NHS Western Isles - Recruit & Retain
advertisement
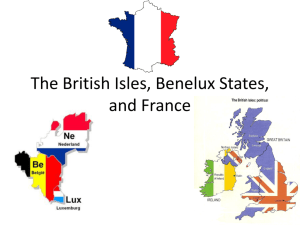
Recruitment and Retention of Health Care Providers in Remote Rural areas Status report for Western Isles Authors: Deanne Gilbert Martin Malcolm Andrew Sim [September 2011] Contents 1 Introduction 3 2 Geography 3 3 Demography, socio-economic trends and population health impacts. 6 3.1Demographics 6 3.2 3.1.1Population Projections 6 3.1.2Age distribution of population 6 3.1.3 Migration Trends 7 Life expectancy / neonatal mortality 8 3.3Socio-economic challenges and Rural Deprivation: 9 3.3.1 Employment status 10 3.3.2 Income deprivation 10 3.3.3 Rural deprivation 11 3.4 Health Impacts from demographic, geographical and socio-economic challenges 12 4 The organisation of the health care services 14 4.1 Primary health care 14 4.2 Hospitals / Specialised service 15 5 Health care professionals 17 6. Urban comparison area 19 6.1 Demographics 20 6.2 Healthcare Services 21 6.2.1 Hospitals 21 6.2.2 Community Hospitals 21 6.2.3 Community Health Partnerships 22 6.3 NHS Grampian Staffing (healthcare professionals) 23 7Education and training 24 7.1 Medical Education 24 7.2 Nurse Education 24 7.3 Other Education 24 8 Vulnerability and sustainability of Services 25 Page 2 of 28 1 Introduction This report provides baseline information about the Western Isles of Scotland. It forms the basis for comparisons in the area of recruitment and retention of Health Care providers. The report includes general information about the islands including; geography and demography, the organisation of the health care services and health care staff 2 Geography The Western Isles is a chain of 150 miles of sparsely populated islands in the Atlantic Ocean 30 miles off the Northwest coast of Scotland with 280 townships. The archipelago of Islands is also known as the Outer Hebrides and officially called by the Gaelic name, Na h-Eileanan Siar. The main islands are - from north to south - Lewis, Harris, North Uist, Benbecula, South Uist and Barra. The islands have an extensive coastline, approximately 2,500km in length, and there are many sea lochs, bays and inlets. The settlements on Lewis are on or near the coasts or sea lochs, being particularly concentrated on the north east coast. The interior of Lewis is a large area of moorland from which peat is traditionally cut for fuel. The southern part of Lewis, adjoining Harris, is more mountainous with inland lochs. Stornoway is the administrative capital of the Outer Hebrides and located on the east coast of Lewis. Stornoway is also the main transport hub with an airport, ferry terminal and bus services on the Outer Hebrides. The Outer Hebrides have a unique culture and tradition. Most communities in the Outer Hebrides use the Scottish Gaelic language. With only 26,000 inhabitants and 8.5 people per square kilometre the Western Isles are one of the most sparsely populated areas in Scotland. Page 3 of 28 There are 12 populated islands in the Outer Hebrides: Lewis and Harris 19,918, South Uist 1,818, North Uist 1,271, Benbecula 1,219, Barra 1,078, Berneray 130, Scalpay 322, Great Bernera 233, Grimsay 201, Eriskay 133, Vatersay 94, Baleshare 49. Climate The Western Isles have a marine climate dominated by ‘North Atlantic Drift’, with only slight temperature changes throughout the year. Winters are rarely cold and snow is almost non-existent. Climatically the dominant features are wind and rain, December being the wettest month of the year. In contrast to the winters, when the days are quite short, in the summer the actual daylight hours are extremely long with lots of daylight with barely two hours of darkness midsummer due to the northerly latitude of the Islands. Travel The Western Isles are accessed from mainland Scotland by ferries and airplanes. There are ferries from Uig on The Isle of Skye to Tarbert on The Isle of Harris, from mainland Scotland, Ullapool to Stornoway and from Oban to Barra and Oban to South Uist. There are airports at Stornoway in Lewis, Benbecula and Barra, with flights to and from Aberdeen, Edinburgh, Glasgow and Inverness on the Scottish mainland and inter island flights to Barra and Benbecula. The Western Isles has a good bus service. Many of the smaller islands are linked by road causeways and bridges, which have been built over a period of time. Off Island