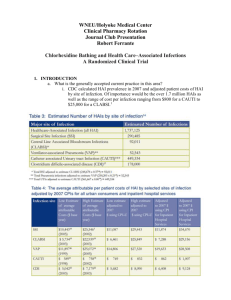
Estimating Infection Rates
advertisement

Developing a Framework for Estimation of Healthcare-Associated Infection Burden at the National and State Level Matthew Wise, MPH, PhD Epidemiologist, Office of Prevention Research and Evaluation CSTE Annual Conference June 4, 2012 National Center for Emerging and Zoonotic Infectious Diseases Division of Healthcare Quality Promotion Importance of HAI Burden Estimates Defining the public health impact of HAIs Morbidity, mortality, and cost Where is burden greatest? How should public health resources be allocated? How has burden changed with implementation of prevention programs or policies? Useful communications tool Policymakers may relate better to numbers than rates Can aid in advocating for resources Major Healthcare-Associated Infection (HAI) Types Device-associated infections: Bloodstream infections in patients with central lines (CLABSI) Urinary tract infections in patients with catheters (CAUTI) Pneumonias in ventilated patients (VAP) Surgical site infections (SSI): Superficial and complex infections following surgical procedures Multidrug-resistant and other important pathogens: Methicillin-resistant Staphylococcus aureus (MRSA) Clostridium difficle infections (CDI) Previous HAI Burden Estimates Expanding on Previous Burden Estimates Ability to project to the state level Focus on HAI types that are targets of prevention efforts Take advantage of more robust HAI data What’s Changed? HAI surveillance is much more comprehensive From hundreds of facilities in the 1990s to thousands of facilities currently Data collected on a larger number of infection types Greater access to National Healthcare Safety Network data at the state level State reporting requirements Group user function CMS Reporting Incentive Timeline HAI type Setting/description Date implemented CLABSI Acute care hospital critical care units January 2011 CAUTI Acute care hospital critical care units January 2012 SSI Acute care hospitals: COLO and HYST January 2012 Dialysis Events Outpatient dialysis centers: IV antimicrobial starts, BSI, access infection January 2012 CLABSI Long-term acute care hospitals October 2012 CAUTI Long-term acute care hospitals October 2012 CAUTI Inpatient rehabilitation facilities October 2012 MRSA BSI Acute care hospitals: LabID event January 2013 CDI Acute care hospitals: LabID event January 2013 Median State-Specific Percent of Acute Care Facilities Participating in HAI Surveillance 2009 2011 CLABSI 9% 61% CAUTI 6% 27% SSI 4% 18% VAP 7% 15% CDI 0% 3% A Common Approach CDC and some states already producing HAI burden estimates or exploring burden estimation Benefits of a common (or at least coordinated) approach: (Relatively) comparable estimates across states Internally consistent estimates (e.g., sum to the ~national total) Greater efficiency by developing standard methods and data sources What is needed to produce HAI burden estimates? Is there a source of data on the frequency of infections that is generalizable to the population I want to calculate burden for? Example: “Do I have information on the rate of CLABSIs in hospitalized critical care patients in the United States?” Do data exist to define the entire population at risk for the outcome of interest? Example: “Do I know the total number of central line-days in hospitalized critical care patients in the United States?” Simple Approach to HAI Burden Estimation Define the denominator: Estimate infection rates: Patient-days Device-days Procedures CDI CLABSI/CAUTI/VAP SSI Multiply Number of infections Simple Approach to HAI Burden Estimation Define the denominator: Estimate infection rates: Patient-days Device-days Procedures CDI CLABSI/CAUTI/VAP SSI Multiply Number of infections Defining the Denominator: Data Sources AHRQ Healthcare Cost and Utilization Project State hospital discharge data CMS Healthcare Cost Reports Defining the Denominator: AHRQ Healthcare Cost and Utilization Project Source of national data on non-Federal short-stay community hospital discharges Also state-specific data available for 35 states Information can be used to estimate patient-days and surgical procedure denominators HCUPnet web query system http://hcupnet.ahrq.gov/ Defining the Denominator: State Hospital Discharge Data “Raw” state-specific discharge data files that HCUP uses to create its databases Data on patient-days and surgical procedures Ability to design more complex queries Can be difficult/cumbersome to access in some states Defining the Denominator: CMS Healthcare Cost Reports Filed by all Medicare-eligible hospitals, nursing homes, dialysis facilities, hospice, and home health agencies Publicly available, but files difficult to work with Patient-day data stratified by hospital type and critical care status http://www.cms.gov/Research-Statistics-Data-and-Systems/Filesfor-Order/CostReports/Cost-Reports-by-Fiscal-Year.html Defining the Denominator: Complications General issues Most data sources exclude Federal facilities Administrative data can lag by 1-3 years