PowerPoint - GRECC Audio Conferences
advertisement
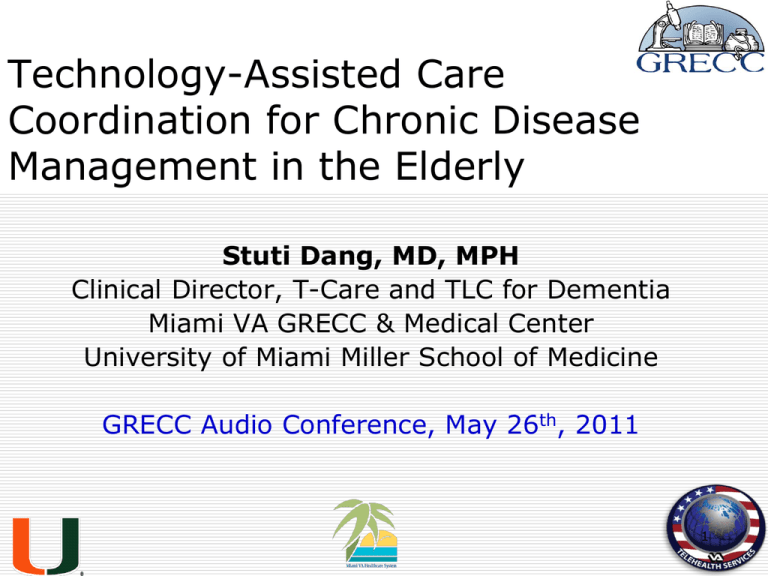
Technology-Assisted Care Coordination for Chronic Disease Management in the Elderly Stuti Dang, MD, MPH Clinical Director, T-Care and TLC for Dementia Miami VA GRECC & Medical Center University of Miami Miller School of Medicine GRECC Audio Conference, May 26th, 2011 1 Objectives Understand definitions of care coordination and home telehealth Discuss examples of technology assisted care coordination for chronic diseases Review proposed reasons for technologyassisted care coordination to work Recognize work ahead 2 Problems With Current System Increasing number of complex older patients with chronic diseases Disproportionate health care resources Fee for service payment structure Fragmentation and duplication Rapidly escalating health care costs Health care delivery system is under stress with shrinking resources 3 Average Annual Per Capita Spending for Patients with Different Numbers of Chronic Conditions Bodenheimer T, et al., N Engl J Med, 2009; 361:1521-1523. 4 Institute of Medicine Priorities for national action (2003): Transforming Health Care Quality -Increased demands -Poorly coordinated care -Inadequate implementation of information technology in health care 5 Care Coordination Definition “Care coordination” is a client-centered, assessment-based interdisciplinary approach to integrating health care and social support services in which an individual’s needs and preferences are assessed, a comprehensive care plan is developed, and services are managed and monitored by an identified care coordinator following evidence-based standards of care. 6 Brown R, in a report commissioned by the National Coalition on Care Coordination, in 2009, at http://www.socialworkleadership.org/nsw/Brown_Full_Report.pdf Impact of Care Coordination Interventions Nurse/SW directed, multidisciplinary interventions in high risk patients Reduced hospital admissions Significantly reduced cost Improved quality of life for patients and caregivers Improved satisfaction of care Rich MW, et al., N Engl J Med, 1995;333(18):1213-4. Naylor MD, et al., JAMA, 1999;282(12):1129 – 36. 7 Care Coordination Interventions Transitional care Self-management education: short community-based programs to “activate” patients in disease self management Coordinated care: patients with chronic conditions at high risk of hospitalization, provide care planning, monitoring of patients’ symptoms and self-care, working with the patient, PCP and caregivers Coleman EA, et al.,Arch Intern Med. 2006 Sep 25;166(17):1822-8. Lorig KR et al. Eff Clin Pract. 2001 Nov-Dec;4(6):256-62. Peikes D, et al. JAMA. 2009 Feb 11;301(6):603-18. 8 Medicare Coordinated Care Demonstration (MCCD) Only 3 of the 15 programs effective Six key components Targeting In-person contact with patients Timely information on admissions Close interaction between care coordinators and PCP: face-to-face and same care coordinator Services provided Staffing: nurses, social workers Peikes D, et al. JAMA. 2009 Feb 11;301(6):603-18. 9 Would Adding Technology Enhance the Model??…….. Technology assisted care coordination may provide an effective and efficient alternative to providing care coordination the traditional way 10 Telemedicine Definition “...the use of electronic information and communications technologies to provide and support health care when distance separates the participants...” Field MJ, et al., Institute of Medicine: Telemedicine: A Guide to Assessing Telecommunications in Health Care, 1996. 