transport is dependent on good weather with the Islands often “cut off” in winter. Remoteness challenge The effects upon both service delivery and many aspects of the health status of the population from the islands demographic and socio-economic position are inextricably linked to the geographic challenges faced. This is felt in terms of both the Western Isles remote islands status and the overwhelmingly rural nature of its communities. Page 4 of 28 Scottish Government 8 Fold Urban-Rural Classification Map, 2007-08 Source: Scottish Government8 Fold Urban-Rural Classification Scheme, 2007-08 Seventy eight percent of the Western Isles’ population live in areas classified as very remote-rural compared to 3.2% in Scotland as a whole, this is the largest remote-rural proportion of any health board area.1 The Western Isles has the second lowest population density at 8.5 persons/square km of all Scottish health boards , the Scottish average is 65.2 persons/sq. km.2These remoteness and sparsity factors of the Western Isles population place obvious challenges in delivering health services particularly where the focus of government policy is to provide care as near to the patient as possible. The 1 Scottish Government 8-Fold Urban-Rural Classification Scheme 2 General Registrars Office Scotland Page 5 of 28 implications of such factors for the population’s health are felt in terms of accessibility of services and also in other direct impacts on a person’s health arising from the economic vulnerability and social isolation of their remote-rural situation. 3 Demography, socio-economic trends and population health impacts. 3.1 Demographics Demographic trends have a clear impact on workforce planning and population health needs both through the overall changes in population size and in the age/gender composition. 3.1.1 Population Projections The Western Isles’ population has experienced significant decline for a number of years with falling birth rates being the main factor. This is forecast to continue into foreseeable future (See graph below) with the Western Isles Health Board area expected over the next 25 years to have the second largest percentage decrease in Scotland. Projected % Change in Health Board Populations, 2008-2033 25 20 % Change 15 10 5 0 -5 -10 Shetland Western Isles Greater Glasgow & Clyde Ayrshire & Arran Dumfries & Galloway Lanarkshire Tayside Fife Highland Orkney Grampian Forth Valley Borders Lothian -7 -4 -2 -2 -1 5 10 10 11 12 12 13 16 19 %Change 3.1.2 Age distribution of population The latest population estimates for 2009 and projections to 2033 are shown below as population pyramids (Figures 1a-b). These show the increasing aged profile of the Western Isles population with 2033 projection set to become a mushroom shaped profile with the largest proportion of the population in the 55+ age groups and the 5 year age bands under 16 becoming the lowest age groups. This is a typical profile of a population in demographic decline. Page 6 of 28 3.1.3 Migration trends Recent net migration trends have shown a small increase in net migration to Western Isles. However, the overall trends mask varying patterns among the different age groups in the Western Isles. Western Isles and Scottish Rates/1,000 persons net migration, 2005-10 Total net migration 10.00 8.00 Not specified SCOTLAND 6.00 Western Isles 4.00 2.00 0.00 -2.00 2005 2006 2007 2008 2009 2010 Year Looking at average annual migration trends for in/out and net migration shows a quite marked deviation from overall trends for those aged around 16-24 (see chart below). Page 7 of 28 The biggest net loss of people is in the 17 to 20 age group – particularly young women. This is common across all Scottish island health boards though it is greatest among Western Isles population. Out migration of young persons is to some extent compensated by immigration but the net effect remains negative. In-migrants to Western Isles after period of increase has been declining in recent years and this is particularly among overseas working age in-migrants. This is reflected in the drop in National Insurance Number allocations to overseas nationals working in the Western Isles since 2007 particularly in the EU Accession States which has dropped from 80 to 30 in 2009 (Source: DWP) 3.2 Life expectancy / neonatal mortality In recent years life