ppt - GRADE working group
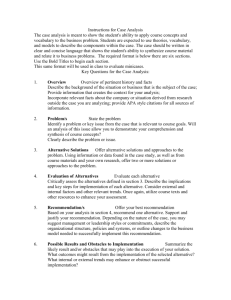
advertisement

Holger Schünemann Professor of Clinical Epidemiology, Biostatistics and Medicine McMaster University, Hamilton, Canada Italian NCI „Regina Elena“, Rome, Italy Principles guideline development and the GRADE system Content Describe the grade of recommendation and what each category means: strong/weak and optional language How the quality of evidence can be upgraded/down-graded What happens when you’re recommending something not be done? Maybe provide some ID-type examples if possible - I’m attaching our clinical questions that may be used as examples? Provide a quick tutorial of GRADEPro Questions The GRADE approach Clear separation of 2 issues: 1) 4 categories of quality of evidence: very low, low, moderate, or high quality? methodological considerations likelihood of systematic deviation from truth by outcome 2) Recommendation: 2 grades – weak/conditional or strong (for or against)? Quality of evidence only one factor Influenced by magnitude of effect(s) – balance of benefits and harms, values and preferences, cost *www.GradeWorkingGroup.org Content Describe the grade of recommendation and what each category means: strong/weak and optional language How the quality of evidence can be upgraded/down-graded What happens when you’re recommending something not be done? Maybe provide some ID-type examples if possible - I’m attaching our clinical questions that may be used as examples? Provide a quick tutorial of GRADEPro Questions Implications of a strong recommendation Patients: Most people in this situation would want the recommended course of action and only a small proportion would not Clinicians: Most patients should receive the recommended course of action Policy makers: The recommendation can be adapted as a policy in most situations Implications of a weak recommendation Patients: The majority of people in this situation would want the recommended course of action, but many would not Clinicians: Be prepared to help patients to make a decision that is consistent with their own values/decision aids and shared decision making Policy makers: There is a need for substantial debate and involvement of stakeholders Content Describe the grade of recommendation and what each category means: strong/weak and optional language How the quality of evidence can be upgraded/down-graded What happens when you’re recommending something not be done? Maybe provide some ID-type examples if possible - I’m attaching our clinical questions that may be used as examples? Provide a quick tutorial of GRADEPro Questions Answer Same type of interpretation Content Describe the grade of recommendation and what each category means: strong/weak and optional language How the quality of evidence can be upgraded/down-graded What happens when you’re recommending something not be done? Maybe provide some ID-type examples if possible - I’m attaching our clinical questions that may be used as examples? Provide a quick tutorial of GRADEPro Questions Determinants of quality - For body of evidence - RCTs start high observational studies start low 5 factors that can lower quality 1. 2. 3. 4. 5. limitations of detailed design and execution inconsistency Indirectness/applicability publication bias Imprecision 3 factors can increase quality 1. 2. 3. large magnitude of effect all plausible confounding may be working to reduce the demonstrated effect or increase the effect if no effect was observed dose-response gradient Assessing the quality of evidence 11 1. Design and Execution limitations lack of concealment intention to treat principle violated inadequate blinding loss to follow-up early stopping for benefit selective outcome reporting Example: RCT suggests that danaparoid sodium is of benefit in treating HIT complicated by thrombosis Key outcome: clinicians’ assessment of when the thromboembolism had resolved Not blinded – subjective judgement 2. Inconsistency of results (Heterogeneity) if inconsistency, look for explanation patients, intervention, outcome, methods unexplained inconsistency downgrade quality Bleeding in thrombosis-prophylaxed hospitalized patients seven RCTs 4 lower, 3 higher risk Example: Bleeding in the hospital Dentali et al. Ann Int Med, 2007 Judgment variation in size of effect overlap in confidence intervals statistical significance of heterogeneity I2 Heparin or vitamin K antagonists for survival in patients with cancer Akl E, Barba M, Rohilla S, Terrenato I, Sperati F, Schünemann HJ. “Anticoagulation for the long term treatment of venous thromboembolism in patients with cancer”. Cochrane Database Syst Rev. 2008 Apr 16;(2):CD006650. Non-steroidal drug use and risk of pancreatic cancer Capurso G, Schünemann HJ, Terrenato I, Moretti A, Koch M, Muti P, Capurso L, Delle Fave G. Meta-analysis: the use of non-steroidal anti-inflammatory drugs and pancreatic cancer risk for different exposure categories. Aliment Pharmacol Ther. 2007 Oct 15;26(8):1089-99. 