11 Telehealth Definition Telehealth (or Telemonitoring) is the use of telecommunications and information technology to provide access to health assessment, diagnosis, intervention, consultation, supervision and information across distance. Includes use for clinical and non-clinical services such as medical education, administration, and research. Center for Medicare and Medicaid Services, 2010, at https://www.cms.gov/Telehealth/12 Care Coordination The Veterans Health Administration defines care-coordination as the “wider application of care and case management principles to the delivery of health-care services using health informatics, disease management, and telehealth technologies to facilitate access to care and improve the health of designated individuals and populations with the intent of providing the right care in the right place at the right time.” http://vaww.telehealth.va.gov/telehealth/ccht/index.asp#info 13 Technology-Assisted Care Coordination Model for Chronic Disease Better Health Outcomes Decreased Cost Increased quality Monitoring Education Feedback Peer Leaders Caregivers Pharmacy Patients at home HTN, DM, COPD, CHF, Asthma, depression, PTSD Specialists Primary Care Providers Education Non VA Providers Support Feedback Care coordination team Support Technologies 14 15 Blood Pressure Graph For a Patient 16 Technology Assisted Care-Coordination Some Examples 17 Telephone-based Management Telephone calls with RN follow-up Biweekly automated telephone calls Maximum benefit when A1c>8% (net effect - 0.5 – 1.1%) Mobile phone and SMS messaging Patients sent glucose result via phone, received message from nurse Decrease in A1c by 1.1% over 12 weeks Piette JD, et al., Diabetes Care, 2001;24(2):202-8. Kim HS, et al., Int J Nurs Stud, 2007;44(5):687-92. 18 Web-based Management 104 Veterans with diabetes, HbA1c 9.0% Web-based care management: notebook computer, glucose and blood pressure monitoring devices, and access to a care management website, messaging system At 12 m, lower A1C, BP, HDL (P < 0.05) More improvement in persistent users and with larger number of website data uploads McMahon G, et al., Diabetes Care, 28:1624–1629, 2005 19 IDEATel - Informatics for Diabetes Education and Telemedicine METHODS Telemedicine home unit with videoconferencing and case management Randomized trial with a usual care group Five year follow up Medicare beneficiaries (n= 1665) Diabetes, >55 years, medically under-served areas in NY (upstate and NYC) Shea S, et al., JAMIA, 2006;13(1):40-51. 20 IDEATel Results Modest clinical effects Small but significant changes A1c (0.29%), SBP (4.3 mm Hg), Lipids (3.8 mg/dl) Reduced waist circumference and BMI Increased diet and exercise knowledge No mortality benefit Costs (Likely under-powered) $622 per person per month Mean Medicare payment in UC $9040 versus IDEATel $9669 per person per yr Moreno L, et al., Diabetes Care, 2009;32(7):1202-4. Palmas W, et al., J Am Med Inform Assoc, 2010;17(2):196-202. Izquierdo R, et al., Diabetes Therapeutics and Technology, 2010;12(3):213-20. 21 The Diatel Study Active Care Management + Home Telemonitoring (ACM+HT=73) Vs. Monthly Care Coordination Telephone Call (CC = 77) Blood glucose, BP, and weight daily in ACM+HT ACM+HT had larger decrease in A1c at 3 months (1.7 vs. 0.7%) and 6 months (1.7 vs. 0.8%; P<0.001 for each) Frequency of self monitored blood glucose did not correlate significantly with reduction in A1c Stone RA, et al., Diabetes Care, 2010;33(3):478-84 22 Multicenter Randomized Trial on Home-based Telemanagement 460 patients with heart failure – 230 each HBT received a portable device to transfer a onelead trace to a nurse by telephone HBT group had lower risk of readmission compared with the Usual Care group (RR = 0.56; 95% CI: 0.38– 0.82; p = 0.01) lower risk of heart failure-related readmission (RR = 0.49, 95% CI: 0.31–0.76; p = 0.0001) No significant difference in cardiovascular mortality Giordana A, et al., Int J Cardiology, 2009;131(2):192-9 23 Telemonitoring to Improve Heart Failure Outcomes (Tele-HF) 1,653 recently hospitalized patients at 33 centers Telephone-based interactive voice-response system, daily information on symptoms and weight No difference in all-cause mortality (11% both groups) or hospital readmission for any reason (49.3% vs. 