Fluid and Electrolytes
advertisement
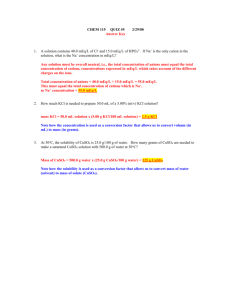
Fluid and Electrolytes Kathleen W. Bartlett, MD August 2, 2007 Pop Quiz SB is an 18 month old male weighing 11 kg. What would be the appropriate maintenance IVF and rate for this patient? Answer: D5 ¼ NS + 20 mEq KCl/L at 42 ml/hour. Maintenance Fluids What is the scientific basis for our administration of IVF? Is there evidence to support the safety and efficacy of IVF administration in children? What are the complications of IVF administration in children? Maintenance Requirements Maintenance fluid and electrolyte needs stem from basal metabolism. Metabolism creates two by-products: – Heat: dissipated through skin and respiratory tract as “insensible losses” – Solute: excreted in the urine Insensible losses contribute 1/3 of fluid needs, while urinary losses contribute 2/3. Metabolic Rate Not directly related to weight Expressed in units of energy (kcals) High in newborn period Low in adults Transition is not linear Adults need less fluid per unit of body weight than infants and children. Fluid and electrolytes per kcal of basal metabolism remain constant. Basal metabolic rate, normal activity and average hospitalized patient Roberts, K. B. Pediatrics in Review 1999;20:429-430 Copyright ©1999 American Academy of Pediatrics General Concepts For each 100 kcals burned, the body needs – 100 ml water – 3 mEq Na – 2 mEq K Because we don’t have basal metabolic rates memorized for various ages, we have three methods to approximate these needs for us. Maintenance Requirements Caloric Expenditure Method Body Surface Area Method Holliday-Segar Method Maintenance requirements are over 24 hours but do not have to be given evenly divided over each hour. Caloric Expenditure Method Caloric needs are based on resting energy expenditure (=basal metabolic rate) plus activity factors Resting energy expenditure is based on size Energy needs increase with injury, fever, growth, etc; these are the “activity factors” Uses tables to find appropriate REE, then adds coefficients for activity factors. Bottom Line: NOT USER FRIENDLY! Body Surface Area Method Requires knowledge of height and weight Then use calculation or table to determine BSA Maintenance requirements are about 1500 ml/m2/day Used exclusively by some pediatric institutions (e.g. St. Louis Children’s Hospital) Holliday-Segar Method Estimates caloric and fluid needs from weight alone, for simplicity Based on computed caloric expenditure in hospitalized patients. Can under-estimate fluid needs in fever and injury Method we tend to use most commonly 4,2,1 rule Basal metabolic rate, normal activity and average hospitalized patient Roberts, K. B. Pediatrics in Review 1999;20:429-430 Copyright ©1999 American Academy of Pediatrics Holliday-Segar Method Weight ml/kg/day ml/kg/hr First 10 kg 100 4 Second 10 kg 50 2 Each additional 20 1 kg e.g. 25 kg 1000+500+100 40+20+5 = 65 =1600 ml/day ml/hr (1560 ml/day) Glucose D5 (5% Dextrose) can run safely through a PIV and maintains euglycemia. 5g glucose per 100 ml at 3.4 kcals/gram 170 kcals/ liter of D5 – 1600 ml of D5 has only 272 kcals – only 11 kcal/kg/day Patients are malnourished when they only receive IVF! Electrolytes Electrolyte Requirements: – Na = 3 mEq per 100 kcals = 3 mEq per 100 ml water (or 30 mEq/L) – K = 2 mEq per 100 kcals = 2 mEq per 100 ml water (or 20 mEq/L) Fluid composition: – NS = 0.9% NaCl = 154 mEq NaCl/L – ¼ NS = 38.5 mEq NaCl/L The commercially available fluid that most closely approximates the electrolyte requirements for maintenance is D5 ¼ NS + 20 mEq KCl/L. D5 ¼ NS for infants and D5 ½ NS for older children and adults? The sodium concentration should NOT differ: – Na needs are 3 mEq/100 kcals, not 3 mEq/kg. – Na needs are not linear; they should decrease like water needs do. – Therefore, the ratio of Na to water should remain constant. Holliday and Segar argue that D5 ¼ NS with 20 mEq of KCl per liter is an appropriate maintenance fluid for all people. The Debate about Sodium 2004 case-control study identified 40 children who developed hyponatremia while in the hospital. The patients in the hospital-acquired hyponatremia group received significantly more free water than controls. Hoorn EJ, Geary D, Robb M, Halperin ML, Bohn D. Acute hyponatremia related to intravenous fluid administration in hospitalized children: an observational study. Pediatrics. 