3. Directness of Evidence differences in populations/patients (mild versus severe COPD, older, sicker or more co-morbidity) interventions (all inhaled steroids, new vs. old) outcomes (important vs. surrogate; long-term healthrelated quality of life, short –term functional capacity, laboratory exercise, spirometry) indirect comparisons interested in A versus B have A versus C and B versus C formoterol versus salmeterol versus tiotropium Directness interested in A versus B available data A vs C, B vs C Alendronate Risedronate Placebo 4. Publication Bias & Imprecision Publication bias number of small studies I.V. Mg in acute myocardial infarction ISIS-4 Lancet 1995 Meta-analysis Yusuf S.Circulation 1993 Publication bias Egger M, Smith DS. BMJ 1995;310:752-54 21 Funnel plot Standard Error 0 Symmetrical: No publication bias 1 2 3 0.1 0.3 0.6 1 3 10 Odds ratio Egger M, Cochrane Colloquium Lyon 2001 22 Funnel plot Standard Error 0 Asymmetrical: Publication bias? 1 2 3 0.1 0.3 0.6 1 3 10 Odds ratio Egger M, Cochrane Colloquium Lyon 2001 23 I.V. Mg in acute myocardial infarction ISIS-4 Lancet 1995 Meta-analysis Yusuf S.Circulation 1993 Publication bias Egger M, Smith DS. BMJ 1995;310:752-54 24 Metaanalysis confirme d by megatrials Egger M, Smith DS. BMJ 1995;310:752-54 25 Publication bias (File Drawer Problem) Faster and multiple publication of “positive” trials Fewer and slower publication of “negative” trials 26 5. Imprecision small sample size small number of events wide confidence intervals uncertainty about magnitude of effect how to decide if CI too wide? grade down one level? grade down two levels? extent to which confidence in estimate of effect adequate to support decision Example: Bleeding in the hospital Dentali et al. Ann Int Med, 2007 Offer all effective treatments? atrial fib at risk of stroke warfarin increases serious gi bleeding 3% per year 1,000 patients 1 less stroke 30 more bleeds for each stroke prevented 1,000 patients 100 less strokes 3 strokes prevented for each bleed where is your threshold? how many strokes in 100 with 3% bleeding? 1.0% 0 1.0% 0 1.0% 0 1.0% 0 What can raise quality? 1. large magnitude can upgrade (RRR 50%) very large two levels (RRR 80%) common criteria everyone used to do badly almost everyone does well oral anticoagulation for mechanical heart valves insulin for diabetic ketoacidosis hip replacement for severe osteoarthritis 2. dose response relation (higher INR – increased bleeding) 3. all plausible confounding may be working to reduce the demonstrated effect or increase the effect if no effect was observed All plausible confounding would result in an underestimate of the treatment effect Higher death rates in private for-profit versus private not-for-profit hospitals patients in the not-for-profit hospitals likely sicker than those in the for-profit hospitals for-profit hospitals are likely to admit a larger proportion of well-insured patients than not-forprofit hospitals (and thus have more resources with a spill over effect) All plausible biases would result in an overestimate of effect Hypoglycaemic drug phenformin causes lactic acidosis The related agent metformin is under suspicion for the same toxicity. Large observational studies have failed to demonstrate an association Clinicians would be more alert to lactic acidosis in the presence of the agent Content Describe the grade of recommendation and what each category means: strong/weak and optional language How the quality of evidence can be upgraded/down-graded What happens when you’re recommending something not be done? Maybe provide some ID-type examples if possible - I’m attaching our clinical questions that may be used as examples? Provide a quick tutorial of GRADEPro Questions Relevant clinical question? Example from a not so common disease Clinical question: Population: Avian Flu/influenza