47.4%; P=0.45) at six months 14% did not use system; 55% used at 6 months Increase contact, formal education, medication management, or peer support to enhance Caution about investment in unevaluated disease management protocols and processes Chaudhry S, et al., NEJM, 2010;363(24):2301-9 24 Effectiveness of Home Blood Pressure Monitoring on Hypertension Control Three-arm randomized controlled trial for 12 m 778 pts, age 25–75, with Internet access Interventions—(1) BP monitoring and secure patient website training (BPM-Web); (2) BPM-Web plus pharmacist care management via web Results: BPM-Web: nonsignificant increase in % with controlled BP compared to UC (36% vs 31%; P = .21) BPM-Web-Pharm: significant increase in % with controlled BP (56%) vs. UC and BPM-Web (P <.001) No difference in PCP, ER or inpatient use Increased web and phone contact in BPM-Web-Pharm Green B, et al., JAMA, 2008; 299(24): 2857–2867. 25 Telemonitoring for COPD – a Systematic Review 9 original studies with 858 patients Home telehealth Reduced rates of hospitalizations Reduced emergency department visits Bed days of care varied Increased mortality based on 3 studies (Risk Ratio 1.21; 95% CI 0.84-1.75) Improved quality of life Improved patient satisfaction Polisena J, et al., J Telemed Telecare,2010;16:120-127. 26 Other Chronic Diseases Interactive asthma education Access to a website: Increased asthma knowledge, reduced symptom days, fewer ER visits, lower steroid doses Weight management using ecounseling Greater weight loss with website access and e-counseling Krishna S ,et al., Pediatrics 2003; 111: 503-510 Tate DF,et al., JAMA 2003; 289: 1833-1836 27 Improvement in Cardiovascular Risk Despite Clinical Inertia Dang S, et al., Diabetes Therapeutics and Technology, 2010;12:995-1001. 28 Veterans Health Administration’s Telehealth Interventions Care Coodination Home Telehealth (CCHT) with over 40,000 Veterans diabetes mellitus (48.4%) hypertension (40.3%) congestive heart failure (24.8%) chronic obstructive lung disease (11.4%) depression (2.3%) and PTSD (1.1%). Reductions in admissions (19.7%) and bed days of care (25.3%) Darkins A, et al., Telemed J E Health, 2008 Dec;14(10):1118-26. Hill RD, et al., Am J Manag Care, 2010;16, e302-e310. http://www.carecoordination.va.gov/telehealth/ccht/index.asp 29 Reduction in Utilization by Condition Monitored in the VHA Condition # of Patients % Decrease Diabetes 8954 20.4 Hypertension 7447 30.3 Chronic Heart Failure 4089 25.9 Chronic Obstructive Pulmonary Disease 1963 20.7 Post Traumatic Stress Disorder 129 45.1 Depression 337 56.4 Other Mental Health Condition 653 40.9 Single Condition 10885 24.8 Multiple Conditions 6140 26.0 Darkins A, et al., Telemed J E Health, 2008 Dec;14(10):1118-26. Hill RD, et al., Am J Manag Care, 2010;16, e302-e310. http://www.carecoordination.va.gov/telehealth/ccht/index.asp Key Contributions of VHA to Teleheath Care Coordination Broadest spectrum of veteran patients Targeting the non institutional care (NIC) patients Standardized procedures for ensuring the security of patient data Highlighted the role of the computerized patient record as a fundamental prerequisite National training program focused on rapidly training staff in care coordination Standardization of the clinical, educational, technical, business, and organizational elements 31 Why Might TechnologyAssisted Care Coordination for Chronic Disease Management Work? 32 33 Chronic Care Model ~ Care Coordination + Technology Benefits stem from re-engineering care, not from addition of technology Patients self-manage Just-in-time versus just-in-case care Proactive not reactive Continuous not episodic Integrate technology into care system Integrate available resources Redesign the system 34 Interactive Behavior Change Technology (IBCT) Any hardware and software to promote and sustain behavior change Assists patients and clinicians in monitoring Assists enhanced frequent communication b/w patients and providers and caregivers Provides ongoing self-management education and support Enables patients’ efforts to change behavior Feedback to providers enables changes in treatment regimens and without office visits Piette JD,et al., Diabetes Care, 2007;30(10):2425-32. 