2004 May;113(5):1279-84. Why hyponatremia? ADH (anti-diuretic hormone) increases in response to stress: – surgery, pain, fever, nausea, bronchiolitis, meningitis, pneumonia, CLD, or in response to certain drugs When ADH increases, renal solute load is excreted in a smaller volume of urine. In this setting hypotonic fluid administration can lead to free water overload and hyponatremia. Why hyponatremia? Estimating caloric need in illness is difficult – it could be much less than in healthy children. Insensible losses may have been overestimated. The authors argue for isotonic fluid (D5NS) as the maintenance fluid for post-op pts and when Na < 138. Other authors have advocated isotonic fluid for all patients. Where is the evidence? 2006 systematic review found 6 studies comparing isotonic to hypotonic fluid for hospitalized children. – 3 observational studies, 2 “unmasked” RCTs, and one nonrandomized, controlled trial. – 4 studies done in post-op surgical patients, 1 in patients with gastroenteritis, and 1 case-control. Hypotonic IVF increased the odds of developing serum Na < 136 (OR 17.22; 95% CI 8.67 to 34.2). Greater patient morbidity in hyponatremia group (seizures, pulmonary edema, nausea/vomiting) Studies poorly designed and heterogeneous, making bias possible. Authors recommend isotonic fluids as “more physiological, and therefore a safer choice.” Choong K, et al. Hypotonic versus isotonic saline in hospitalised children: a systematic review. Arch Dis Child. 2006 Oct;91(10):828-35. Problems with isotonic fluid for maintenance May lead to excessive sodium loading in patients with cardiac or renal disease (not observed in any of studies included in systematic review). Does not treat SIADH (fluid restriction more appropriate). Does not correct hypovolemia which may be causing appropriate ADH secretion. Holliday MA; Friedman AL; Segar WE; Chesney R; Finberg L. Acute hospital-induced hyponatremia in children: a physiologic approach. J Pediatr 2004 Nov;145(5):584-7. Conclusion about sodium Iatrogenic hyponatremia is a real and preventable medical error. Do not use maintenance fluids to replace deficits (i.e. giving a patient 2 x MIVF). Giving a bolus of isotonic solution in volume-depleted children may decrease ADH secretion. However, isotonic fluid will not prevent hyponatremia in patients with SIADH. Conclusion about sodium For now continue to use Holliday-Segar method for maintenance fluid while – Following serum sodium – Being mindful of situations that lead to increased ADH. “…no one fluid rate or composition is suitable for all patients, and the administration of any intravenous fluid should be considered an invasive procedure, requiring close monitoring.” Moritz MJ, Ayers JC. “Hospital acquired hyponatremia: why are there still deaths [commentary]? Pediatrics. 