A (H5N1) patients Intervention: Oseltamivir (or Zanamivir) Comparison: No pharmacological intervention Outcomes: Mortality, hospitalizations, resource use, adverse outcomes, antimicrobial resistance Schunemann et al. The Lancet ID, 2007 Methods – WHO Rapid Advice Guidelines for management of Avian Flu Applied findings of a recent systematic evaluation of guideline development for WHO/ACHR Group composition (including panel of 13 voting members): clinicians who treated influenza A(H5N1) patients infectious disease experts basic scientists public health officers methodologists Independent scientific reviewers: Identified systematic reviews, recent RCTs, case series, animal studies related to H5N1 infection Evidence Profile Oseltamivir for treatment of H5N1 infection: Summary of findings Quality assessment No of studies (Ref) Design Limitations Consistency No of patients Other considerations Directness Effect Oseltamivir Placebo Relative (95% CI) Absolute (95% CI) Quality Importance Healthy adults: Mortality 0 Hospitalisation (Hospitalisations from influenza – influenza cases only) - - - - - 5 (TJ 06) Imprecise or sparse data (-1) - - OR 0.22 (0.02 to 2.16) - Very low 6 - - - - - - 7 2/982 (0.2%) 9/662 (1.4%) RR 0.149 (0.03 to 0.69) - Very low 8 Randomised trial No limitations One trial only - Major uncertainty (-2)1 9 Duration of hospitalization 0 LRTI (Pneumonia - influenza cases only) 5 (TJ 06) Randomised trial - No limitations One trial only - Major uncertainty (-2)1 Imprecise or sparse data (-1)2 Duration of disease (Time to alleviation of symptoms/median time to resolution of symptoms – influenza cases only) Randomised 53 No limitations4 Important trials inconsistency (TJ 06) (DT 03) (-1)5 Viral shedding (Mean nasal titre of excreted virus at 24h) 26 (TJ 06) Randomised trials No limitations -7 Major uncertainty (-2)1 - - - HR 1.303 (1.13 to 1.50) - Very low 5 Major uncertainty (-2)1 None - - - WMD -0.738 (-0.99 to -0.47) Low 4 - - - - - - 4 - - - - - - 7 - - - - - - 7 Imprecise or sparse data (-1)14 - - OR range15 (0.56 to 1.80) - Low - - - - - - Outbreak control 0 Resistance - - - - 0 Serious adverse effects (Mention of significant or serious adverse effects) 09 Minor adverse effects 311 (TJ 06) 10 - - - (number and seriousness of adverse effects) Randomised trials No limitations -12 Some uncertainty (-1)13 Cost of drugs 0 - - - - 4 Oseltamivir for Avian Flu Summary of findings: No clinical trial of oseltamivir for treatment of H5N1 patients. 4 systematic reviews and health technology assessments (HTA) reporting on 5 studies of oseltamivir in seasonal influenza. Hospitalization: OR 0.22 (0.02 – 2.16) Pneumonia: OR 0.15 (0.03 - 0.69) 3 published case series. Many in vitro and animal studies. No alternative that is more promising at present. Cost: ~ 40$ per treatment course Schunemann et al. Lancet ID, 2007 & PLOS Medicine 2007 Determinants of the strength of recommendation Factors that can strengthen a Comment recommendation Quality of the evidence The higher the quality of evidence, the more likely is a strong recommendation. Balance between desirable The larger the difference between the and undesirable effects desirable and undesirable consequences, the more likely a strong recommendation warranted. The smaller the net benefit and the lower certainty for that benefit, the more likely weak recommendation warranted. Values and preferences The greater the variability in values and preferences, or uncertainty in values and preferences, the more likely weak recommendation warranted. Costs (resource allocation) The higher the costs of an intervention – that is, the more resources consumed – the less likely is a strong recommendation warranted Example: Oseltamivir for Avian Flu Recommendation: In patients with confirmed or strongly suspected infection with avian influenza A (H5N1) virus, clinicians should administer oseltamivir treatment as soon as possible (????? recommendation, very low quality evidence). Schunemann et al. The Lancet ID, 2007 Example: Oseltamivir for Avian Flu Recommendation: In patients with confirmed or strongly suspected infection with avian influenza A (H5N1) virus, clinicians should administer oseltamivir treatment as soon as possible (strong recommendation, very low quality evidence). Values and Preferences Remarks: This recommendation places a high value on the prevention of death in an illness with a high case