35 Other Potential Benefits of Technology in Care Coordination Case management by exception Enhanced efficiency of care provision Cost effective approach to manage large populations Centralized data management Potential cost savings Access to care Decrease travel time 36 Technology-Assisted Care Coordination –Where does it stand? Establishing programs is feasible Can complement the ability to assess, monitor, educate, and support patients Technology has limitations Some clinical benefits demonstrated Limitations in study design Questions regarding impact on health care utilization, mortality, and cost Questions regarding design Technology is a tool 37 Technology is a tool – Circle of Management Reliable measure of the correct physiological variable(s) Efficient transmission of information Information received by personnel qualified to recommend an appropriate and effective intervention Patient must correctly implement the intervention Reassessment Desai A and Stevenson LW. NEJM, 2010; 363:2364-2367 38 Current and Perceived Challenges People: politics, relationships, provider, patients Cost: capitalization, operations, sustainability Difficult outside an integrated delivery model Reimbursement: unaligned incentives/payments Regulatory: licensure, credentialing, malpractice liability and jurisdiction, protected health information Limitations of technology Systematic protocols, best practices, and standards Lack of adequate outcome data Kang ,et al., J Am Geriatr Soc, 2010; 58:1579–1586. Dang, et al., Telemedicine and e-Health, 2006; 12(1):14–23. 39 Work Ahead… Evidence on cost, effectiveness, and best practices, and guidelines Collaboration between clinicians, patients, academia, industry, and health policy-makers Healthcare system reform Integrated delivery models Payment reform and aligned incentives Regulatory and licensure changes Interoperability of systems and devices Robust, fail-safe systems and operating procedures Interoperability of systems and devices with the creation of a single end user interface interoperable with multiple applications and providers Kang, et al., J Am Geriatr Soc,2010; 58:1579–1586. http://www.ntia. doc.gov/reports/telemed/privacy.htm 40 Interoperability of Systems and Devices 41 Work Ahead… Issues for Ongoing Research Ideal design: technology, professional, patients, protocols Ideal parameter(s) to monitor Episodic vs. continuous enrollment/eligibility For what purpose: prevention, disease management Frequency of monitoring Frequency of communication How to assess technology’s contribution as distinct from other components of care Impact on health care utilization, mortality, and cost Dang, S., et al., (2009). Telemedicine and e-Health. 15 (10),1-14. 42 Health Care Costs are Rising 43 Source: CBO The Health Care Imperative Decrease Cost Improve Outcomes /Quality 44 Patient Protection and Affordable Care Act – Public Law 111-148 Accountable Care Organizations Patient Centered Medical Home Partially Capitated Fully Capitated Independence at Home Project 45 “I don’t want to talk to the doctor, I want my symptoms to go straight through to your computer!” 46 Special Thanks to: Office of Telehealth, VISN 8, and Sunshine Training Center Office of Geriatrics and Extended Care and GRECC Tom Edes, MD Ken Shay, DMD Miami VAHS Adam Darkins, MD Pat Ryan, MSN Rita Kobb, MSN Bernie Roos, MD Adam Golden, MD, MBA Hermes Florez, MD, MPH, PhD Jorge Ruiz, MD Enrique Aguilar, MD Herman Cheung, PhD Past and present care coordinators, fellows, and students 47 48 Technology-Assisted Care Coordination: Design Questions Ideal intervention Technology Professional Patients Protocols Ideal parameter(s) to monitor Duration Frequency of monitoring Frequency of communication Relative contribution of technology vs. coordination Dang, S., et al., (2009). Telemedicine and e-Health. 