Health IT
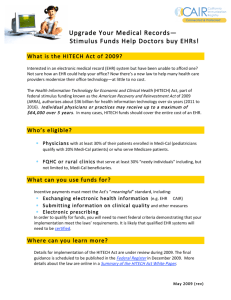
advertisement
Yesterday, Today, and Tomorrow Judy Murphy, RN, FACMI, FHIMSS, FAAN Deputy National Coordinator for Programs & Policy Office of the National Coordinator for Health IT Department of Health & Human Services Washington DC 0 A look at . . . • Yesterday - what we’ve gotten done – The status of the HITECH Programs • Today - what are our key priorities – Health information exchange – Patient engagement • Tomorrow – what are the biggest challenges in our future – Meaningful use of meaningful use – Health reform 1 We’ve come a long way … 2 A Bit of History … On the eve of the Presidential Election President Bush’s goal in January 2004 “… an Electronic Health Record for every American by the year 2012. By computerizing health records, we can avoid dangerous medical mistakes, reduce costs, and improve care.” - State of the Union address, January 20, 2004 Executive order established the Office of the National Coordinator for Health IT (ONCHIT) as part of the Dept of Health & Human Services – Dr. David Brailer appointed the first National Coordinator for Health IT – Followed by Dr. Rob Kolodner President Barack Obama’s goal in January 2009 “To lower health care cost, cut medical errors, and improve care, we’ll computerize the nation’s health records in five years, saving billions of dollars in health care costs and countless lives.” - Speech at George Mason University, January 12, 2009 February 17, 2009 – HITECH Act (part of ARRA) is signed into law – – – – Dr. David Bluementhal appointed National Coordinator Health IT Policy and Standards Committees are formed ONC grows from around 30 to over 150 employees Dr. Farzad Mostashari becomes the current National Coordinator 3 A Remarkable Journey 4 Progress of Eligible Providers toward EHR Incentive Payments as of 8-31-12 NAMCS Survey: • The percentage of primary care providers who have adopted EHRs in their practice has doubled from 20 % to 40 % between 2009 to 2011 Note: The 2012 data will be available in 2013 Source: CMS EHR Incentive Program Data 5 EHR Adoption of Eligible Providers by state as of 8-31-12 http://dashboard.healthit.gov/HITadoption/ 6 Regional Extension Centers are working with 148,448 Primary Care Providers Includes 70% of all primary care providers in the rural areas and 1,185 Rural or Critical Access Hospitals 2012 GAO Report: Providers 2.3 times more likely to achieve MU if working with an REC http://dashboard.healthit.gov/rec/ 7 Progress of Eligible Hospitals toward EHR Incentive Payments as of 8-31-12 AHA Survey – in one year, from 2010 to 2011: • Hospitals increased their use of Basic EHRs from 19% to 35% (84%) • Hospitals doubled their use of Comprehensive EHRs from 4% to 9% (125%) Note: Totals reflect the number of unique hospitals that have received payments from Medicare or Medicaid. Note: The 2012 data will be available in early 2013 Source: CMS EHR Incentive Program Data 8 EHR Adoption of Eligible Hospitals by state as of 8-31-12 http://dashboard.healthit.gov/HITadoption/ 9 Meaningful Use – All Payments as of 8-31-12 ($ in Millions) Payments to All Eligible Professionals and Hospitals Under the Medicare or Medicaid EHR Incentive Programs $900 $8,000 $836 Cumulative Total $7,120 $800 Source: CMS EHR Incentive Program Data $659 $619 $608 $600 $563 $6,000 $620 $586 $5,000 $505 $500 $428 $387 $400 $4,000 $396 $3,000 $276 $300 $237 $2,000 $200 $116 $109 $80 $100 $22 $0 Cumulative Amount Paid (Millions) Amount Paid per Month (Millions) $700 $7,000 $16 $26 $1,000 $31 $0 10 HITECH Framework for MU of EHRs Taken from: Blumenthal, D. “Launching HITECH,” posted by the NEJM on 12-30-2009. 