2105Lectures 10abc powerpoint
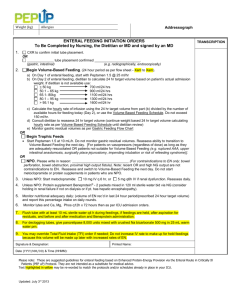
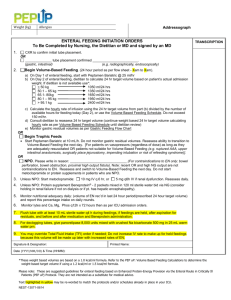
advertisement
Inflammatory bowel disease(IBD)-ulcerative colitis and Crohn’s alterations in microbiome play a role in IBD 1)different oxidative pathways in the altered microbiome 2)more aggressive nutrient uptake by altered microbiome-this favours the altered microbiome 3) altered microbiome is more virulent Exam 180 minutes 120 multiple choice questions-120 points -4 short answer question-60 points multiple choice-lecture 7a-12c inclusive short answer-whole Nutr2105 course Note Nutrition 2106-Fall 2014- Principles of Nutrition in Metabolism Nutrition 2101-Nutritional AssessmentTheory-Fall 2014 Nutrition 2107- Introduction to Sports Nutrition-Winter 2015 Note Nova Scotia now spends 47 cents of every budget dollar on healthcare(10 years ago it was 40 cents) -is the publically funded healthcare system in its present form sustainable? Note Email sent today to first year and senior students. Email is regarding completion of NSEE survey (first year and senior students) . Please complete to help CBU better help you! Lecture 10a 17 March 2014 Enteral and Parenteral Feeding Enteral Feeding -refers to use of intestine (uses oral or tube feeding to direct nutrients to intestine) -called complete enteral feeding if formula is primary source of nutrients -complete formulas can be used in smaller quantities to supplement table foods -complete formulas required if patient is on tube feeding or oral liquid diet for more than a few days Types of enteral formulations -standardised -hydrolysed -modular -characterised by type of protein in the formulation Types of enteral formulations Standardised Appropriate for people who are able to digest and absorb Contain complete proteins (complete refers to whole proteins or combination of protein isolates(purified proteins)) Blenderised formulas contain protein from pureed foods (e.g. blenderised meats) Types of enteral formulations Hydrolysed • Pre-digested protein- so only get small peptides or just free amino acids • Some have medium chain triglycerides or are very low in fat Types of enteral formulation Modular Provide a single nutrient Modules can be combined with other modules or with minerals and/or vitamins to address the specific needs of a patient Candidates for tube feeding Anybody who: •can not get food down orally or •has mental incapacitation •are malnourished or •has high nutrient requirements or extensive intestinal resections or is on a ventilator •gastrointestinal obstructions or fistulas •in short anyone who cannot access or utilise GI tract on their own Distinguishing characteristics of enteral formulations 1) Nutrient density 1.0 kcal/ml- standard 1.2 – 2.0 kcal/ml for nutrient dense formulas -nutrient dense formulations are given in smaller volumes to persons with fluid balance issue- e.g. congestive heart patients Distinguishing characteristics of enteral formulations 2) Fibre if administered over short time - low to moderate fibre - otherwise gas and distension can be an issue if long term administration -then higher amounts of fibre Distinguishing characteristics of enteral formulations 3) Osmolality- measure of concentration of molecular and ionic particles in solution -serum is 300 milliosmoles/kg of solution -isotonic solution is 300 milliosmoles/kg -hypertonic is greater than 300 milliosmoles/kg of solution -hypertonic can induce diarrhea in intestine so a slow introduction of hypertonic solution for intestinal route is essential Tube placement-1) transnasal or 2) direct catheter 1)Transnasal Nasogastric-children and adults-larger nose than infants so nasogastric is used in children and adults Orogastric-infants- smaller nose than adults and children so orogastric is used Nasoduodenal-nose to duodenum Nasojejunal placement-nose to jejunum Tube placement 2) Catheter direct to stomach or jejunum Enterostomies- surgical placement of catheter -Gastrostomy- direct to stomach -Jejunostomy-direct to jejunum Safehandling of formulations Open and closed systems Open- exposed to air Closed-not exposed to air Keep your fingers out of the soup for open systems Initiating and progressing a tube feeding Formula delivery techniques-Intermittent feeding •Best to stomach •No more than 250-400 ml over 30 minutes •Use- depends on tolerance Bolus feeding included here (300-400 ml) in 10 minutes Initiating and progressing a tube feeding Formula delivery techniques Continuous