infants You are called to the floor for a 8 yo child with PIGN who is seizing. His BP is 155/98 What do you do for immediate treatment? IV labetalol bolus dose Transfer to PICU for nicardipine or labetalol infusion Goal is to decrease his BP by 20-25% in first 8 hours What other therapy might be helpful? Lasix- PIGN is assoc with volume overload Severe asymptomatic HTN May have headache Most commonly due to non-adherence or ingestion of large amounts of salt Reduce BP over several hours to days Oral medications Oral medications Nifedipine ▪ Short-acting- see effects in 15-20 min ▪ 0.25 mg/kg initial dose ▪ 10 mg capsules Isradipine ▪ Short-acting: effects within one hour ▪ 0.05-1 mg/kg/dose Labetalol ▪ Heart rate is dose limiting factor