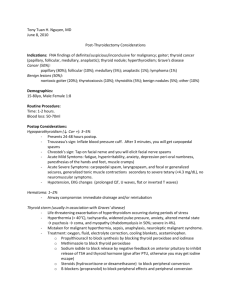
The Recurrent Laryngeal Nerves
advertisement

Thyroid Surgery and Nerve Monitoring Course The Recurrent Laryngeal Nerves Dr Frank CT Voon Frank_Voon@nuhs.edu.sg http://courseware.nus.edu.sg/som/Anatomy Advanced Surgery Training Centre National University Hospital 2 June 2010 Innervation of the Larynx The larynx receives motor and sensory supply from the right and left vagus nerves through 3 nerves on each side. These are the: Internal laryngeal nerve External laryngeal nerve Recurrent laryngeal nerve. The internal laryngeal nerve contains afferent or sensory fibers. The external laryngeal nerve contains efferent or motor fibers. The recurrent laryngeal nerve contains both sensory and motor fibers. The Vagus Nerves Each vagus nerve initially gives off 2 branches, the superior laryngeal nerve and the recurrent laryngeal nerve. The superior laryngeal nerve then subsequently divides into an internal laryngeal nerve and the external laryngeal nerve. The external laryngeal nerve pierces the inferior constrictor of the pharynx and enters the cricothyroid. It supplies both muscles. The internal laryngeal nerve carries sensory fibers from the mucosa of the larynx above the level of the vocal folds. The terminal branches of the internal laryngeal nerve communicate with the sensory branches of the recurrent laryngeal nerve. The Recurrent Laryngeal Nerves The sensory fibers in the recurrent laryngeal nerve supply the mucosa of the larynx below the level of the vocal folds. The motor fibers in the recurrent laryngeal nerve supply all the intrinsic muscles of the larynx except cricothyroid. The right and left recurrent nerves branch off from the vagus nerves at different levels following the development of the aortic arches in the embryo. The right recurrent laryngeal nerve hooks under the first part of the subclavian artery. The left recurrent laryngeal nerve hooks under the arch of the aorta and the ligamentum arteriosum. The Tracheo-Esophageal Groove The right and left recurrent laryngeal nerves then ascend near or in the groove between the trachea and the esophagus to reach the larynx and the lower lobe of the thyroid gland. Both nerves are closely related to the thyroid gland. Both nerves are closely related to the inferior thyroid artery. Both recurrent laryngeal nerves therefore pose a danger in thyroid operations. Each recurrent laryngeal nerve divides into two or more branches before passing deep to the lower border of the inferior constrictor of the pharynx and behind the cricothyroid joint to enter the larynx. The Right Recurrent Laryngeal Nerve At the level of the lower border of the thyroid, it is usually no more than 1 cm lateral to (or within) the tracheo-esophageal groove. At the level of the midportion of the thyroid, it is within the tracheoesophageal groove, and is usually found either anterior or posterior to a main branch of the inferior thyroid artery. Here, it may divide into 2 or more branches. The most important branch travels beneath the inferior border of the cricothyroid muscle (note that the cricothyroid muscle is supplied by the external laryngeal nerve). The other branches enter in the spaces above or below the first or second rings of the trachea. The Left Recurrent Laryngeal Nerve The right and the left recurrent laryngeal nerves are consistently found in the tracheo-esophageal groove when they are within 2.5 cm of their entry into the larynx. The recurrent laryngeal nerve passes either below or behind a branch of the inferior thyroid artery before entering the larynx at the level of the cricothyroid joint (lower border of the cricothyroid muscle). The nerve is closely related to the superior parathyroid gland, the inferior thyroid artery and the posterior part of the thyroid gland. Careful dissection is needed to avoid stretching of the nerve as it is basically tethered to the cricothyroid muscle when it passes below the muscle. Nerve Injuries Injury to a recurrent laryngeal nerve leads to paralysis of the vocal cord on the affected side, with the vocal cord remaining in a median position or just lateral to the midline. Speech is still possible if the contralateral vocal cord can approximate the paralyzed cord though the voice is weakened. Severe impairment of the voice and ineffectiveness of coughing will result when closure is not possible due to the paralyzed cord being in an abducted position. Complete loss of voice can result with obstruction to the airway that may require emergency intubation and tracheostomy if there is bilateral damage to the recurrent laryngeal nerves. At times, bilateral injury may lead to the cords being in an abducted position which will allow air flow though it may result in upper respiratory tract infections from ineffective coughing. The Internal Laryngeal Nerve The superior laryngeal nerve begins to separate from the vagus nerve at the base of the skull. It descends alongside the internal carotid artery to reach the superior pole of the thyroid gland. At the level of the cornu of the hyoid, the superior laryngeal nerve divides into the internal laryngeal nerve and the external laryngeal nerve. The internal laryngeal nerve is the larger branch of the superior laryngeal nerve. It is afferent and contains sensory fibers. It enters the thyrohyoid membrane to innervate the mucosa of the larynx, above the level of the vocal fold. The External Laryngeal Nerve The external laryngeal nerve is efferent and contains motor fibers. It is the smaller branch of the superior laryngeal nerve and continues to travel on the lateral surface of the inferior constrictor of the pharynx. It usually descends anteriorly and medially together with the superior thyroid artery. Within 1 cm of the entrance of the superior thyroid artery into the capsule of the thyroid gland, the external laryngeal nerve usually turns medially to enter and innervate the cricothyroid muscle. During thyroid lobectomy, the external laryngeal nerve may not be seen if it has already entered the fascia covering the inferior constrictor of the pharynx. If the blood vessels are ligated at too great a distance from the superior pole of the thyroid gland, the external laryngeal nerve may be damaged. This can result in a severe loss in quality and strength of the voice. Intrinsic Muscles of the Larynx Cricothyroid - stretches and abducts the vocal cords Posterior cricoarytenoid - abduction and external rotation of the arytenoid cartilages, resulting in abducted vocal cords Lateral cricoarytenoid - adduction and internal rotation resulting in adducted vocal cords Transverse arytenoid - adduction, resulting in adducted vocal cords Oblique arytenoid - adduction and narrowing of the laryngeal inlet Vocalis increases the thickness of the cords and changes the tone Thyroarytenoid - narrows the laryngeal inlet. Note that the posterior cricoarytenoids are the only muscles that abduct the vocal cords. Their paralysis (eg from bilateral injury to the recurrent laryngeal nerves) will lead to breathing difficulties. The ligament of Berry The thyroid gland has its own capsule. The pretracheal fascia surrounding the trachea also encloses the capsule. The part of the capsule of the thyroid gland that fuses with the pretracheal fascia laterally and posteriorly is known as the ligament of Berry. The ligament is closely attached to the cricoid cartilage. Important surgical implications The recurrent laryngeal nerves ascend in the tracheo-esophageal groove and enter the larynx just lateral to the ligament of Berry. Both recurrent laryngeal nerves are usually in the tracheo-esophageal groove when they are within 2.5 cm of their entrance into the larynx.