11 Health IT Resource Center THEN: Work within REC community to share knowledge NOW: Work with all external communities to share knowledge Tools Beacon HIE CCC REC SHARP Resources Communities of Practice (CoPs) National Learning Consortium HealthIT.gov 12 Workforce Training – Community College Program Enrollment & Graduation Students Enrolled or Completed: 21,321 13 Workforce Training - University-Based Program Enrollment & Graduation As of September 14, 2012 Students Enrolled or Graduated: 1,627 (Target: 1,685) 14 Health Information Exchange - Directed Exchange Implementation as of 6-30-12 Summary Stats States/territories with directed exchange options broadly available States/territories piloting directed exchange solutions States/territories with directed exchange options unavailable Number of Grantees 36 10 10 15 Directed Exchange: Estimated number enabled as of 6-30-12 Summary Stats Total number of organizations enabled for directed exchange nationally Total number of clinical & administrative staff enabled for directed exchange nationally Number 8.349 48,649 16 Query-Based Exchange: Estimated number enabled as of 6-30-12 Summary Stats Total number of organizations enabled for query-based exchange nationally Total number of individuals enabled for query-based exchange nationally Number 3,554 56,496 17 Exchange is increasing across the nation 18 states had more than 10% of their hospitals actively engaged in sharing health information electronically as of 6-30-12 State Delaware Vermont Michigan Arkansas New York Minnesota North Dakota Colorado California Alaska Utah % of Acute Care Hospitals Actively* Participating in Directed Exchange that is supported or enabled by State HIE grantees** 100% 79% 48% 45% 42% 34% 34% 26% 20% 18% 14% State Delaware New York Maryland New Jersey Arizona Colorado Nebraska Idaho Kentucky Michigan Tennessee % of Acute Care Hospitals Actively* Participating in Query-Based Exchange that is supported or enabled by State HIE grantees** 67% 65% 54% 32% 27% 26% 20% 17% 16% 15% 12% * Active = at least one directed message sent between production end points or at least one patient record query during previous calendar quarter ** Data self-reported by HIE grantees, Denominators calculated with 2011 Medicare Inpatient Hospital Data 18 The Beacon Community Program: Where HITECH Comes to Life 17 diverse communities, each funded over 3 yrs to: Build and strengthen health IT infrastructure and exchange capabilities - positioning each community to pursue a new level of sustainable health care quality and efficiency over the coming years. Improve cost, quality, and population health - translating investments in health IT in the short run to measureable improvements in the 3-part aim. Test innovative approaches to performance measurement, technology integration, and care delivery - accelerating evidence generation for new approaches. 19 “Beacons for Public Health” • Funded by the CDC and launched in collaboration with the ONC in 2011 • Primary goal: Gain an understanding of the range of activities currently conducted in population and public health within the Beacon Communities, to accelerate the work of other organizations across the country Western New York Beacon Community Buffalo, NY Southeastern Minnesota Beacon Community Rochester, MN Rhode Island Beacon Community Providence, RI Southeast Michigan Beacon Community Detroit, MI Greater Cincinnati Beacon Community Cincinnati, OH • Case studies available today! Southern Piedmont Beacon Community Concord, NC San Diego Beacon Community San Diego, CA Crescent City Beacon Community New Orleans, LA 20 20 IT-Care Management Partnership: Beacons and AF4Q Bangor Beacon Community Brewer, ME Maine Alliance Southeastern Minnesota Beacon Community Rochester, MN Humboldt County Alliance • Partnership to align “regional health care improvement” programs between ONC (Beacons) and RWJ (Aligning Forces for Quality or AF4Q) • On October 24th, pioneering organizations from both programs came together to understand opportunities and gaps related to IT and care management Wisconsin Alliance Western NY Alliance Cleveland Alliance Keystone Beacon Community Danville, PA Southern Piedmont Beacon Community Concord, NC • Lessons will be shared through case studies and videos • Future topics: Behavioral health and IT, and data use agreements across communities 21 21 Connecting Health IT to Payment Bangor Beacon Community Brewer, ME • Bangor Beacon HIT infrastructure serves as the foundation for the Bangor Pioneer ACO • 3 Beacon Communities (CO, Tulsa and Cincinnati) are