expectancy has been improving for both men and women within the Western Isles, but there remains significant variation between men and women and between Western Isles and the national average. Life expectancy in the Western Isles for latest period is significantly worse for men than women by approximately 9 years at birth(Fig. 4). While women have significantly greater life expectancy in Western Isles compared to Scotland as a whole men on the other hand have a significantly lower life expectancy. Page 8 of 28 : Life expectancy at birth, 95% confidence intervals for NHS Board areas, 20072009 (Males and Females) SCOTLAND Borders Grampian Dumfries & Galloway Lothian Highland MALE Tayside FEMALE Shetland Forth Valley Fife Orkney Ayrshire & Arran Lanarkshire Western Isles Greater Glasgow & Clyde 68 70 72 74 76 78 80 82 84 86 Years 3.3 Socio-economic challenges and Rural Deprivation: The Western Isles face undoubted socio-economic challenges such that resource deprivation is a very real aspect of life for some of the islands population. This can include low household income and access to affordable and good quality housing. Hence, Western Isles has the 3rd lowest average household income in UK at just £23,400 out of total of 121 areas3 while over 10% homes in Western Isles are ‘below tolerable standard’ compared to 0.5% for Scotland as a whole.4 The Scottish Index of Multiple Deprivation (SIMD) is currently the main measurement used by the Scottish Government to rank communities by their level of deprivation according to a number of factors including employment, income, housing, education & training, geographic access and crime. The Western Isles does not have any communities recognized as falling within the most deprived group, which affects the resources made available for regenerating communities and targeting inequalities. It has been recognized that this area-based deprivation measure is not suited to identifying rural deprivation which is not concentrated in particular areas as tends to be the case for more urban communities. 3 Wealth of Nation Report, 2003 4 2002 Scottish House Condition Survey, 2004 Page 9 of 28 3.3.1 Employment status Thirty eight percent are employed in the public sector, of which the majority are women (55.9%); 62.1% are employed in the private sector, of which the majority are men (75.4%). The employment rate level for 2010 was 11,400 (68.7%). The Outer Hebrides had the highest percentage change over the last 2 years, - 8.7% (-1,600). Employment rates (16-64) by local authority, Scotland. Change over two years (2008-2010) 3.3.2 Income deprivation The Western Isles is among the most income deprived areas within Scotland (see chart below). Rate Income deprived/1,000 working age population 450.0 400.0 350.0 no./1,000 300.0 250.0 200.0 150.0 100.0 local authority area Note: Income deprived based on no. of income deprived persons in SIMD2009. Page 10 of 28 Aberdeenshire Aberdeen City East Renfrewshire East Dunbartonshire Shetland Islands Perth & Kinross Orkney Islands Edinburgh, City of Moray Stirling East Lothian Midlothian Scottish Borders Highland Argyll & Bute Falkirk Angus Fife West Lothian Scotland South Ayrshire Dumfries & Galloway South Lanarkshire Eilean Siar Renfrewshire Clackmannanshire East Ayrshire Dundee City North Ayrshire Glasgow City West Dunbartonshire Inverclyde 0.0 North Lanarkshire 50.0 3.3.3 Rural Deprivation The link between such socio-economic deprivation and health outcomes is well known and the targeting of rising health inequalities is a challenge in the Western Isles. The remote and rural nature of Western Isles’ communities makes the challenge yet more difficult as deprivation here is not found in the concentrations seen in urban areas. Such urban concentrations can be readily targeted. In the Western Isles with more heterogenous communities deprivation is found on individual basis and as a result is often less visible. The challenge for services is how to tackle the inequalities that exist in a targeted manner given their geographical distribution. In recognition of the challenge of identifying rural areas of deprivation the Office of the Chief Statistician produced a methodology based on the existing SIMD and Rural classified areas to identify those rural areas with greatest levels of deprivation in terms of income, employment and