feeding Delivered slowly over 8-24 hours Good for people who have received nothing though GI tract for a long time, hypermetabolising persons and those receiving intestinal feedings Formula volume and strength institutionally based- standard operating procedures (sops) Initiating and progressing a tube feeding Additional matters Supplemental water -standard formulas contain about 850 ml of water/per formula -most people need about 2 L of water per day Gastric residual volume -amount left over from previous feedings-significance of this? 2 Youtubes- enteral feeding https://www.youtube.com/watch?v=EWtqxJeyCMA https://www.youtube.com/watch?v=hploKHe-V4U Class activity Design an enteral feeding for the pathology/problem of your choice that meets the dietary principles of adequacy, variety, moderation, nutrient density, energy control, and balance Lecture 10b 17 March 2014 Parenteral Feeding Parenteral Feeding (going around ie circumventing the intestine) Nutrients go directly into blood stream bypassing gastrointestinal tract-this is done by intravenous needle or catheter Used when a patient cannot, due to physical or psychological impairment, consume sufficient nutrients enterally Used when patients gi system will not adequately process food for body Actual infusion depends on site of infusion and patient’s fluid and nutrient requirements Types of Parenteral Nutrition Peripheral parenteral nutrition (PPN)peripheral vein used Total parenteral nutrition (TPN)-superior vena cava used Basic difference between the two is the concentration of nutrients infused (higher concentration is used for TPN due to more rapid dilution in superior vena cava) Parenteral Feeding Usual fluid volume is 1.5-2.5 L over a 24 hour period for most people Parenteral Feeding Composition of ingredients in bag for intravenous delivery Dextrose Amino acids Lipid emulsion Sterile water Electrolytes Vitamins Carbohydrate Dextrose- provides 3.4 kcal/g and not 4 kcal/g -difference is due to what? Concentration is 12.5 % (max for peripheral introduction) to 25 % (total parenteral nutrition) Restricted in ventilator patients because oxidation of glucose produces more carbon dioxide than does oxidation of fat Protein Mixture of essential and non-essential amino acids Concentration 3.5-15 % Quantity of amino acids depends on patients estimated requirements and hepatic and renal function-why? Lipid emulsions Safflower and soybean oil with egg lecithin used as an emulsifier (why the emulsifier and how does it work?) Isotonic Significant source of calories Lipid emulsions Available in 10, 20, 30 % concentrations supplying 0.9 and 1.8 and 2.7 kcal/ml respectively-Do the math Usual dose is 0.5 to 1 g/kg/day to supply 20-30 % of total kcal requirement IV fat contradicted for severe hepatic pathology, hyperlipidemia or severe egg allergies Used cautiously with atherosclerosis, blood coagulation disorders Electrolytes Dictated by patients blood chemistry values and physical assessment findings Standard multivitamin and trace mineral preparations added to parenteral solutions to meet micronutrient needs PPN -must be isotonic and therefore low in dextrose and amino acids to prevent phlebitis and increased risk of thrombus formation -need to maintain isotonic solutions of dextrose and amino acids while avoiding fluid overload limits the caloric and nutritional value of PPN PPN delivers complete but limited nutrition the final concentration cannot exceed 12.5 % dextrose-also uses lower concentrations of amino acids vitamins and minerals are added lipid emulsion may be added to supplement calories depending on the patients tolerance PPN -provides temporary nutritional support -short term- 7-10 days and do not require more than 2000 to 2500 kcal per day PPN -may be used for a post surgical ileus or anastomotic leak or for patients who require nutritional support but are unable to use TPN because of limited accessibility to a central vein -sometimes used to supplement an oral diet or tube feeding or transition from TPN to enteral intake TPN Hypertonic solutions provide more dextrose and/or protein but they must be delivered centrally in a large diameter vein so that they can be quickly diluted TPN TPN is used when nutritional requirements are high and anticipated need is relatively long 3 litres of 10 % dextrose provides only 1020 kcal -calculation TPN -traditionally-catheter to superior vena cava figure 21-2 TPN Indications: severe malnutrition GI abnormalities : due