working on how Beacon HIT infrastructure can be used to support provider practices participating in CMMI’s comprehensive primary care initiative (CPC) Greater Cincinnati Beacon Community Cincinnati, OH Colorado Beacon Community Grand Junction, CO Great Tulsa Health Access Network Beacon Community Tulsa, OK 22 22 22 EHR Certification Program: Certified Health IT Product List (CHPL) • 1,642 “Unique” Certified EHR Products as of 11/01/12 Ambulatory Complete EHR 694 Modular EHR 436 Total 1130 Inpatient 96 416 512 Total 790 852 1642 This table shows a unique count of products. Any additional versions of the same products are not included. • 2,744 Certified EHR Products when all product versions are counted • 896 EHR Vendors/Developers • On October 4th, ONC’s Permanent Certification Program was launched; the Temporary Certification Program which was operating for 2 years was sunset 23 MU Attestations by Vendor (7/28/12) http://www.modernhealthcare.com/article/20120728/MAGAZINE/307289983 24 TODAY - Key Priorities: Keeping the Patient at the center of all we do • Patient-Centric health care and health record by – Laying the groundwork for interoperability with standards, testing & certification – Facilitating broad implementation of health information exchange • Patient Engagement by enabling patient – Access – Action – Attitude 25 Focus on INTEROPERABILITY in the Stage 2 Meaningful Use Criteria • E-prescribing (ambulatory and inpatient discharge) • Transition of Care summary exchange: • Create & transmit from EHR • Receive & incorporate into EHR • Lab tests & results from inpatient to ambulatory • Public health reporting – transmission to: • Immunization Registries • Public Health Agencies for syndromic surveillance • Public health Agencies for reportable lab results • Cancer Registries • Patient ability to View, Download and Transmit their health data to a 3rd Party • Create an export summary of patient data, in order to enable data portability 26 Focus on PATIENT ENGAGEMENT in the Stage 2 Meaningful Use Criteria • Reminders for preventive/follow-up care provided • Educational resources identified and provided • Online access to personal health information (portal, PHR) • Visit Summaries provided • Patients can send secure messages to their provider • Patients can View, Download and Transmit to 3rd Party 27 Back in the Day… “The obedience of a patient to the prescriptions of his physician should be prompt and implicit. [The patient] should never permit his own crude opinions as to their fitness to influence his attention to them.” - AMA’s Code of Medical Ethics (1847) 28 And Now… “Patients share the responsibility for their own health care….” - AMA’s Code of Medical Ethics (current) “Patients can help. We can be a second set of eyes on our medical records. I corrected the mistakes in my health record, but many patients don't understand how important it will be to have correct medical information, until the crisis hits. Better to clean it up now, not when there’s time pressure.” – Dave deBronkart (ePatient Dave) 29 ONC’s Consumer Engagement Strategy: The Three A’s Access Attitudes Support a shift in attitudes and expectations regarding consumer (and provider) roles. Give consumers electronic access to their health information. Action Action Catalyze development of tools and services that help consumers (and providers) take action using their health information. ACCESS: Consumer eHealth Pledge Program Over 400 organizations have Pledged to provide access to personal health information for 1/3 of Americans… 31 Taking the Blue Button nation-wide www.healthit.gov/pledge • Get more organizations to offer Blue Button • Make “Blue Button” a household name = “electronic access to my health data” • Advance technical capabilities = “set it and forget it” • One of 5 game-changing projects involving the 2012 Presidential Innovation Fellows 32 ACTION: Making it easier for Patients to use Health IT • Surgeon General’s Healthy Apps Challenge More at: http://sghealthyapps.challenge.gov • PHR Model Privacy Notice More at: http://bit.ly/qfjP1a 33 ACTION • Blue Button Mash-Up