Principles and Definitions - University of Evansville Faculty Web sites
Antibiotics: Protein Synthesis,
Nucleic Acid Synthesis and
Metabolism
Principles and Definitions
• Selectivity
– Selectivty 8 toxicity
9
• Therapeutic index
– Toxic dose/ Effective dose
• Categories of antibiotics
– Bactericidal
• Usually antibiotic of choice
– Bacteriostatic
• Duration of treatment sufficient for host defenses
Principles and Definitions
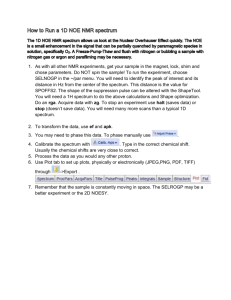
• Antibiotic susceptibility testing (in vitro)
– Minimum inhibitory concentration (MIC)
• Lowest concentration that results in inhibition of visible growth
– Minimum bactericidal concentration (MBC)
• Lowest concentration that kills 99.9% of the original inoculum
Antibiotic Susceptibility Testing
Determination of MIC
Disk Diffusion Test
Str
Tet Ery
8 4 2 1
Tetracycline (
g/ml)
MIC = 2 g/ml
0
Chl Amp
Zone Diameter Standards for Disk Diffusion Tests
Antimicrobial agent
(amt. per disk) and organism
Ampicillin (10
g)
Enerobacteriacae
Haemophilus spp.
Enterococci
Tetracycline (30
g)
R
Zone diameter (mm)
I
12-13
15-18
MS S
Approx. MIC
(
g/ml) for:
R S
Principles and Definitions
• Combination therapy
– Prevent emergence of resistant strains
– Temporary treatment until diagnosis is made
– Antibiotic synergism
• Penicillins and aminoglycosides
• CAUTION: Antibiotic antagonism
– Penicillins and bacteriostatic antibiotics
• Antibiotics vs chemotherapeutic agents vs antimicrobials
Review of Initiation of Protein Synthesis
30S
1 3
2 GTP
1 2 3 GTP
Initiation Factors mRNA
3 f-met-tRNA
Spectinomycin
P A
GDP + Pi
2
1
50S
70S
Initiation
Complex
Aminoglycosides
1
2 GTP
30S
Initiation
Complex
Review of Elongation of Protein Synthesis
Tetracycline
P A P A
P A
Fusidic Acid
Ts
Tu GTP
GTP
Tu
Ts
Tu GDP +
Ts
Pi
GDP
GDP
+
G
GTP
G GDP + Pi
G GTP
Erythromycin
P A
Chloramphenicol
Survey of Antibiotics
Protein Synthesis Inhibitors
• Mostly bacteriostatic
• Selectivity due to differences in prokaryotic and eukaryotic ribosomes
• Some toxicity - eukaryotic 70S ribosomes
Antimicrobials that Bind to the 30S
Ribosomal Subunit
Aminoglycosides
(bactericidal) streptomycin , kanamycin, gentamicin, tobramycin, amikacin, netilmicin, neomycin (topical)
• Mode of action - The aminoglycosides irreversibly bind to the 16S ribosomal RNA and freeze the 30S initiation complex (30S-mRNAtRNA) so that no further initiation can occur. They also slow down protein synthesis that has already initiated and induce misreading of the mRNA. By binding to the 16 S r-RNA the aminoglycosides increase the affinity of the A site for t-RNA regardless of the anticodon specificity. May also destabilize bacterial membranes.
• Spectrum of Activity -Many gram-negative and some gram-positive bacteria; Not useful for anaerobic (oxygen required for uptake of antibiotic) or intracellular bacteria .
• Resistance - Common
• Synergy - The aminoglycosides synergize with -lactam antibiotics.
The
-lactams inhibit cell wall synthesis and thereby increase the permeability of the aminoglycosides.
Tetracyclines
(bacteriostatic) tetracycline , minocycline and doxycycline
• Mode of action - The tetracyclines reversibly bind to the 30S ribosome and inhibit binding of aminoacyl-t-RNA to the acceptor site on the 70S ribosome.
• Spectrum of activity Broad spectrum; Useful against intracellular bacteria
• Resistance - Common
• Adverse effects - Destruction of normal intestinal flora resulting in increased secondary infections; staining and impairment of the structure of bone and teeth.
Spectinomycin
(bacteriostatic)
• Mode of action - Spectinomycin reversibly interferes with m-RNA interaction with the 30S ribosome. It is structurally similar to the aminoglycosides but does not cause misreading of mRNA.
• Spectrum of activity - Used in the treatment of penicillin-resistant
Neisseria gonorrhoeae
•
Resistance - Rare in Neisseria gonorrhoeae
Antimicrobials that Bind to the 50S
Ribosomal Subunit
Chloramphenicol, Lincomycin,
Clindamycin
(bacteriostatic)
• Mode of action - These antimicrobials bind to the 50S ribosome and inhibit peptidyl transferase activity.