15 (10),1-14. 49 It's Not About The Technology Most patients are comfortable and adapt to technology Technology has its limitations Patients’ willingness ability to use Providers willingness to be part of it Health informatics and sufficiently robust IT infrastructure can be implemented 50 Issues Plaguing TeleCare Coordination Evaluation Issues Lack of adequate outcome data Few systematic comparative studies that assess effect on quality, accessibility, or cost of health care Unmatched retrospective analyses using a single-group study design regression to the mean Essential Transformational Elements: Patient (Veteran) Centered Care Delivering “health” in addition to “disease care” Veteran as a partner in the team Empowered with education Focus on health promotion and disease prevention Self-management skills Efficient Access Visits Non face-to-face 52 Telephone Secure messaging Telemedicine Others? ACP Medical Home Builder Modules 53 Patient-Centered Care & Communication Access & Scheduling Organization of Practice Care Coordination & Transitions of Care Use of Technology Population Management Quality Improvement & Performance Improvement 54 Technology-Assisted Care: Research Questions Who benefits most? And from which technologies? How long? In which setting? For what purpose, e.g., prevention, disease management? How to assess technology’s contribution as distinct from other components of care Chronic disease management (T-Care and TLC) Health promotion and disease prevention (MOVE) Patient safety and medication reconciliation for community-based dependent elderly U.S. Health Care Spending In 2009, the U.S. spent $2.53 TRILLION on Health Care 56 Home Telemonitoring for Heart Failure: Systematic Review Twenty-five original studies (3062 patients) A random effects model was used to compute average treatment efficacy Reduced mortality (RR 0.66, 95% CI 0.54 to 0.81, P < 0.0001) compared with usual care and CHFrelated hospitalizations (RR 0.79, 95% CI 0.67 to 0.94, P = 0.008) Several studies suggested lower the number of hospitalizations, improved quality of life and satisfaction Polisena J, et al., J Telemed Telecare, 2010;16(2):68-76. 57 Patient Protection and Affordable Care Act – Public Law 111-148 Accountable Care Organizations Patient Centered Medical Home Partially Capitated Fully Capitated Independence at Home Project 58 Communication Links that could be Targeted by Interactive Behavior Change Technology Piette JD, Diabetes Care, 2007;30(10):2425-32. 59 Care Coordinator Role Licensed health care professionals who assess and monitor patients using home telehealth Detect changes in chronic diseases and conditions Identify and coordinate services across a continuum of care Provide education and emotional support for frail patients with complex clinical needs 60 Care Coordination Definition Veterans Health Administration definition: “process of assessment and on–going monitoring of selected patients using telehealth to proactively enable prevention, investigation, and treatment that enhances the health of patients and prevents unnecessary and inappropriate use of resources. This process allows for the appropriate information to be communicated to providers and the healthcare system to assure the right care, at the right place, and at the right time. ” 61 http://vaww.telehealth.va.gov/telehealth/ccht/index.asp#info Types of Applications Store and Forward Remote Monitoring Interactive Services http://www.answers.com/topic/telemedicine#Types_of_telemedicine 62 Patient Centered Goals of Care Coordination Medical, preventive and psychosocial needs Ensure appropriate and comprehensive care Make the patient a partner in his/her care Promote communication Guide through a maze