Challenge – develop an app that mashes up PHR data with other health-related data sets • Leon Rodriguez, Director-Office of Civil Rights: clarification of the patient’s right to access their own health information under HIPAA (videos, pamphlets, answers to questions, and other guidance) More at: http://www.hhs.gov/ocr/privacy/hipaa/understanding/consumers/righttoa ccessmemo.pdf 34 ATTITUDE: Health IT Animation http://www.healthit.gov/patients-families/video/preview-health-it-yougiving-you-access-your-medical-records • 1 and 3 minute versions of the animation are available to use for patient teaching 35 Beat Down Blood Pressure Consumer Video Challenge 36 Beat Down Blood Pressure Winner A Regular Guy Beats Down Blood Pressure: http://vimeo.com/42121895 37 What’s in Your Health Record Consumer Video Challenge 38 What’s in Your Health Record Winner Wright and Luft: http://vimeo.com/46790323 39 TOMORROW – The biggest challenges in our future Improved outcomes Advanced clinical processes Data capturing and sharing Stage 3 Stage 2 Stages of Meaningful Use Stage 1 40 HIT as the means, not the end Dr. David Blumenthal, previous National Coordinator of HIT, emphasizes “HIT is the means, but not the end. Getting an EHR up and running in health care is not the main objective behind the incentives provided by the federal government under ARRA. Improving health is. Promoting health care reform is.” - At the National HIPAA Summit in Washington, D.C. on September 16, 2009 41 Best Care at Lower Cost The Path to Continuously Learning Health Care in America September 2012 iom.edu/bestcare 10 Recommendations Foundational elements 1. The digital infrastructure – Improve the capacity to capture clinical, delivery process, and financial data for better care, system improvement, and creating new knowledge. 2. The data utility – Streamline and revise research regulations to improve care, promote the capture of clinical data, and generate knowledge. Care improvement targets 3. 4. 5. 6. 7. Clinical decision support Patient-centered care Community links Care continuity Optimized operations Supportive policy environment 8. Financial incentives. 9. Performance transparency 10. Broad leadership Our National Quality Strategy Better Health for the Population Better Care for Individuals Lower Cost Through Improvement 44 Health IT: Helping to Drive the 3-Part Aim Better healthcare Improving patients’ experience of care within the Institute of Medicine’s 6 domains of quality: Safety, Effectiveness, PatientCenteredness, Timeliness, Efficiency, and Equity. Better health Keeping patients well so they can do what they want to do. Increasing the overall health of populations: address behavioral risk factors; focus on preventive care. Reduced costs Lowering the total cost of care while improving quality, resulting in reduced monthly expenditures for Medicare, Medicaid, and CHIP beneficiaries. $ Health Information Technology 45 Meaningful Use as a Building Block Transform health care Improved population health Access to information Enhanced access and continuity Data utilized to improve delivery and outcomes Data utilized to improve delivery and outcomes Patient self management Patient engaged, community resources Care coordination Care coordination Patient centered care coordination Patient informed Evidenced based medicine Team based care, case management Basic EHR functionality, structured data Structured data utilized Registries for disease management Registries to manage patient populations Privacy & security protections Privacy & security protections Privacy & security protections Privacy & security protections Stage 2 MU PCMH 3-Part Aim ACO’s “Stage 3 MU” Utilize technology Stage 1 MU 46 Meaningful Use Is Just the Beginning: Other Three Part Aim Programs • A recent analysis identified that the national network of RECs are currently working on over 190 different programs to help providers meet the Three Part Aim * Based on information from 53 of 62 RECs. Some are working on several different Three-Part Aim Programs 47 . 48 THE FUTURE IS NOW. THIS IS OUR TIME. Thanks! judy.murphy@hhs.gov 49