accessibility. Areas within the Western Isles featured strongly as those most deprived across rural Scotland. (see map below). Source: Office of Chief Statistician and Ordnance Survey Page 11 of 28 3.4 Health Impacts from demographic, geographical and socio-economic challenges There are a number of population health impacts facing the Western Isles arising from a combination of our ageing population, remote geography both from mainland centres and within the islands, and the comparatively low socio-economic position and dispersed rural deprivation of our communities. The Western Isles already has one of the highest proportions of older people of any area in Scotland. With this expected to increase the impacts upon a range of chronic long term conditions are projected to be significant. The table below indicates the projected rise of prevalent cases within the population for selected conditions and those where there is a relationship to ageing have the largest expected increases eg. Dementia, CHD, COPD. These figures are based on the projected population figures and do not take account of improvements in healthcare, diagnosis, etc. which may expect further rises in numbers of persons living longer with a range of such conditions. Projected Persons living with Long Term Health Conditions in Western Isles 2008-31 CHD COPD Asthma Diabetes Dementia All selected LTCs 2008 1136 567 1337 1128 509 4676 2031 1510 724 1298 1365 839 5735 % change 32.81 27.72 -2.88 20.98 64.85 22.65 The impacts on healthcare delivery from such increasing prevalence levels among our ageing population based on current models of delivery are seen in the large rises in unscheduled hospital care for the elderly. In past 10 years the Western Isles has seen the highest increase of such admissions to hospital among its elderly population (see chart below). Such rates of emergency admissions will increase further with pressures described above from our ageing population. Alternative healthcare approaches are key to slowing down this unsustainable trend and are very much the focus of much of the work of the both the health and social services designed to intervene earlier in a person’s health problem so anticipating and avoiding acute crises that result in hospital admissions. Page 12 of 28 Ageing population and healthcare impacts – emergency care % change in Rate of Emergency Hospital Admissions for persons 65+, 200/01 to 2009/10 35% 30% 25% 20% 15% 10% 5% he t la nd B or Fo d e rth rs V al D l um G ey ra fri m es & pia n G al lo w a H y ig hl an d Ta y A si ll de S co Lo tti sh th ia R es n G re id en at er ts G la sg ow Fif e & C La lyd e n A yr ark sh s ire h ir e & A rr an O rk W e s ne y te rn Is le s 0% S -5% -10% -15% Page 13 of 28 4. The organization of the health care services in the Western Isles Organization of the health care services • • Primary health care – 10 Practices all run by independent contractors working to a national contract with some local contractual elements related to local issues. 3 Hospital sites – 3 sites. – 1 Rural General Hospital – 2 Community Hospital x2 4.1 Primary Healthcare There are 10 GP practices run by independent contractors working to a national contract (with 36 (headcount) General Practitioners) throughout the Western Isles providing primary care services to the community. A number of GPs provide additional support in specialist areas such as Dermatology, Cardiology, Learning Disabilities, Child Protection, Public Health, Anaesthetics, General Surgery and Paediatric services, in partnership with the Western Isles Hospitals. The GPs and their staff work closely with a range of community health staff such as district nurses, community midwives, health visitors, Allied Health Professionals (Physiotherapy, Speech & Language Therapy, Occupational Therapy, Dietetics and Podiatry), community mental health services and health promotion services. Community based dental services are also provided across the islands Page 14 of 28 4.2 Hospitals / Specialised service NHS Western Isles NHS has 3 Hospitals. Western Isles Hospital, a Rural General Hospital, is located in Stornoway. It was opened in 1992 with a range of hospital acute specialities, psychiatry and care of the elderly. Consultants (17) – Medicine, Surgery, Orthopaedics, Anaesthetics, Paediatrics, Obstetrics and