of services Match need with funding and resources Maximum cost effective use of resources Maintain function and independence to enable person to remain in the most independent environment 63 REMOVE Care Coordination Definition “the deliberate organization of patient care activities between two or more participants (including the patient) involved in a patient's care to facilitate the appropriate delivery of health care services. Organizing care involves the marshalling of personnel and other resources needed to carry out all required patient care activities, and is often managed by the exchange of information among participants responsible for different aspects of care. Closing the Quality Gap: A Critical Analysis of Quality Improvement Strategies. 64 Agency for Healthcare Research and Quality (US); 2007 Current and Perceived Challenges Physician skepticism of new healthcare models Coordination outside of an integrated delivery model Reimbursement - Payment reform and aligned incentives Interoperability of systems and devices Developing the evidence Caution about increased use and investment in unevaluated technologies Integrate into existing practice and process 65 Identify best practices Challenges Ahead…Technology Robust, fail-safe systems and operating procedures for lay people Hardware and software with the creation of a single end user interface interoperable with multiple applications and providers Safe, reliable, and secure FDA approval http://www.ntia. doc.gov/reports/telemed/privacy.htm Mahoney DM, et al. Telemed J E Health 2008;14:224–234. 66 The Future……. Dialogue between clinicians and patients and between academia, industry, and health policy-makers regulatory and licensure needs Early real-world testing of technology and collection of cost effectiveness data Guided by geriatrics providers, patients and caregivers Kang, et al., J Am Geriatr Soc,2010; 58:1579–1586. 67 Care Coordination The Veterans Health Administration defines care-coordination as the “wider application of care and case management principles to the delivery of health-care services using health informatics, disease management, and telehealth technologies to facilitate access to care and improve the health of designated individuals and populations with the intent of providing the right care in the right place at the right time.” 68 But Needs Caution……. Nurse care management - 246 patients, A1c 9.3% - Nurse care management using algorithms; follow-up over 18 months - No difference in A1c, BP, lipids - Intervention resulted in greater satisfaction with diabetes care Gagnon AJ, et al., J Am Geriatr Soc, 1999;48(5):596-7. Boult C, et al. J Am Geriatr Soc, 2000;48(8):996-1001. 69 70 IDEATEL – Change in A1c Shea S, et al., JAMIA, 2009;16(4):446-56. 71 Technology-Assisted Care: Some Recent Answers Real Time Transmission of Data 1 year controlled parallel group trial Intervention group assigned to teleassistance system using real time transmission of FSBG with immediate reply when needed + Telephone consultation Control Group 328 T2D from 35 family practices in Spain At 12 months Intervention group with in A1c (7.62 ±1.60 to 7.40 ±1.43; P=0.025) and significant in blood pressure, total and LDL cholesterol, and BMI Control Group with in A1c (7.44 ±1.31 to 7.35 ±1.38; P=0.303) and only decrease in LDL cholesterol Feasible in primary care setting Rodriguez-Idigoras MI, et al., Diabetes Therapeutics and Technology, 2009 ;11(7):431-7. 