2004;113:1395-96. Dehydration Diarrhea Acute gastroenteritis is common in children. Average of 1.3-2.3 episodes of diarrhea per child per year for children younger than 5 in the U.S. 1.5 million pediatric office visits >200,000 hospitalizations 300 preventable deaths Rotavirus is most common cause (1/3 of all hospitalizations) and costs $250 million per year in direct medical costs. Dehydration Assessment of dehydration Initial resuscitation Determining deficit Adding in maintenance Ongoing losses Assessment of dehydration Recent weight changes (gold standard) Physical exam findings Dehydration Mild (5%) Moderate (10%) Severe (15%) Turgor Normal Tenting None Cap Refill Brisk (<2 secs) 2-4 seconds >4 seconds Mucous membranes Moist Dry Parched/cracked Eyes Normal Deep set Sunken Tears Present Reduced None Fontanel Flat CNS Consolable Irritable Lethargic/Obtunded Pulse Regular Slightly increased Increased Urine output Normal Decreased Anuric Sunken Is this child dehydrated? Systematic review of the published data on history, PE, and labs in dehydration revealed: – Poor to moderate inter-observer agreement – History and parental report have limited value – Best individual tests Prolonged capillary refill Abnormal skin turgor Abnormal respirations – Groups of positive signs are most helpful – Extremely abnormal lab tests are helpful Steiner MJ, DeWalt DA, Byerley JS. Is this child dehydrated? JAMA. 2004 Jun 9;291(22):2746-54. Conclusions Focus on symptoms and signs with proven utility. Ability to estimate exact degree of dehydration is limited. Support change to “none (<3%), some (39%), or severe (>9%)” classification method recommended by CDC and WHO. WHO assessment of dehydration King CK, Glass R, Bresee JS, Duggan C. Managing acute gastroenteritis among young children. MMWR. November 21, 2003/52 (RR16):1-16. Fluid management in shock Initial boluses of 10 - 20 ml/kg given quickly – 20 ml/kg is 2% of body weight – therefore it should reduce 10% dehydration to 8% dehydration. – One bolus is not enough to replace a deficit when someone is dehydrated. – Reassessment is key! Use isotonic solutions (NS, LR) Consider blood, other fluids and/or pressors in special circumstances – Trauma or blood loss, nephrotic syndrome, septic and cardiogenic shock Fluid Composition Fluid CHO KCal/L Na 5 170 K Cl CO3 Ca 28 3 g/100cc D5W 154 NS 154 (0.9% NaCl) LR 0-10 0-340 130 4 109 IV Rehydration First resuscitate out of shock – restore perfusion Calculate maintenance, including ongoing losses, and deficit Run maintenance as usual Replace ongoing losses Typically replace deficit over 24 hours – Half in first 8 hours – Other half over 16 hours Replacement should be done in relation to the rate that the loss occurred Where the deficit is coming from— the traditional teaching For a brief duration of illness (<3 days), 80% of the deficit is from the extracellular fluid space (ECF) After more than 3 days of illness, the deficit from the ICF increases to about 40% (therefore 60% from ECF) ECF contains a lot of Na (135-145 mEq); ICF contains a lot of K (150 mEq) Case # 1 JW is a previously healthy 6 mo male who presents with a 4-day history of low-grade fever, vomiting and diarrhea. He has been unable to tolerate PO. Mom reports that he has lost 1 ½ lbs since his well-child check last week. On exam, he weighs 7 kg. He is mildly tachycardic and tachypneic. He is listless. He has a slightly sunken fontanelle, dry mucous membranes and delayed CR (~3 secs). Example Calculations, normal Na 7 kg infant with 10% dehydration that accumulated over >3d. 24 Hours H2O Na K Maintenance (Hol.-Seg.) 700 21 14 Deficit (8% of 7 kg) 560 ECF (60%) 336 ICF (40%) 224 Total 49 (145 MEq/L x 0.336 L) 34 (150 MEq/L x 0.224 L) 1260ml 70mEq 48 mEq First 8 hours MIVF for the first 8 hours + 50% of the deficit 1/ 3 Maint ½ Deficit Total H2O Na K 233 7 5 280 513 24 31 17 22 513/8 = 64 ml/hr 31/0.513= 22/0.513= 60 mEq 43 mEq Na/L K/L Roughly D5 ½ NS (77 mEq/L) + 40 mEq KCl/L at 64 ml/hr Next 16 hours MIVF for 16 hours + other 50% of the deficit. H2O Na K 467 14 9 ½ Deficit 280 24 17 Total 747 38 26 747/16= 47 ml/hr 38/0.747= 26/0.747= 51 mEq/L 35 mEq/L 2/ 3 Maint Roughly D5 ¼ NS (38.5 mEq/L) + 30 mEq KCl/L at 47 ml/hr Simplified – fluid choice, normal Na (Roberts’ method) Usually after boluses with NS or LR, D5 ½ NS is an appropriate rehydration fluid After urine output is assured, give K as 20 MEq/L – That is usually safe – Often you don’t need to fully replete K losses