Gynaecology, Psychiatry, Radiology. Some consultant led services are provided in the Western Isles hospital by consultants based in mainland hospitals. The hospital also includes diagnostic facilities, day hospital, laboratory and Allied Health Professionals and other service. Delivering for Remote and Rural Healthcare (SG, 20085) provides models for staffing, education, transport and emergency care for remote and rural areas as well as designating the Western Isles Hospital (WIH) as one of 6 Rural General Hospitals (RGH) in Scotland. Each RGH will offer, as a minimum, the core services of medicine, general surgery and anaesthetics. The provision of other services over and above those minimum core services are dependent on local circumstances and health needs of the population. The Uist & Barra Hospital, a Community Hospital run by general practitioners, is located in Benbecula; it was opened in 2001. It provides a local service for the population of the Southern Isles (North and South Uist, Benbecula, Barra, Berneray, Grimsay, Eriskay, Vatersay and Baleshare. The Hospital has 29 beds, and provides care of the elderly, respite care, GP acute care and midwifery led maternity services. Many of the Consultants from the Western Isles Hospital, and some from mainland Health Boards, visit the Uist & Barra Hospital to provide outpatient services. St Brendan’s Hospital, a Community Hospital with 5 acute beds, is located in Castlebay on the Isle of Barra and is in a shared building with the Local Authority Residential facility. It is supported by the local GP Practice to provide care of the elderly and other services. 5 The Scottish Government, Edinburgh 2008. Delivering for Remote and Rural Healthcare. The final Report of the Remote and Rural Workstream. Page 15 of 28 Orthopaedics Lewis Surgery Medicine Psychiatry Obs & Gynae Paediatrics Harris . Stornoway Oncology Respiratory Medicine Gastroenterology Urology Ophthalmology ENT North Uist . Inverness Additional pathways . Stroke Thrombolysis South Uist Aberdeen Barra Paediatrics Psychology Diabetes Plastic Surgery Neurology . Glasgow Cardiology Orthopaedics MRI Western Isles Clinical Pathways Dundee Edinburgh . CAMHS Assisted Conception . Radiology Obligate Network NHS Western Isles has external agreements with other Health Boards, primarily Highland Health Board and Greater Glasgow and Clyde Health Board, for the provision of care to Western Isles residents. This includes services such as Ear Nose & Throat (ENT) Surgery, Dermatology, Respiratory Medicine, Child Psychiatry, Rheumatology, specialised Paediatrics, Ophthalmology, Oral Surgery, Neurology, Oncology and Urology. Referral pathways for other spcialities are with other NHS Scotland Health Boards - for example Child and Adolescent Mental Health Services and Assisted conception with NHS Tyside and Stroke Thrombolysis with NHS Grampian. NHS Western Isles works closely with a range of other statutory bodies (e.g. Comhairle nan Eilean Siar (CNES), NHS 24, the Scottish Ambulance Service) and voluntary sector services to ensure the best possible health care service for the Western Isles population. Page 16 of 28 5 Health Care Professionals Sept 2011: Headcount 1050 (Including General Practitioners (1086) WTE 838.71 Staff in Post - WTE (30th Sept 2011) Staff Group Staff in Post at Aug 2011 (wte) Medical (not including GPs) 21.56 Dental 17.45 Medical & Dental Support 46.20 Med & Dental Total 85.21 Nursing & Midwifery (Band 1 -4) 81.38 Nursing & Midwifery (Band 5+) 269.55 Nursing & Midwifery Total (wte) 350.93 AHP (Band 1-4) 16.31 AHP (Band 5+) 50.82 AHP Total 67.13 Other Therapeutic Service 9.78 Personal & Social Care 17.31 WIHB - Employments by Job Admin Services Family AHP 2% 1% 16% 18% 1% Healthcare Science Med & Dental 7% 1% 44% 5% 5% Med & Dental Supp Nur & Mid Health Science Services 11.77 Support Services 119.44 Admin Services 166.14 Management (Non AFC) 11.00 Other Total 335.44 Band Not AFC 8c Administrative Services 8b Allied Health Profession 8a Health Science Services 7 Medical & Dental 6 Medical and Dental Support 5 Nursing and Midwifery 4 Other Therapeutic 3 2 1 TOTAL Page 17 of 28 838.71 Personal and Social Care Senior Managers Support Services WIHB Staff by Age Group 200 180 160 140 120 100 80 60 40 20 0 11.45 9.25 8.70 4.44 18.18 8.27 1.90 30.77 10.53 5.36 SUPPORT SERVICES OTHER THERAPEUTIC