to obstruction, peritonitis, severe acute pancreatitis after surgery or trauma especially that involving extensive burns, sepsis need for supplementation of inadequate oral uptake in patients who are being treated aggressively for cancer bone marrow transplantation TPN cyclic -constant infusion for 8-12 hours -used for home patients -used to support inadequate oral intake -allows insulin and glucose to drop when infusion is not taking place -switch from continuous TPN to cyclic TPN should be gradually decreased by several hours per day and signs of glucose overload and fluid imbalance should be monitored Note Lecture 10c 17 March 2014 Surgery and Burns Surgery -patient should be well nourished prior to surgery-this gives better recovery -however, surgical patients are often malnourished due to anorexia, nausea, vomiting, burns, fever, malabsorption, and blood loss -surgical prep- range of actions include: -high calorie protein diet -enteral feeding -parenteral feeding Surgery -nothing by mouth (NPO) for a least 8 hours prior to general anesthesia due to risk of aspiration -oral intake is resumed after bowel sounds return- usually 24-48 hours after surgery -start with clear liquids to full liquids to soft or regular diet as tolerated post-op -usually a high protein high calorie diet is appropriate-this helps with healing Burns -hypermetabolism involved- why? -large quantities of nutrients leech through burn area -therefore fluid and electrolyte imbalances are a problem Burns -result in anorexia, pain, emotional trauma, weight loss and immune incompetence, malnutrition Burns -after fluid and electrolytes are addressed and by hour 72 (if bowel sounds)- oral intake begins -if no bowel sounds by hour 96 then PPN or TPN Burns - regardless of routes of administration -Protein 1.5-3.0 g /kg body weight/day 20-25 % protein, 50 % carbohydrate, 25 % fat -Kcal- additional 40-60 kcal/kg body weight/day -high fluid intake –including more potassium, zinc and vitamins A and C (zinc, vitamins A and C for wound healing) and vitamins B1, B2 and B3 (in proportion to increased energy intake) Table 29-1, p. 870 Table 29-2, p. 903 Table 29-3, p. 904 Cancer Dietary factors - cancer initiators - these dietary components start cancer -additives and pesticides are of particular but not exclusive concern here -stomach cancer particularly high in parts of world where pickled or salt-cured foods that produce carcinogenic nitrosamines are consumed Cancer Dietary factors -alcohol associated with high incidence of some cancers, especially of the mouth, esophagus and liver in all persons and breast cancer(postmenopausal) in females -beer and scotch may contain nitrosamines -wine and brandy may contain urethane -urethane and nitrosamines are carcinogens -moderation is the key to prevention here Dietary factors –cancer promoters and inhibitors -cancer promoters accelerate the rate of progression of cancer once it has started - eg excess dietary fats -linoleic acid- has been suggested to promote -omega 3s have been suggested to prevent or delay cancer development Dietary factors-antipromoters Fruits and veggies as per Canada’s food guide -fibre speeds up gi transit time thus reducing carcinogen exposure -fruits and vegetables containing antioxidants that scavenge free radicals –such free radicals contribute to cancer -various phytochemicals activate enzymes that can destroy carcinogens Once cancer starts -do nutritional assessment and respond accordingly -early dietary intervention prepares body for stresses that lay ahead AIDS Weight loss, diarrhea, seborrhea, eczema, fever, sweating-nutritional implications? Nutritional implications can further deteriorate patient’s health e.g. further immune response compromise Kcal requirement is increased compared to non-infected persons in good health Protein requirements 1-2 g/kg bw/day due to lean body mass loss and other protein losses AIDS Drugs can exacerbate nutritional difficulties (table) AIDS Fat – medium chain triglycerides(mct) (6-12 carbon fatty acids) for additional calories -lipase and bile not required for mct- therefore easier absorption AIDS Vitamins and Minerals recommendation-close to DRI-otherwise adverse interactions with antiretroviral drugs AIDS Feedings -small, numerous meals -liquid commercial preparations -antidiarrheals shortly before meals -high soluble fibre foods like oatmeal, cooked carrots, bananas, peeled apples and apple sauce may help slow transit time (diarrhea reduced perhaps)