ANTIBIOTICS
advertisement
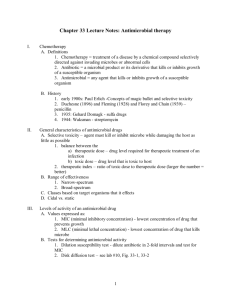
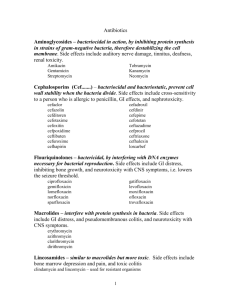
Lecturer: Dr. Thanaa Rasheed © CDC / Gilda L. Jones Definitions 1. Chemotherapy: treatment of a disease by a chemical compound selectively directed against invading microbes or abnormal cells. 2. Antibiotic: a microbial product or its derivative that kills or inhibits growth of a susceptible organism. 3. Antimicrobial: any agent that kills or inhibits growth of a susceptible organism. 1. Early 1900s: Paul Erlich -Concepts of magic bullet and selective toxicity 2. Duchesne (1896) and Fleming (1928) and Florey and Chain (1939) – penicillin 3. 1935: Gehard Domagk - sulfa drugs 4. 1944: Waksman – streptomycin. • The discovery of the first antibiotic was an accident. – Alexander Fleming accidentally contaminated a plate with a fungus. – He observed a clearly defined region of no bacterial growth where the fungi had contaminated the plate. – The area around the fungus was eventually referred to as a zone of inhibition. • Natural products the majority of antibacterial agents in clinical use today are derived from natural products of fermentation • Semi-synthetic chemically modified to improve their antibacterial or pharmacologic properties. • Synthetic (e.g. sulfonamides, quinolones). Therefore the term 'antibacterial' or 'antimicrobial' agent is often used in preference to 'antibiotic'. A. Selective toxicity – agent must kill or inhibit microbe while damaging the host as little as possible 1. balance between the a) therapeutic dose – drug level required for therapeutic treatment of an infection b) toxic dose – drug level that is toxic to host B. Range of effectiveness 1. Narrow-spectrum 2. Broad-spectrum C. Classes based on target organisms that it effects D. Cidal vs. static C. Factors that influence effectiveness a) oral – must survive acid b) topical c) parenteral – non-oral administration (i.e. injection) Tests for determining antimicrobial activity 1. Dilution susceptibility test - dilute antibiotic in 2fold intervals and test for MIC 2. Disk diffusion test. 3. Drug concentration in blood/body Via a variety of tests; important for verifying agent has reached blood or other bodily areas in therapeutic concentrations. Bacteriostatic vs. bactericidal drugs • Bacteriostatic – arrest the growth and replication of bacteria – at serum levels achievable in the patient - limit the spread of infection while the body's immune system attacks, immobilizes, and eliminates the pathogens. – If the drug is removed before the immune system has scavenged the organisms, enough viable organisms may remain to begin a second cycle of infection. • Intact immune system – decreased e.g. in: alcoholism, diabetes, immunosuppresion, malnutrition, advanced age - bactericidal agents are required. • Bactericidal – kill bacteria at drug serum levels achievable in the patient. - often drugs of choice in seriously ill patients. • It is possible for ATB to be bacteriostatic for one organism and bactericidal for another. Bacteriostatic vs. bactericidal drugs: • Minimum inhibitory concentration (MIC) – the lowest concentration of ATB that inhibits bacterial growth. Effective antimicrobial therapy – ATB concentration in body fluids should be greater than the MIC. • Minimum bactericidal concentration (MBC) – the lowest concentration of ATB that results in a 99.9 % decline in colony count after overnight broth dilution incubations. • MIC/MIB – It is an in vitro test in a homogenous culture system, while in vivo: • plasma concentration should reach a value several-times higher (8x) – concentration at the site of infection may be considerably lower than the plasma concentration. • it is necessary to take into consideration pharmacokinetic properties of antibiotics – penetration into site of infection, its metabolism.. Classification of antibacterial agents: bactericidal bacteriostatic β-lactam agents Aminoglycosides Co-trimoxazole Vancomycin Erythromycin Tetracyclines Chloramphenicol Sulfonamides Trimethoprim – only against a single or a limited group of microorganisms, • e.g. INH is active only against mycobacteria. – against G+ organisms and also against a significant number of G- bacteria • e.g., ampicillin • e.g. tetracycline and chloramphenicol – affect a wide variety of microbial species. – !!! alter the normal bacterial flora • precipitate a superinfection of an organism, e.g., candida. Mechanisms of action of antibacterial drugs Inhibition of cell wall synthesis Inhibition of DNA gyrase: RNA polymerase Inhibition of protein synthesis: Inhibition of folic acid metabolism: Disruption of cell membranes Penicillins Cephalosporins Monobactams Vancomycin Quinolones Rifampicin Aminoglycosides Tetracyclines Erythromycin Chloramphenicol Trimethoprim Sulfonamides polymyxin B INHIBITORS OF CELL WALL SYNTHESIS • Bactericidal – selectively interfere with synthesis of the bacterial cell wall • a structure that mammalian cells do not possess. – The cell wall is a polymer called peptidoglycan • that consists of glycan units joined to each other by peptide cross-links. • require actively proliferating microorganisms(cell division) – To be maximally effective, these agents – Little