Chapter 6: Osseous Tissue and Bone Structure
advertisement

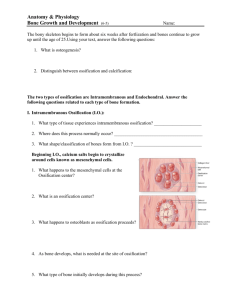
Bone Development • Human bones grow until about age 25 • Osteogenesis: – bone formation • Ossification: – the process of replacing other tissues with bone Calcification • The process of depositing calcium salts • Occurs during bone ossification and in other tissues Ossification • The 2 main forms of ossification are: – intramembranous ossification – endochondral ossification Intramembranous Ossification: Step 1 • Mesenchymal cells aggregate: – differentiate into osteoblasts – begin ossification at the ossification center – develop projections called spicules Intramembranous Ossification: Step 2 Figure 6–11 (Step 2) Intramembranous Ossification: Step 2 • Blood vessels grow into the area: – to supply the osteoblasts • Spicules connect: – trapping blood vessels inside bone Intramembranous Ossification: Step 3 Figure 6–11 (Step 3) Intramembranous Ossification: Step 3 • Spongy bone develops and is remodeled into: – osteons of compact bone – periosteum – or marrow cavities Endochondral Ossification • Ossifies bones that originate as hyaline cartilage • Most bones originate as hyaline cartilage Endochondral Ossification • Growth and ossification of long bones occurs in 6 steps Endochondral Ossification: Step 1 • Chondrocytes in the center of hyaline cartilage: – enlarge – form struts and calcify – die, leaving cavities in cartilage Figure 6–9 (Step 1) Endochondral Ossification: Step 2 Figure 6–9 (Step 2) Endochondral Ossification: Step 2 • Blood vessels grow around the edges of the cartilage • Cells in the perichondrium change to osteoblasts: – producing a layer of superficial bone around the shaft which will continue to grow and become compact bone (appositional growth) Endochondral Ossification: Step 3 • Blood vessels enter the cartilage: – bringing fibroblasts that become osteoblasts – spongy bone develops at the primary ossification center Figure 6–9 (Step 3) Endochondral Ossification: Step 4 • Remodeling creates a marrow cavity: – bone replaces cartilage at the metaphyses Figure 6–9 (Step 4) Endochondral Ossification: Step 5 • Capillaries and osteoblasts enter the epiphyses: – creating secondary ossification centers Figure 6–9 (Step 5) Endochondral Ossification: Step 6 Figure 6–9 (Step 6) Endochondral Ossification: Step 6 • Epiphyses fill with spongy bone: – cartilage within the joint cavity is articulation cartilage – cartilage at the metaphysis is epiphyseal cartilage Endochondral Ossification • Appositional growth: – compact bone thickens and strengthens long bone with layers of circumferential lamellae PLAY Endochondral Ossification Figure 6–9 (Step 2) What are the characteristics of adult bones? Epiphyseal Lines Figure 6–10 Epiphyseal Lines • When long bone stops growing, after puberty: – epiphyseal cartilage disappears – is visible on X-rays as an epiphyseal line How does the skeletal system remodel and maintain homeostasis, and what are the effects of nutrition, hormones, exercise, and aging on bone? Remodeling • The adult skeleton: – maintains itself – replaces mineral reserves • Remodeling: – recycles and renews bone matrix – involves osteocytes, osteoblasts, and osteoclasts KEY CONCEPTS • Bone continually remodels, recycles, and replaces • Turnover rate varies • If deposition is greater than removal, bones get stronger • If removal is faster than replacement, bones get weaker Bone Degeneration • Bone degenerates quickly • Up to 1/3 of bone mass can be lost in a few weeks of inactivity KEY CONCEPTS • What you don’t use, you lose • Stresses applied to bones during physical activity are essential to maintain bone strength and mass Effects of Hormones and Nutrition on Bone • Normal bone growth and maintenance requires nutritional and hormonal factors Calcitriol • The hormone calcitriol: – is made in the kidneys – helps absorb calcium and phosphorus from digestive tract – synthesis requires vitamin D3 (cholecalciferol) Vitamins • Vitamin C is required for collagen synthesis, and stimulates osteoblast differentiation • Vitamin A stimulates osteoblast activity • Vitamins K and B12 help synthesize bone proteins Other Hormones • Growth hormone and thyroxine stimulate bone growth • Estrogens and androgens stimulate osteoblasts • Calcitonin and parathyroid hormone regulate calcium and phosphate levels Calcium Regulation • Calcium ions in body fluids: – must be closely regulated • Homeostasis is maintained: – by calcitonin and parathyroid hormone – which control storage, absorption, and excretion Calcitonin and Parathyroid Hormone Control • Bones: – where calcium is stored • Digestive tract: – where calcium is absorbed • Kidneys: – where calcium is excreted Parathyroid Hormone (PTH) • Produced by parathyroid glands in neck • Increases calcium ion levels by: – stimulating osteoclasts – increasing intestinal absorption of calcium – decreases calcium excretion at kidneys Calcitonin • Secreted by C cells (parafollicular cells) in thyroid • Decreases calcium ion levels by: – inhibiting osteoclast activity – increasing calcium excretion at kidneys Fractures • Fractures: – cracks or breaks in bones – caused by physical stress • Fractures are repaired in 4 steps Fracture Repair: Step 1 Figure 6–15 (Step 1) Fracture Repair: Step 1 • Bleeding: – produces a clot (fracture hematoma) – establishes a fibrous network • Bone cells in the area die Fracture Repair: Step 2 Figure 6–15 (Step 2) Fracture Repair: Step 2 • Cells of the endosteum and periosteum: – Divide and migrate into fracture zone • Calluses stabilize the break: – external callus of cartilage and bone surrounds break – internal callus develops in marrow cavity Fracture Repair: Step 3 Figure 6–15 (Step 3) Fracture Repair: Step 3 • Osteoblasts: – replace central cartilage of external callus – with spongy bone Fracture Repair: Step 4 Figure 6–15 (Step 4) Fracture Repair: Step 4 • Osteoblasts and osteocytes remodel the fracture for up to a year: – reducing bone calluses PLAY Steps in the Repair of a Fracture The Major Types of Fractures • Pott’s fracture Figure 6–16 (1 of 9) The Major Types of Fractures • Comminuted fractures Figure 6–16 (2 of 9) The Major Types of Fractures • Transverse fractures Figure 6–16 (3 of 9) The Major Types of Fractures • Spiral fractures Figure 6–16 (4 of 9) The Major Types of Fractures • Displaced fractures Figure 6–16 (5 of 9) The Major Types of Fractures • Colles’ fracture Figure 6–16 (6 of 9) The Major Types of Fractures • Greenstick fracture Figure 6–16 (7 of 9) The Major Types of Fractures • Epiphyseal fractures Figure 6–16 (8 of 9) The Major Types of Fractures • Compression fractures Figure 6–16 (9 of 9) What are the effects of aging on the skeletal system? Age and Bones • Bones become thinner and weaker with age • Osteopenia begins between ages 30 and 40 • Women lose 8% of bone mass per decade, men 3% Effects of Bone Loss • The epiphyses, vertebrae, and jaws are most affected: – resulting in fragile limbs – reduction in height – tooth loss Osteoporosis • Severe bone loss • Affects normal function • Over age 45, occurs in: – 29% of women – 18% of men Hormones and Bone Loss • Estrogens and androgens help maintain bone mass • Bone loss in women accelerates after menopause Cancer and Bone Loss • Cancerous tissues release osteoclastactivating factor: – that stimulates osteoclasts – and produces severe osteoporosis