acutely – Watch the rate of fluids regarding K and don’t give more than 1 mEq/kg/hr Roberts, KB. Fluid and electrolytes: parenteral fluid therapy. Pedatr. Rev. 2001;22:380-387. Simplified Rate (Roberts’ method) If a child is 10% dehydrated: Give a 20 ml/kg bolus of NS – Restores hydration 2% Next give 10 ml/kg/hr of D5 ½ NS with 20 KCl for 8 hours – Restores hydration 8% Next give 1.5 times MIVF using D5 ¼ NS with 20 KCl for 16 hours – The whole day’s maintenance Case #1 using Roberts’ Method 7 kg child with 10% dehydration Bolus of 140 ml NS 70 ml/hr of D5 ½ NS with 20 KCL for 8 hours, then 40 ml/hr of D5 ¼ NS with 20 KCL for 16 hours Hyponatremia Hyponatremic patients appear more dehydrated than they are. Risk of rapid correction is central pontine myelinolysis. Correct the Na fast only if the patient is symptomatic (seizing or particularly irritable) For asymptomatic patients, the goal should be to increase the Na no faster than 1 mEq/L per hour. Now suppose JW has Na=115 Fluid deficit is the same. Na deficit from dehydration is the same. K deficit is the same. Excess Na deficit: – (Desired Na – Actual Na) x distribution factor x wt – (135-115) mEq Na/L x 0.6 L/kg x 7 kg = 84 mEq Na Make a table! Component Maintenance Na=3mEq/100ml K=2mEq/100ml Deficit 60% ECF x 700 = 420 40% ICF x 700 = 280 Excess Na (135-115) x .6 x deficit 7kg 24 hour totals H2O (mL) 700 Na (mEq) 21 K (mEq) 14 700 61 42 84 1400 166 56 First 8 hours—hyponatremia MIVF for the first 8 hours + 50% of the deficit 1/ 3 Maint ½ Deficit Total H2O Na K 233 7 5 350 583 72 80 21 26 583/8 = 73 ml/hr 80/0.583= 26/0.583= 137 mEq 45 mEq Na/L K/L Roughly D5 ½ NS (77 mEq/L) + 40 mEq KCl/L at 73 ml/hr Next 16 hours MIVF for 16 hours + other 50% of the deficit. H2O Na K 467 14 9 ½ Deficit 350 72 21 Total 817 86 30 817/16= 51 ml/hr 86/0.817= 30/0.817= 105 mEq/L 37 mEq/L 2/ 3 Maint Roughly D5 ½ NS (77 mEq/L) + 30 mEq KCl/L at 51 ml/hr Hypernatremia Hypernatremic patients may appear less dehydrated than they really are. In hypernatremia, rehydrate more slowly to avoid fluid shifts that could cause cerebral edema or intracranial bleeding The hypernatremic dehydrated patient is still total body sodium depleted, but in addition has lost free water Free water losses must be calculated and subtracted from total deficit to calculate the solute deficit. Now JW has Na=155 Same fluid deficit and maintenance requirements FW deficit= [Na]actual – [Na]desired x 1000 ml/L x 0.6L/kg = ml/kg [Na]actual FW deficit= (155-145) ÷ 155 x 0.6 L/kg x 7 kg= 0.270 L Replace free water deficit evenly over 48 h – Give only half of deficit in first 24 hours. Subtract the free water deficit from the total deficit when calculating Na and K deficits from dehydration. Decrease Na by less than 15 MEq/L/day Follow electrolytes closely Table for Hypernatremia, first 24 h H2O Na K MIVF 700 21 14 Free water deficit = 270cc/2 days 135 Def remaining (solute) =420cc (700-270=430) ECF (60%) ICF (40%) Total, 24 hr 258 172 37 1265 58 27 41 Fluid Choice—hypernatremia 1265 ml/ 24 hours = 53 ml/ hr 58/1.265 = 46 mEq/L Na 41/1.265 = 32 mEq/l K Roughly D5 ½ NS with 30 KCl at 53 ml/hr – Could also use D5 ¼ NS (half is more conservative) Practical approach to hypernatremia Still bolus the hypernatremic patient with NS if needed. To lower the Na slowly, start with D5 ½ NS and remeasure. The calculations almost always come out to something near ¼ NS, so that is also a reasonable starting point. The important thing is to follow the sodium carefully and adjust as necessary. Conclusions Intravenous fluid is very important therapy, but a frequent source of medical error. Think about isotonic maintenance fluids in patients at risk for SIADH. Treat hypovolemia carefully—do not just increase the rate of maintenance fluids. Hyponatremia and hyponatremia require extra caution with fluid calculations. Reassess frequently and follow electrolytes.