fatality. It places relatively low values on adverse reactions, the development of resistance and costs of treatment. Schunemann et al. The Lancet ID, 2007 Other explanations Remarks: Despite the lack of controlled treatment data for H5N1, this is a strong recommendation, in part, because there is a lack of known effective alternative pharmacological interventions at this time. The panel voted on whether this recommendation should be strong or weak and there was one abstention and one dissenting vote. Strength of recommendation “The strength of a recommendation reflects the extent to which we can, across the range of patients for whom the recommendations are intended, be confident that desirable effects of a management strategy outweigh undesirable effects.” Strong or weak/conditional Quality of evidence & strength of recommendation Linked but no automatism Other factors beyond the quality of evidence influence our confidence that adherence to a recommendation causes more benefit than harm Systems/approaches failed to make this explicit GRADE separates quality of evidence from strength of recommendation Content Describe the grade of recommendation and what each category means: strong/weak and optional language How the quality of evidence can be upgraded/down-graded What happens when you’re recommending something not be done? Maybe provide some ID-type examples if possible - I’m attaching our clinical questions that may be used as examples? Provide a quick tutorial of GRADEPro Questions Creating a new GRADEpro file Profile groups Profiles Profiles: Questions Importing a RevMan 5 file of a systematic review Imported data from RevMan 5 file: • outcomes • meta-analyses results • bibliographic information Managing outcomes to include a maximum of 7 Entering/editing information for dichotomous outcomes Entering/editing information to grade the quality of the evidence Content Describe the grade of recommendation and what each category means: strong/weak and optional language How the quality of evidence can be upgraded/down-graded What happens when you’re recommending something not be done? Maybe provide some ID-type examples if possible - I’m attaching our clinical questions that may be used as examples? Provide a quick tutorial of GRADEPro Questions Example: Oseltamivir for Avian Flu Recommendation: In patients with confirmed or strongly suspected infection with avian influenza A (H5N1) virus, clinicians should administer oseltamivir treatment as soon as possible (strong recommendation, very low quality evidence). Values and Preferences This recommendation places a high value on the prevention of death in an illness with a high case fatality. It places relatively low values on adverse reactions, the development of resistance and costs of treatment. Remarks Despite the lack of controlled treatment data for H5N1, this is a strong recommendation, in part, because there is a lack of known effective alternative pharmacological interventions at this time. Schunemann et al. The Lancet ID, 2007 Confidence in evidence There always is evidence “When there is a question there is evidence” Research evidence alone is never sufficient to make a clinical decision Better research greater confidence in the evidence and decisions Factors leading to bias? Can you explain them? Question Baseline Method Random? Allocation Sequence gen. Selection bias? A Performance Intervention bias? B Allocation concealment No interv. Blinding/Masking Attrition bias? Follow up Follow up Intention-to-treat analysis Detection bias? Outcome Outcome Blinding/Masking P-values and confidence intervals important? CONSENSUS ALWAYS REQUIRED 77 Limitations of existing systems confuse quality of evidence with strength of recommendations lack well-articulated conceptual framework criteria not comprehensive or transparent GRADE unique breadth, intensity of development process wide endorsement and use conceptual framework comprehensive, transparent criteria Grades of Recommendation Assessment, Development and Evaluation GRADE WORKING GROUP *Grade Working Group. CMAJ 2003, BMJ 2004, BMC 2004, BMC 2005, AJRCCM 2006, BMJ 2008 GRADE Working Group David Atkins, chief medical officera a) Agency for Healthcare Research and Quality, USA Dana Best, assistant professorb b) Children's National Medical Center, USA Martin Eccles, professord c) Centers for Disease Control and Prevention, USA Francoise Cluzeau, lecturerx