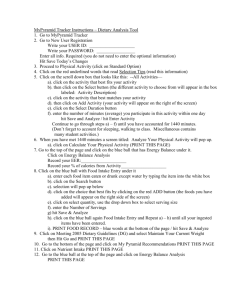
HIT FINAL EXAM REVIEW
advertisement

HIT FINAL EXAM REVIEW HI120 HIT FINAL EXAM REVIEW 1. The use of a serial numbering system does not need computer software to track the assignment of patient numbers. T/F HIT FINAL EXAM REVIEW 2. The Health Care Quality Improvement Act of 1986 requires consumers to be provided with informed consent and information about state laws that impact legal choices in making health care decisions. T/F HIT FINAL EXAM REVIEW 3. The Health Care Financing Administration was created to replace the Centers for Medicare and Medicaid Services. T/F HIT FINAL EXAM REVIEW 4. In 1918, just 89 hospitals of 692 surveyed as part of the Hospital Standardization Program met requirements of the Minimum Standard for Hospitals. T/F HIT FINAL EXAM REVIEW 5. The NCRA requires CTRs to submit proof of 30 continuing education hours every two years. T/F HIT FINAL EXAM REVIEW 6. A coding and reimbursement specialist collects cancer data from a variety of sources and reports cancer statistics to government and health care agencies. T/F 7. The American Association of Professional Coders offers the Certified Professional Coder Certification and the Certified Coding Associate Certification. 8. Privacy officers oversee that an organization’s policies and procedures covering the privacy and access of patient health information are in compliance with federal and state laws. T/F 9. Emergency care patients are treated for urgent problems and are admitted to the hospital as inpatients. T/F HIT FINAL EXAM REVIEW 10. A neighborhood health clinic is usually a hospital-based outpatient department. T/F HIT FINAL EXAM REVIEW 11. In a direct contract model HMO, individual physicians in the community deliver contracted health care services to subscribers. HIT FINAL EXAM REVIEW 12. The Food and Drug Administration provides a system of health surveillance to monitor and prevent the outbreak of diseases. T/F HIT FINAL EXAM REVIEW 13. A patient record serves as a business record for the patient encounter and contains administrative and clinical data. HIT FINAL EXAM REVIEW 14. Demographic data is a type of clinical data that identifies a patient’s medical condition. T/F HIT FINAL EXAM REVIEW 15. A consultation report, history and physical exam, and operative report are all types of administrative data. T/F HIT FINAL EXAM REVIEW 16. Administrative data includes demographic, socioeconomic, and financial information. T/F HIT FINAL EXAM REVIEW 17. Since the early 1980s, the provision of outpatient services has decreased. T/F HIT FINAL EXAM REVIEW 18. The ordering physician is not required to countersign a telephone order documented by a nurse. T/F HIT FINAL EXAM REVIEW 19. Fax signatures are not accepted by facilities. T/F HIT FINAL EXAM REVIEW 20. The legibility of patient record entries impacts patient care. T/F HIT FINAL EXAM REVIEW 21. The JCAHO requires that patient records be completed within 20 days after a patient is discharged. T/F HIT FINAL EXAM REVIEW 22. Most facilities organize the patient record according to reverse chronological date order during inpatient hospitalization. T/F HIT FINAL EXAM REVIEW 23. Incident reports should be filed in the patient record. T/F HIT FINAL EXAM REVIEW 24. Source oriented records consist of a database, problem list, and initial plan. HIT FINAL EXAM REVIEW 25. Medicare Conditions of Participation require hospitals to retain medical records for a period of no less than five years. T/F HIT FINAL EXAM REVIEW 26. Every report in the patient record must contain patient identification data. T/F 27. When a facility closes, it is the responsibility of the closing facility to ensure that records are handled according to federal and state statutes. T/F HIT FINAL EXAM REVIEW 28. A principal procedure is performed for definitive or therapeutic reasons. T/F 29. The Health Care Financing Administration is now called the Centers for Medicare and Medicaid Services. HIT FINAL EXAM REVIEW 30 A consent to admission documents a patient’s consent for all medical treatment including procedures and surgeries to be completed during the current admission. T/F HIT FINAL EXAM REVIEW 31. A discharge progress note can be documented in a patient record instead of a discharge summary if a patient had an uncomplicated hospital stay of less than 48 hours. T/F HIT FINAL EXAM REVIEW 32. The history of the present illness is the patient’s description of his current medical condition in his own words. T/F HIT FINAL EXAM REVIEW 33. Integrated progress notes are documented by physicians, nurses, therapists, and other professionals in the same section of the patient record. T/F HIT FINAL EXAM REVIEW 34. An admission note documented by the attending physician can replace a dictated history and physical examination. T/F HIT FINAL EXAM REVIEW 35. Pre-anesthesia and post-anesthesia progress notes are often documented on a separate form to facilitate documentation by the anesthesiologist. T/F HIT FINAL EXAM REVIEW 36. AOA requirements state that laboratory reports should be placed on the record immediately, and they can be signed or initialed by the person performing the test after being filed in the patient’s record. T/F HIT FINAL EXAM REVIEW 37. EKG reports include a graphic printout of measurements of the electrical activity of the brain. T/F HIT FINAL EXAM REVIEW 38. JCAHO standards require that a provisional diagnosis be documented in the patient record within 48 hours after an autopsy is performed. T/F HIT FINAL EXAM REVIEW 38. Indexes and registers allow health information to be maintained and retrieved for the purpose of education, planning, and research. T/F HIT FINAL EXAM REVIEW 39. An index is an organized system for the collection and dissemination of information on individual persons who have a particular disease. T/F HIT FINAL EXAM REVIEW 40. An automated master patient index consists of a computerized database of identification data about patients who have received health care services from a facility. T/F A manual master patient index (MPI) is less expensive to purchase compared with an automated MPI. T/F