• Spectrum of activity - Chloramphenicol - Broad range;
Lincomycin and clindamycin - Restricted range
• Resistance - Common
• Adverse effects - Chloramphenicol is toxic (bone marrow suppression) but is used in the treatment of bacterial meningitis.
Macrolides
(bacteriostatic) erythromycin , clarithromycin, azithromycin, spiramycin
• Mode of action - The macrolides inhibit translocation.
• Spectrum of activity - Gram-positive bacteria, Mycoplasma,
Legionella
• Resistance - Common
Antimicrobials that Interfere with
Elongation Factors
Selectivity due to differences in prokaryotic and eukaryotic elongation factors
Fusidic acid
(bacteriostatic)
• Mode of action - Fusidic acid binds to elongation factor G (EF-G) and inhibits release of EF-G from the EF-G/GDP complex.
• Spectrum of activity - Gram-positive cocci
Inhibitors of Nucleic Acid Synthesis
Inhibitors of RNA Synthesis
Selectivity due to differences between prokaryotic and eukaryotic
RNA polymerase
Rifampin, Rifamycin, Rifampicin,
Rifabutin
(bactericidal)
• Mode of action - These antimicrobials bind to DNA-dependent RNA polymerase and inhibit initiation of mRNA synthesis.
• Spectrum of activity - Wide spectrum but is used most commonly in the treatment of tuberculosis
• Resistance - Common
• Combination therapy - Since resistance is common, rifampin is usually used in combination therapy.
Inhibitors of DNA Synthesis
Selectivity due to differences between prokaryotic and eukaryotic enzymes
Quinolones
(bactericidal) nalidixic acid , ciprofloxacin , ofloxacin, norfloxacin, levofloxacin, lomefloxacin, sparfloxacin
• Mode of action - These antimicrobials bind to the A subunit of DNA gyrase (topoisomerase) and prevent supercoiling of DNA, thereby inhibiting DNA synthesis.
• Spectrum of activity - Gram-positive cocci and urinary tract infections
• Resistance - Common for nalidixic acid; developing for ciprofloxacin
Antimetabolite Antimicrobials
Inhibitors of Folic Acid Synthesis p-aminobenzoic acid + Pteridine
Sulfonamides
Pteridine synthetase
• Basis of
Selectivity
• Review of
Folic Acid
Metabolism
Dihydropteroic acid
Dihydrofolate synthetase
Dihydrofolic acid
Trimethoprim
Dihydrofolate reductase
Thymidine
Tetrahydrofolic acid
Methionine
Purines
Sulfonamides, Sulfones
(bacteriostatic)
• Mode of action - These antimicrobials are analogues of paraaminobenzoic acid and competitively inhibit formation of dihydropteroic acid.
• Spectrum of activity - Broad range activity against gram-positive and gram-negative bacteria; used primarily in urinary tract and Nocardia infections.
• Resistance - Common
• Combination therapy - The sulfonamides are used in combination with trimethoprim; this combination blocks two distinct steps in folic acid metabolism and prevents the emergence of resistant strains.
Trimethoprim, Methotrexate,
Pyrimethamine
(bacteriostatic)
• Mode of action - These antimicrobials binds to dihydrofolate reductase and inhibit formation of tetrahydrofolic acid.
• Spectrum of activity - Broad range activity against gram-positive and gram-negative bacteria; used primarily in urinary tract and Nocardia infections.
•
Resistance - Common
• Combination therapy - These antimicrobials are used in combination with the sulfonamides; this combination blocks two distinct steps in folic acid metabolism and prevents the emergence of resistant strains.
Anti-Mycobacterial Antibiotics
Para-aminosalicylic acid (PSA)
(bacteriostatic)
• Mode of action - Similar to sulfonamides
• Spectrum of activity - Specific for Mycobacterium tuberculosis
Dapsone
(bacteriostatic)
• Mode of action - Similar to sulfonamides
• Spectrum of activity - Used in treatment of leprosy ( Mycobacterium leprae )
Isoniazid (INH)
(bacteriostatic )
• Mode of action - Isoniazid inhibits synthesis of mycolic acids.
• Spectrum of activity - Used in treatment of tuberculosis
• Resistance - Has developed
Antimicrobial Drug Resistance
Principles and Definitions
• Clinical resistance
• Resistance can arise by mutation or by gene transfer ( e.g.
acquisition of a plasmid)
• Resistance provides a selective advantage
• Resistance can result from single or multiple steps
• Cross resistance vs multiple resistance
– Cross resistance -- Single mechanism-- closely related antibiotics
– Multiple resistance -- Multiple mechanisms -- unrelated antibiotics
Antimicrobial Drug Resistance
Mechanisms
• Altered permeability
– Altered influx
• Gram negative bacteria
– Altered efflux
• tetracycline
• Inactivation
– -lactamse
– Chloramphenicol acetyl transferase
Antimicrobial Drug Resistance
Mechanisms
• Altered target site
– Penicillin binding proteins (penicillins)
– RNA polymerase (rifampin)
– 30S ribosome (streptomycin)
• Replacement of a sensitive pathway
– Acquisition of a resistant enzyme
(sulfonamides, trimethoprim)