72 Care Coordination Definition Veterans Health Administration definition: "the ongoing monitoring and assessment of selected patients using telehealth technologies to proactively enable prevention, investigation, and treatment that enhances the health of patients and prevents unnecessary and inappropriate utilization of resources. Care Coordination uses best practices derived from scientific evidence to bring together health care resources from across the continuum of care in the most appropriate and effective manner to care for the patient“ Case management is the foundation of care coordination. VHA Office of Care Coordination, 2003 73 Improvement in Cardiovascular Risk Factors Despite Clinical Inertia 180 160 140 120 SBP mmHg 100 80 p=0.03 p=0.09 60 40 20 0 No Clinical Inertia Baseline Clinical Inertia T-Care 2 Years n = 46; Clinical Inertia is the lack of dose adjustment or initiation of a new medication for BP or lipid 74 management when indicated according to practice guidelines. For BP medication: 10.8%; for lipid medication: 15.5%. Dang S, et al., Diabetes Therapeutics and Technology, 2010 E-Health e-Health is broader than either telemedicine or telehealth and can be described as an emerging field in the intersection of medical informatics, public health and business, that enables health services and information to be delivered or enhanced through the Internet and related technologies. (http://www.biohealthmatics.com/healthinf ormatics/ telemedicine/telemed.aspx ) 75 Reduction in Utilization by Condition Monitored Condition # of Patients % Decrease Diabetes 8954 20.4 Hypertension 7447 30.3 Chronic Heart Failure 4089 25.9 Chronic Obstructive Pulmonary Disease 1963 20.7 Post Traumatic Stress Disorder 129 45.1 Depression 337 56.4 Other Mental Health Condition 653 40.9 Single Condition 10885 24.8 Multiple Conditions 6140 26.0 76 Reimbursement Provider - same Common Procedural Terminology (CPT) code, and add Healthcare Common Procedure Coding System (HCPCS) modifier code ‘‘GT’’ Patient site: Telehealth Originating Site Facility Fee CPT/HCPCS code Q3014 Appropriate clinical code for a separate face-toface visit to account for clinical activities Store and forward - CPT 99090 77 Reimbursement – Medicare Limitations ‘‘Originating site’’ - non-Metropolitan or a rural health professional shortage area Specific CPT codes - consultations, general office visits, psychiatry, psychotherapy, pharmacological management, end-stage renal disease services, and nutrition Particular providers - physician, mid-level practitioner, nurse–midwife or clinical nurse specialist, psychologist, social worker, and registered dietitian or nutritionist 78 List of Medicare Telehealth Services. Vol Pub 100-04 Medicate Claims Processing: CMS Manual System; 2005 Issues for Ongoing Research While much has been learned since the earliest care coordination efforts and the components of effective interventions can now be specified with a substantial probability of success, much remains to be learned. The key issues for which greater clarity is required are: 79 Major Forces Driving Health Care into the Home Aging of the U.S. population Epidemics of chronic diseases Technological advances Health care consumerism Rapidly escalating health care costs 80 . The LifeMasters Demonstration program is a population-based program targeting people dually eligible for Medicare and Medicaid with particular diagnoses and is also at financial risk for program fees. Enrollment through January 2006 was 50,654 (36,182 of whom were in the treatment group). LifeMasters’ fees are lower because it is not providing prescription drug coverage. The 81 Improvement in Cardiovascular Risk Factors Despite Clinical Inertia 180 160 140 120 SBP mmHg 100 80 p=0.03 p=0.09 60 40 20 0 No Clinical Inertia Baseline Clinical Inertia T-Care 2 Years Clinical Inertia is the lack of dose adjustment or initiation of a new medication for BP or lipid management when indicated according to practice guidelines. For BP medication: 10.8%; for lipid medication: 15.5%. TLC and Caregiver Burden 40 35 Zarit Burden Interview Score * 30 25 p<0.05 * 20 15 10 5 0 n=113 n=60 Overall Black Baseline Hispanic TLC Dang et al. J Telemed Telecare 2008;14:443-447. White TLC and Caregiver Depression 25 20 15 CES-D Score 10 5 0 n=113 n=60 Overall Blacks Baseline Hispanics Whites TLC 1 Year Dang et al. J Telemed Telecare 2008;14:443-447.