d) University of Newcastle upon Tyne, UK Yngve Falck-Ytter, Signe associate directore e) German Cochrane Centre, Germany Flottorp, researcherf Gordon H f) Norwegian Centre for Health Services, Norway Guyatt, professorg Robin T Harbour, quality g) McMaster University, Canada and information director h Margaret C Haugh, methodologisti David Henry, i) Fédération Nationale des Centres de Lutte Contre le Cancer, France professorj Suzanne Hill, senior j) University of Newcastle, Australia lecturerj Roman Jaeschke, clinical h) Scottish Intercollegiate Guidelines Network, UK k) McMaster University, Canada professork l) National Institute for Clinical Excellence, UK Regina Kunx, Associate Professor m) Università di Modena e Reggio Emilia, Italy Gillian Leng, guidelines programme directorl n) Centro per la Valutazione della Efficacia della Assistenza Sanitaria, Italy Alessandro Liberati, professorm o) Australasian Cochrane Centre, Australia Nicola Magrini, directorn p) Polish Institute for Evidence Based Medicine, Poland James Mason, professord q) The Cancer Council, Australia Philippa Middleton, honorary research Jacek Mrukowicz, executive Dianne O’Connell, senior fellowo directorp epidemiologistq Andrew D Oxman, directorf Bob Phillips, associate fellowr r) Centre for Evidence-based Medicine, UK s) National Cancer Institute, Italy t) World Health Organisation, Switzerland u) Finnish Medical Society Duodecim, Finland v) Duke University Medical Center, USA Holger J Schünemann, professorg,s w) Centers for Disease Control and Prevention, USA Tessa Tan-Torres Edejer, medical officert x) University of London, UK David Tovey, Editory Y) BMJ Clinical Evidence, UK Jane Thomas, Lecturer, UK Helena Varonen, associate editoru Gunn E Vist, researcherf John W Williams Jr, professorv Stephanie Zaza, project directorw GRADE Uptake World Health Organization National Institute Clinical Excellence (NICE) Allergic Rhinitis in Asthma Guidelines (ARIA) American Thoracic Society British Medical Journal Infectious Disease Society of America American College of Chest Physicians UpToDate American College of Physicians Cochrane Collaboration Infectious Disease Society of America European Society of Thoracic Surgeons Clinical Evidence Agency for Health Care Research and Quality (AHRQ) Over 20 major organizations The GRADE approach Clear separation of 2 issues: 1) 4 categories of quality of evidence: very low, low, moderate, or high quality? methodological quality of evidence likelihood of systematic deviation from truth by outcome 2) Recommendation: 2 grades – weak/conditional or strong (for or against)? Quality of evidence only one factor Influenced by magnitude of effect(s) – balance of benefits and harms, values and preferences, cost *www.GradeWorkingGroup.org GRADE Quality of Evidence “Extend of confidence on how adequate the estimate of effect is to support decision” high: considerable confidence in estimate of effect. moderate: further research likely to have impact on confidence in estimate, may change estimate. low: further research is very likely to impact on confidence, likely to change the estimate. very low: any estimate of effect is very uncertain Developing recommendations Conclusion clinicians, policy makers need summaries that separate: quality of evidence strength of recommendations explicit rules transparent, informative GRADE four categories of quality of evidence two grades for strength of recommendations transparent, systematic by and across outcomes applicable to diagnosis wide adoption Consistency of results consistency of results if inconsistency, look for explanation patients, intervention, outcome, methods unexplained inconsistency downgrade quality oxygen for day-to-day dyspnea in COPD with exercise hypoxemia five cross-over RCTs oxygen versus placebo 4 no benefit, 1 substantial benefit Evidence profiles Directness of Evidence indirect comparisons interested in A versus B have A versus C and B versus C formoterol versus salmeterol versus tiotropium Acetylcysteine alone for Pulmonary Fibrosis (all that is available is Acetylcysteine + Prednisone + Azathioprine vs. Prednisone + Azathioprine) Directness of Evidence differences in patients (inhalers for mild versus moderate to severe COPD) interventions (all inhaled steroids versus those used in clinical trials – drug class effect) outcomes (long-term health-related quality of life, short – term functional