Renal Disorders
advertisement
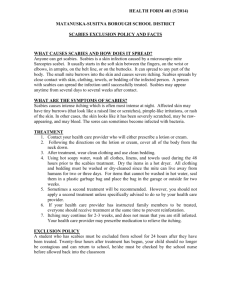
Impetigo Vesicles or pustule surrounded by edema and redness Impetigo Begins as a reddish macular rash, commonly seen on face/extremities Progresses to papular and vesicular rash that oozes and forms a moist, honey colored crust. Pruritis of skin Common in 2-5 year age group Impetigo Impetigo became infected group a hemolytic strep infection of skin. Incubation period is 2-5 days after contact Easily spread merely by touching another part of skin after scratching infected area. Therpeutic Management Apply warm, moist soaks to soften lesions, remove crusts Apply Bactroban TID to cleaned lesions Cephalexin (keflex) for 10 days Teach good handwashing and hygiene to prevent spread, keep fingernails short Impetigo Be alert for signs of acute glomerulonephritis, If the impetigo was caused by beta-hemolytic streptococci Therapeutic Interventions Goal - prevent scarring and promote positive self-image. Individualize treatment to gender, age, and severity of infection. It takes 4-6 weeks to begin to see improvement, with optimal results in 3-5 months. What is the major nursing implication here? Oral Candidiasis Fungal or yeast infection also known as Thrush Oral Candidiasis - causes Passing through an infected birth canal Child who is on immunosuppressant's Exposure to mothers infected breasts Unclean bottles and pacifiers Oral Candidiasis - Manifestations White curdlike plaques on tongue, gums, and buccal mucosa How to differentiate from milk Thrush is very difficult to remove and bleeding of the area when plaques are removed. Oral Candidiasis – Treatment Oral Nystatin suspension Swish and swallow Rub medication on the area with gloved hands Apply after meals Oral fluconazole administed 1/day orally Clean pacifiers, bottles, etc. Provide cool liquids for the older child Tinea / Ringworm Caused by a group of fungi called dermatophytes Clinical Manifestations fungal infection of the stratum corneum, nails and hair(the base of hair shaft causing hair to break off-rarely permanent. Scaly, circumscribed patches to patchy, gray scaling areas of alopecia. Pruritic itching Generally asymptomatic, but severe, deep inflammatory reaction may appear as boggy, encrusted lesions (kerions) Tinea capitis Tinea corpus Tinea cruis Tinea pedis or athletes foot http://www.ecureme.com/quicksearch_reference.asp Drug Therapy: Antifungal Medication: Oral griseofulvin Give with fatty foods to aid in absorption Treatment is for 6- 8 weeks Can return to day care when lesions are dry Avoid sun exposure Nizoral, Diflucan, Lamisil – used only in older children because of risk of hepatoxicity Teaching transmitted by clothing, bedding, combs and animals (cats) may take 1-3 months to heal completely, even with treatment Child doesn't return to school until lesions dry. See Home Care for Child with Tinea infection on page 1347. Pediculosis Lice infestation Pediculosis Capitis (lice or cooties!) a parasitic skin disorder caused by lice the lice lay eggs which look like white flecks, attached firmly to base of the hair shaft, causing intense pruritus Lice assessment Close examination of scalp reveals (nits) firmly attached to hair shafts. Easily transmitted by clothing towels, combs, close contact, unrelated to hygiene. Goals of Care Kill the active lice Remove Nits Prevent Spread Treatment and Nursing Care pediculicide, permethrin (NIX) crème rinse Applied to washed and towel dried hair. Massage into the hair and scalp one section at a time. **Wet hair dilutes the product and may contribute to treatment failure. Leave in place for 10 minutes and rinse Towel dry Comb hair with a fine-tooth comb to remove any remaining nits. Repeat in 1-2 weeks Treatment and Nursing Care Ovide Approved for treatment in older children only. Must have prolong contact (8-10 hrs) to be effective Lindane (Kwell) is no longer approved for treatment Scabies Mite infestation Scabies Sarcoptes scabei mite. Females are 0.3 to 0.4 mm long and 0.25 to 0.35 mm wide. Males are slightly more than half that size. a parasitic skin disorder (stratum corneum- not living tissue) caused by a female mite. The mite burrows into the skin depositing eggs and fecal material; between fingers, toes, palms, axillae pruritic & grayish-brown, thread-like lesion Scabies Scabies is spread from person to person mainly by prolonged direct skin-to-skin contact, such as touching a person who has scabies. In rare cases, scabies can spread by contact with clothes, towels, bedding, and other personal items that were recently in contact with an infected person. The mites live on human blood and need the warmth of the human body to survive. Away from the body, they die within 48 hours. Scabies Scabies between thumb and index finger On foot Therapeutic Interventions transmitted by clothing, towels, close contact Diagnosis confirmed by demonstration from skin scrapings. treatment: application of scabicide cream which is left on for a specific number of hours (4 to 14)to kill mite rash and itch will continue until stratum corneum is replace (2-3 weeks) Care: Fresh laundered linen and underclothing should be used. Contacts should be reduced until treatment is completed. DERMATITIS Inflammation of the skin that occurs in response to contact with an allergen or irritant Dermatitis Common Irritants Soap, fabric softeners, lotions, urine and stool Common Allergens Poison ivy, Poison oak Lanolin Latex, rubber Nickel Fragrances Dermatitis – Signs and Symptoms Erythema Edema Pururitus Vesicles or bullae that rupture, ooze and crust Dermatitis - Treatment Medications Application of a corticosteroid topical agent – remind to continue use for 2-3 weeks after signs of healing Application of protective barrier ointments Oatmeal baths, Cool compresses Antihistamines given for sedative effect Treatment of Dermatitis Eczema Chronic superficial skin disorder characterized by intense pruritis Eczema Immune disorder of the skin Influenced by genetic predisposition and external triggers Tends to occur in children with hereditary allergic tendencies Eczema – Signs and Symptoms Erythematous patches with vesicles Pruritus Exudate and crusts Drying and scaling Lichenification (thickening of the skin) Goal of Treatment Hydrate the Skin Reduce the amount of allergen exposure Relieve Pruritis Acne Inflammatory disease of the skin involving the sebaceous glands and hair follicles. Acne- Three Main Types Comedomalnoninflammatory follicular plug ACNE Papulopustularpapules and pustules Cysticnodules and cysts Precipitating factors Heredity Hormonal influences Emotional stress Heat and Humidity Patient Teaching Do not pick! this increases the bacterial count on the surface of the skin and opens lesions to infection which worsens scarring. Remind patients that the treatment will not show improvement until about 4-6 weeks but they must consistently follow the regime set up by the physician. Medical Therapy for Acne Topical: Benzoyl Peroxide, Tretinoin (RetinA), tetracycline and erythromycin. Topical agents are preferred treatment to systemic antibiotics, however increases in antibiotic resistant bacteria may require use of systemic antibiotics. Oral: Tetracycline, minocycline, erythromycin and clindamycin- used for severe inflammatory acne or resistant to topical medications. Estrogen may also work for female patients. Isotretinoin (Accutane)- side effects include cataracts, dry skin, pruritius, conjunctivitis, nosebleeds and depression. Also a teratogen! Acne – Nursing Care THE END