or no effect on bacteria that are not growing – do not combine with bacteriostatic ATBs Figure 1 : ß-lactam A. Inhibitors of cell wall synthesis 1.Penicillins a) derivatives of 6-aminopenicillanic acid (ß-lactam ring is important structure) figure 1 b) mechanism of action: (1) analogue of D-alanyl-D-alanine on peptide side chain of peptidoglycan , inhibits transpeptidase from crosslinking peptidoglycan (2) binds penicillin binding proteins à activation of autolysins c) bactericidal d) effective against gram + and gram -, depending on derivative 2. Cephalosporins a) derivatives of 7-aminocephalosporanic acid b) similar mechanism of action as penicillins c) bactericidal d) broad spectrum e)Four generation 3. Bacitracin a) peptide b) mechanism of action: inhibits dephosphorylation of bactoprenol pyrophosphate c) bactericidal d) mostly effective against gram + 4. Vancomycin a) glycopeptide b) mechanism of action: prevents crosslinking of peptidoglycan by binding to the D-ala-D-ala portion of the cell wall precursor c) bactericidal d) gram + B. Disruption of cell membranes 1. fungal drugs 2. polymyxin B a) basic polypeptides that act as detergents b) mechanism of action: interact with Phospholipids to increase permeability and decrease osmotic integrity à leakage on intracellular components. c) bactericidal d) gram – C. Interference with metabolism: Antimetabolites Sufadrugs (sulfonamides) a) structural analogues of p-aminobenzoic acid . b) mechanism of action: competes with p-aminobenzoic acid for binding to the enzyme dihydropteroate synthetase ,no folic acid synthesis , no nitrogenous base synthesis c) bacteristatic d) broad spectrum D. Protein synthesis inhibition 1. Tetracycline a) 4-ring structure with side chains. b) mechanism of action: reversible binding to the 30s subunit of ribosome à inhibits binding of aminoacyl tRNA to ribosome , inhibition of protein synthesis. c) bacteriostatic. d) broad spectrum 2. Aminoglycosides (streptomycin, kanamycin, gentamicin) a) group of antibiotics in which contain amino sugars and a cyclohexane ring . b) mechanism: irreversible binding to the 30s subunit of ribosome , inhibits protein synthesis and causes misreading of mRNA c) bactericidal d) some are broad spectrum but mostly used against gram negatives. 3. Macrolides (erythromycin) a) 12-22 carbon lactone ring linked to sugars. b) mechanism (erythromycin): reversibly binds 23s rRNA of 50s subunit of the ribosome à inhibits translocation during protein synthesis c) bacteriostatic d) mostly gram + 4. Chloramphenicol a) mechanism: binds to 23S rRNA of 50s subunit of the ribosome , inhibits transpeptidation during protein synthesis b) bacteriostatic c) broad spectrum. E. Inhibition of nucleic acid synthesis 1. quinolones and fluoroquinolones a) characterized by quinolone ring b) mechanism of action: inhibits DNA gyrase , inhibition of DNA replication . c) bactericidal d) broad spectrum 2. rifampin a) macrocyclic compound b) mechanism of action: inhibits RNAP , inhibition of RNA synthesis c) bactericidal d) mostly gram +, some gram negatives Antimicrobial resistance A. Molecular mechanisms 1. decreased drug accumulation a) Prevention of entrance of drug into the cell b) Pumping drug out of cell 2. enzymatic detoxification 3. altered target site B. Origins of resistance 1. Inheritance from mother cell 2. Spontaneous mutation 3. Acquisition of plasmid (R plasmid) or transposon or phage with drug resistance gene a) via conjugation or transformation (plasmid) b) via transduction (phage) Drug resistance • growth of bacteria is not stopped – by the maximal level of that antibiotic that can be tolerated by the host. • Primary – Some organisms are inherently resistant to an antibiotic – e.g., gram-negative organisms are inherently resistant to vancomycin. • Secondary – spontaneous mutation or acquired resistance and selection. • Cross-resistance – resistant to more than one antibiotic. C. Solutions 1. Effective use of antibiotics a) only for appropriate infections b) dual antibiotics c) completion of treatment d) narrow spectrum 2. Drug discovery 3. Rational drug design • It is better to treat patients with the single agent – that is most specific for the infecting organism. – reduces the possibility of superinfection, – decreases the emergence of resistant organisms – minimizes toxicity. • Combination • Special situations • e.g., the treatment of tuberculosis, sepsis • Advantages Synergism – e.g., b-Iactams and aminoglycosides – synergism – rare example • Disadvantages – Hepatotoxity of anti-TBC – Therapy failure static vs cidal • (e.g. TTC X PNC or cephalosporins) Complications of antibiotic therapy • • • • Hypersensitivity Direct toxicity Superinfections Resistance – primary, secondary, cross. Sterilization Is the process of killing or removing all viable organisms. Achieved by: physical & chemical Disinfection Is the process of removing or killing most but not all viable organisms. 