MEDICAL AND DENTAL ADMINISTRATIVE SERVICES 0 20 40 78.43 60 80 100 Turnover rate: (including medical trainees - 11.45%.Without medical trainees 6%.) N.B. Small numbers of staff can give a “false” picture – i.e. Healthcare Science – 30.77% = 1 leaver and one new start. Page 18 of 28 6. Urban comparison area The Urban area for comparison will be the city of Aberdeen. Aberdeenshire is one of the 32 unitary council areas in Scotland. Aberdeenshire council area does not include the City of Aberdeen, now a separate council area, from which its name derives. Grampian was a local government region of Scotland from 1975 to 1996. It is now divided into the unitary council areas of: Moray, Aberdeenshire and the City of Aberdeen. Grampian continues to have a joint police service, fire service, and electoral, valuation, and Health boards. Aberdeen City is the 3rd largest and one of the most densely populated cities in Scotland, with a population density of 1,151 persons/sq km. Population density within Aberdeenshire sits at 36 persons/sq km with approximately 63% of the population living in the main towns. This reflects the rural nature of the region. Page 19 of 28 6.1 Demography The estimated population for Grampian 2009 was 544,980, an increase of 1% from 539,630 in 2008. The population of Grampian accounts for 10.4% of the total population of Scotland. The population currently has a relatively high proportion of under 20s and fewer over-65s compared with the Scottish average, reflecting employment-driven in-migration in recent decades. Area 2008 2009 % Change Scotland 5,168,500 5,194,000 0.49% Grampian 539,630 544,980 0.99% Aberdeen City 210,400 213,810 1.62% Population Projections 2008 to 2033 By 2033 the population of Grampian is projected to be 605,307, an increase of 12.71% compared to 2008. The population of Scotland is projected to increase by 7.27% between 2008 and 2033. Area 2008 2033 % Change Scotland 5,168,500 5,544,410 7.27% Grampian 539,630 605,307 12.17% Aberdeen City 210,400 219,630 4.39% Page 20 of 28 6.2 Health care services NHS services for the Grampian region are provided by NHS Grampian, and are overseen by one single NHS Board. NHS Grampian covers an area of over 3,000 square miles of city, town, village and rural communities. The Board is supported from headquarters at Summerfield House in Aberdeen. Senior managers for the functions which cover the whole of Grampian are based here, including financial overview, corporate planning, and central responsibility for protection and promotion of public health. NHS Grampian consists of acute services, corporate services and three Community Health Partnerships (CHP) and works closely with the local authorities. NHS Grampian is also very closely linked with both the University of Aberdeen and The Robert Gordon University, especially in the fields of research, workforce planning and training. Care is provided throughout Grampian in 9 main hospitals, a 17 community hospitals, 84 GP Practices and various other specialist care units. 6.2.1 Hospitals: Aberdeen Royal Infirmary is NHS Grampian's largest hospital, situated at Foresterhill, Aberdeen. Royal Aberdeen Children's Hospital and Aberdeen Maternity Hospital are also housed at the Foresterhill site. Woodend Hospital caters for many patients, including the elderly. Royal Cornhill Hospital provides inpatient and community support for mental health services. A large number of outpatients are seen at the Woolmanhill Hospital in the city centre. Roxburghe House is a new purpose-built unit providing palliative care for terminally ill patients. Dr Gray's Hospital is the district general hospital based in Elgin, Moray. Children with special needs are cared for at the Raeden Centre jointly with Aberdeen City Council. The Oaks is a another purpose-built unit which provides specialist care and support for people with cancer and other progressive illnesses in Moray. 