Device-associated infections Need to stratify patient-day denominators by critical care status Must take device utilization into account Surgical site infections NHSN procedures may not map directly to ICD-9-CM procedure codes used in hospital discharge data An Example of Estimating Burden: CLABSIs in Critical Care Patients, US, 2010 Estimate critical care patient-days from CMS Hospital Cost Reports and inflate by 4% to account for Federal hospitals 20.8 million*1.04=21.7 million total patient-days An Example of Estimating Burden: CLABSIs in Critical Care Patients, US, 2010 Obtain device utilization ratio from NHSN and convert patient-days to central line-days 21.7 million*0.50 = 10.8 million central line-days 21.7 million US critical care patient-days Simple Approach to HAI Burden Estimation Define the denominator: Estimate infection rates: Patient-days Device-days Procedures CDI CLABSI/CAUTI/VAP SSI Multiply Number of infections Estimating Infection Rates: Data Sources Hospital discharge data Emerging Infections Program National Healthcare Safety Network (NSHN) Estimating Infection Rates: Discharge Data Few HAIs can be accurately identified using administrative data sources CDI ICD-9-CM code 008.45 does a reasonable (but not perfect) job of identifying CDI Primary diagnosis correlated with community-onset infection Secondary diagnosis correlated with hospital-onset infection Some surgical site infections Example: Some success in identifying post-CABG mediastinitis using a combination of ICD-9-CM diagnosis and procedure codes Estimating Infection Rates: Emerging Infections Program Captures infections occurring in community and healthcare settings Rates generally calculated per 100,000 population Active Bacterial Core Surveillance (ABCs) Invasive MRSA surveillance Healthcare-Associated Infections-Community Interface CDI surveillance HAI and antimicrobial use prevalence survey of hospitalized patients Estimating Infection Rates: National Healthcare Safety Network Voluntary, incentivized, and mandatory reporting of HAIs to CDC by healthcare facilities and organizations Outcomes under surveillance (selected): Hospital-onset CLABSI, CAUTI, and VAP rates per 1,000 device-days Surgical site infections per 1,000 procedures (40 different procedure types) Dialysis events (IV antimicrobials, BSI, access infection) per 100 patient-months by vascular access type Multidrug-resistant organism and CDI rates based on patient-days or admissions Estimating Infection Rates: Complications Discharge data is useful in only specific circumstances EIP data only collected from (at most) ten geographic areas and may not represent the locality for which estimates are being generated NHSN The units/facilities participating in surveillance may be systematically different than non-participants Reported data from participants may not represent “ground truth” Primarily captures infections with onset in hospitals and other inpatient healthcare facilities (some exceptions) Simple Approach to HAI Burden Estimation Define the denominator: Estimate infection rates: Patient-days Device-days Procedures CDI CLABSI/CAUTI/VAP SSI Multiply Number of infections An Example of Estimating Burden: CLABSIs in Critical Care Patients, US, 2010 ~16,000 critical care CLABSIs in 2010 Multiply critical care CLABSI rate by central linedays to estimate infections: *10.8 million*(1.46/1000) 10.8 million US central line-days 21.7 million US critical care patient-days Additional Considerations For point estimates Is infection data representative of in my entire jurisdiction Are there reasons the data might not represent “ground truth”? When examining trends Definition and surveillance system changes Changes in the types of units/facilities participating in surveillance Growing “at risk” population may need a counterfactual comparison Uncertainty Sensitivity analyses Monte Carlo simulation Summary HAI infection rate data is increasingly robust enough to produce estimates at the state level More infection types Greater number of settings Numerous supplemental (and often publicly available) data sources exist to facilitate extrapolation of infection rates to estimate burden at the state level Future Burden Estimation Efforts When can we just start counting infections reported to NHSN? How can reliable estimates be produced for less populous areas? Can we produce more comprehensive HAI burden estimates (i.e., less piecemeal)? Could state-specific HAI denominators (e.g., patientdays, device-days, procedures) be made publicly available? Contact Information: Matthew Wise, MPH, PhD Prevention and Response Branch Division of Healthcare Quality Promotion, CDC cxx4@cdc.gov For more information please contact Centers for Disease Control and Prevention 1600 Clifton Road NE, Atlanta, GA 30333 Telephone: 1-800-CDC-INFO (232-4636)/TTY: 1-888-232-6348 E-mail: cdcinfo@cdc.gov Web: http://www.cdc.gov The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention. National Center for Emerging and Zoonotic Infectious Diseases Division of Healthcare Quality Promotion