1. Chemical The substance is called a disinfectant it kills pathogens but may not kill viruses or spores 2. Physical process Boiling or low pressure steam – reduces only the bioburden. Antiseptics: A particular group of disinfectants – used to reduce the number of viable organisms in the skin. Act differentially on organism and host tissue 1. Germicide Chemical agent capable of killing microbes 2. Sporicide A germicide capable of killing bacterial spores . Pasteurization: Reduces the total number of viable microbes in bulk fluids such as milk and fruit juices without destroying flavor and palatability. Uses 1. Prevention of hospital infection depends on o sterile equipments, instruments and dressings. o isolation facilities. o safe disposal of infected materials 2. Microbiologists o production of sterile media and the laboratory activities 3. Central to almost all areas of medical practice like surgery(from hand washing to needles and prosthesis) Process: The rate of killing of microorganisms depends upon the concentration of the killing agent and time of exposure. N = 1/CT N – number of survivors ; C – concentration of agent ;T – time of exposure to the agent Factors affecting efficacy 1. Physical environment 2. Presence of moisture 3. Temperature and Ph 4. Concentration of the agent 5. Hardness of water 6. Bioburden and the object 7. Mature and state of microbes in bioburden 8. Ability of microbes to inactivate the chemical agent Techniques for Sterilization A. Heat – preferred choice 1. 2. 3. 4. ease of use controllability cost efficiency Types: 1. Dry heat o Incineration o use of bunsen burner . o hot air oven (one hour) 2. Moist heat under pressure o autoclave - most effective for sterilization (121oC, 15 mins.) o pressure aids in penetration o derived from thermal death curves for pathogens like Clostridium o sterilization of surgical instruments, dressing and heat resistant pharmaceuticals 3. Boiling Water o for a few minutes can be used as a rapid emergency measure to disinfect instruments o kills vegetative bacteria but not all spores 4. Pasteurization o done at 62.8 – 65.6°C for 30 minutes o used for fluids o reduce the number of bacteria o eliminate pathogen present in small numbers o improve shelf-like of milk o Flash pasteurization 71.7 ° C for 15 secs. after the process, the fluid should be kept at a temperature below 10 ° C to minimize, subsequent bacterial growth. B. Irradiation Gamma irradiation – used for sterilizing large batches of small volume items such as: 1. Needles, syringes, catheters, gloves 2. Vaccines 3. To prevent food spoilage capital cost is high but process is 100% efficient killing mechanism involves production of free radicals that break the bonds in DNA sporocidal at higher doses (4.5 mega rads) C. Filtration • used to produce particles and pyrogen-free fluid. • composed of nitrocellulose • work by electrostatic attraction and physical pore size • purify drinking water • to recover very small number of organism from large volumes of fluid • can be used for quantitating bacteria in fluids D. Chemical agents (liquid or gas phase) 1. Alkylating agents a. Gases i. ethylene oxide (toxic and explosive; prosthetic heart valves) ii. formaldehyde (extremely unpleasant odor; and irritant to mucous membrane decontaminate rooms and exhaust protective cabinets) b. Liquid i. Glutaraldehyde - disinfects of heat–sensitive articles (endoscopes and inanimate surfaces) . 2. Oxidizing agents a. Hydrogen peroxide • 3 – 6% kills most bacteria • 10-25% kills all including spores • (disinfects plastic implants, contact lenses and surgical prosthesis) b. Halogens – I2 or Cl2 containing: . Iodine compounds • most effective, virtually effective among all organisms including spore- former sand mycobacteria. • effective in acid pH because more free I2 is liberated • acts more rapidly than other halogens and quarternary NH4compounds • effectivity reduced by serum, feces, body fluids. Povidone iodine used to disinfect metalsurfaces and tissues. Chlorine compounds used extensively 3 forms available ,Cl2, HOCl( hypochlorous acid) , OCl (hypochlorite) good germicide activity, though spores are resistant to it. Phenolic compounds o rarely used as disinfectant nowadays o historical interest it was used as comparative standard for assessing the activity of germicidal compounds . o sporocidal at T approaching 100°C but not at room temperature o effective on resistant mycobacteria o Activity potentiated by halogenation and aromatic group into their nucleus o Hexachlorophene 4. Quarternary Ammonium compounds Bacteriostaticat low concentrations, bactericidal at high. Not effective against Pseudomonas, Mycobacteria and Trichophyton). 5. Alcohols o germicidal activity increases with increasing chain length (5-8 carbons) o most commonly used – ethanol and isopropanol o no activity against spores o activity is more active in the presence of water hence 70% alcohol is more active than 95% alcohol. o common disinfectants used for skin surfaces o extremely effective when followed by treatment with iodophor. 6. Heavy metals o soluble salts of Hg, arsenic, silver and other heavy metals o by forming mercaptides with sulfhydryl groups of cysteine residue o mercurials – merthiolate, mercurochrome o silver compounds – irritant and caustic effect; silver nitrate (propylax is);sulfadiazine cream; wound, culloidal silver compounds used in ophth E. Others – freezing, lysis, dessication, ultrasonication, use of electrical discharges