6.2.2 Community Hospitals: Community hospitals are hospitals where most patients are admitted, and cared for, by their own GPs. They normally deal with : Acute medical care where patients cannot be cared for at home, but where the expertise and / or the specialist diagnostic facilities of a major specialist hospital are not required. Post acute care including rehabilitation. Casualty services. Palliative care. They may also have : Page 21 of 28 Diagnostic facilities (such as x-ray, ultrasound, sigmoidoscopy, cardiac assessment, telemedicine). Therapeutic facilities (such as physiotherapy, occupational therapy, minor surgery, day hospital). Facilities for joint teams (such as community nursing teams and social work / care management teams). Specialist out patient clinics. Intermediate care clinics. Hospitals often share expertise and equipment and offer services to patients not normally in their area. 6.2.3 Community Health Partnerships: CHPs are co-terminous with council areas and represent a district or area within the region. A CHP manages a wide range of community based health services and, in partnership with local councils, provides a focus for the integration between primary care, specialist services and with social care to ensure that local population health improvement is placed at the heart of service planning and delivery. The CHP is responsible for many services already delivered jointly by health and social work staff including: older people, learning disability, mental health and drug and alcohol services. The CHP also works closely with local GPs, pharmacists, dentists, opticians and specialist staff from local hospitals. Page 22 of 28 6.3 NHS Grampian Staffing NHS Grampian Current Staffing (wte) Total 10885.20 Administrative Services 1726.20 Nursing/Midwifery 4967.50 Allied Health Profession 874.80 Other Therapeutic 291.20 Healthcare Sciences 438.40 Personal and Social Care 77.90 Medical and Dental 627.60 Senior Managers 127.20 Medical and Dental Support 203.60 Support Services 1550.80 Note: the above Medical and Dental figure excludes training grades and GP sessional The following Table is a breakdown of Medical and Dental Staff. (headcount) Total 1330 Associate Specialist 48 Career Start GP 11 Clinical Director 3 Asst Clinical Director 1 Consultant 447 Dental Officer 36 Dental Trainee 6 FTSTA 15 FY1 108 FY2 105 Limited Specialist 1 Medical Director 1 Para 94 9 Salaried 2C GP 40 Salaried GP 4 Salaried OoH GP 23 Senior Dental Officer 13 Salaried GDP 11 SHO 5 Specialty Doctor 51 SPR 63 Staff Grade 4 STR 275 STRCT 50 In addition to the above there are approximately 123 GPs carrying out sessional work within Community Hospitals. Page 23 of 28 7 Education and Training 7.1 Medical Education Undergraduate medical training is the responsibility of Universities throughout Scotland. Workforce planning for intake numbers to University is the responsibility of the Scottish Government Health Department, informed by local NHS Board workforce planning. NHS Education for Scotland (NES) are responsible for the design, development, commissioning and Provision of post graduate medical training in Scotland. The delivery of postgraduate medical training requires a partnership approach between Deaneries, NES and local Health Boards. The quality of the training is overseen by the General Medical Council (GMC). There are four Deaneries in Scotland – the North Deanery is responsible for 5 Health Boards: Western Isles, Orkney, Shetland, Grampian and Highland. All North of Scotland Deanery Foundation Programmes (134 posts) offer as a minimum 4 months in a remote or rural placement, Aberdeen-based with a placement in one of the 6 Rural General Hospitals (RGHs). NHS Western Isles works with the North Deanery and is a Local Education provider – offering training placements across all specialities for doctors in Foundation years (FY) one and two and Specialist Trainees (ST). Modernising Medical Careers (MMC) and the new junior doctor appointments process, UK MMC Career Framework, effective from 01 August 2007, have resulted in delays in matching junior doctors to training positions and have left boards with unfilled posts. This appears to have had a disproportionately large effect on remote and rural and island Health Boards. 