capacity, laboratory exercise, spirometry) Reporting Bias & Imprecision reporting bias reporting of studies publication bias number of small studies reporting of outcomes small sample size small number of events wide confidence intervals uncertainty about magnitude of effect Differences in exercise capacity in short-term randomized trials of oxygen in COPD patients. What can raise quality? large magnitude can upgrade (RRR 50%) very large two levels (RRR 80%) common criteria everyone used to do badly almost everyone does well Insulin in diabetic ketoacidosis dose response relation (smoking - cancer) The clinical scenario A 68 year old male long-term patient of yours. He suffers from COPD but is unable to stop smoking after over 30 years of tobacco use. He has been taking beta-carotene supplements for several months because someone in the “healthy food” store recommended it to prevent cancer. He wants to know whether this will prevent him from getting cancer and whether he should use beta-carotene. The clinical question Population: Intervention: Comparison: Outcomes: In patients with COPD does beta-carotene suppl compared to no suppl. reduce the risk of lung cancer? Where do you look for an answer? Clinical Practice Guidelines Systematically developed statements to assist practitioner and patient decisions about appropriate health care for specific clinical circumstances Institute of Medicine, 1992 Determinants of quality RCTs start high observational studies start low 5 Factors that lower quality (bias) 3 Factors that increase quality (bias is unlikely to explain observed effect) Final quality by outcome: High Moderate Low Very low Design and Execution limitations lack of concealment intention to treat principle violated inadequate blinding loss to follow-up early stopping for benefit 13 RCTs bacterial extract (immunomodulation) for preventing exacerbation unclear concealment of randomization questionable intention to treat inadequate attention to loss to follow-up Consistency of results consistency of results if inconsistency, look for explanation patients, intervention, outcome, methods unexplained inconsistency downgrade quality oxygen for day-to-day dyspnea in COPD with exercise hypoxemia five cross-over RCTs oxygen versus placebo 4 no benefit, 1 substantial benefit Directness of Evidence indirect comparisons interested in A versus B have A versus C and B versus C formoterol versus salmeterol versus tiotropium differences in patients (mild versus severe COPD) interventions (all inhaled steroids) outcomes (long-term health-related quality of life, short – term functional capacity, laboratory exercise, spirometry) How should recommendations be formulated and presented? Few written standards exist For strong recommendations, the GRADE working group has suggested adopting terminology such as, “We recommend…” or “Clinicians should…”. For weak recommendation, they should use less definitive wording, “We suggest…” or “Clinicians might…”. Clinicians and patients want to know! 1) UpToDate® Users 2) Mini Medical School attendees*: • Participants preferred to know about the uncertainty relating to outcomes of a treatment or a test • more interested in knowing about uncertainty relating to benefits than harms (96% vs. 90%; P<0.001). • strong preference to be informed about the quality of evidence that supports a recommendation. *Akl et al. J Clin Epi, 2007, in press GRADE Quality of Evidence Extent to which confidence in estimate of effect adequate to support decision high: considerable confidence in estimate of effect. moderate: further research likely to have impact on confidence in estimate, may change estimate. low: further research is very likely to impact on confidence, likely to change the estimate. very low: any estimate of effect is very uncertain There always is evidence The better the research and the evidence, the more confident the decision Evidence alone is never sufficient to make a clinical decision Do evidence based guidelines make a difference? Non-rigorous guidelines: • Create noise & bias • Make more aggressive recommendations • Can harm patients and impair research efforts • Can reduce credibility of professional societies Evidence-based clinical practice guidelines can: • reduce delivery of inappropriate care • support introduction of new knowledge into clinical practice Grimshaw et al (1992); Woolf et al (1999); Fretheim et al (2002)