7.2 Nurse Education Stirling University Campus is sited within NHS Western Isles Hospital. The University delivers pre and post registration nurse training. Members of staff from Stirling University have honorary contracts with NHS Western Isles and NHS Western Isles staff have honorary contracts with Stirling University. The funding for nursing and midwifery students comes from the Scottish Government's Health budget. The NHS commissions the number of nursing and midwifery students using mechanisms calculated to meet the healthcare sector's workforce requirements for the future. At present the non means tested bursary is £6578 p.a. On average the NHS Western Isles campus recruits 17-20 undergraduate nursing students p.a. Recruitment comes mainly from the local area, with applications received from: school leavers, Further Education and Higher Education graduates, mature students, those who have completed Access courses, from those who are revising their career aspirations and re-joining the workforce. 6.3 Other Education Other types of health care education can be studied across Scotland and the United Kingdom; placements for students are available in many of the Allied Health Professions in NHS Western Isles. Most of the health care professionals are trained at a university level. Most university studies take minimum 4 years at Bachelor level. Page 24 of 28 8 Vulnerability and sustainability of services: 8.1 Medical The Board faces significant recruitment challenges in Medical training grades and succession planning of some trained medical and surgical posts. A number of initiatives are being developed via key work streams of the Acute Strategic Planning group – particularly in relation to Paediatrics, Orthopaedics, and Obstetrics and Gynaecology. Work is ongoing in conjunction with the North of Scotland Planning group (NoSPG), the Remote and Rural Implementation group (RRIG) and the Remote and Rural Healthcare Alliance (RRHEAL) to look specifically at medium to long term workforce needs and solutions. and with other Health Boards via the development of Service Level Agreements and Obligate networks. Specific examples where recruitment has proved challenging for NHS Western Isles include; 2009. Failure to attract a single applicant to interview or a Consultant Surgeon vacancy. 2010. Failure to attract a single candidate to interview for a Consultant Physician vacancy. 2011. Three vacant posts for Junior Doctors in training. Despite repeated advertisements, only one of these posts is currently filled. Variable quality and suitability of locum doctors; as the health care environment – covering multiple specialties in very small teams – is unfamiliar to many doctors whose experience has been previously in large teaching centers. This has meant that even though the doctors have the necessary skills and competencies on paper, they often find it challenging to adapt quickly to the local situation and require a significant amount of additional support and supervision, and have, on a number of occasions, decided to leave before the conclusion of their contracted period. Vacancies for Island GPs requiring repeated adverts, and successful applicants leaving after a relatively short period. Retention of some key staff has been problematic for non professional (family) reasons. 8.2 Pharmacy There have been problems recruiting to registered/qualified Pharmacy posts from November 2000; some current vacancies having been vacant since March 2007, filled by successive locums. Difficulties include distance to mainland centres, cost of travel, and perceived isolation both socially and professionally; this coupled with the national shortage of specialised clinical pharmacists has placed us at a disadvantage when recruiting to these posts. Various approaches have been used to fill these posts including reviewing and re-grading of posts and development of the service to improve the skill mix within the department Locums have been used for long periods, but these are also becoming increasingly difficult to obtain. Community Pharmacy can and do offer more lucrative packages for newly and recently qualified staff than NHS are able to offer which causes additional difficulties in attracting staff to these posts. These packages are not always just financial but also provision of accommodation has also been used to attract staff. If newly qualified pharmacists want to work in Secondary care and are willing to move around the country etc to gain valuable clinical experience then locum opportunities are many and varied, the locum gets paid more with little or no responsibility to the employing organisation. Page 25 of 28 8.3 Other NHS Western Isles experiences recruitment difficulties/challenges across a number of health care staff involved in both direct and indirect patient care, particularly in the more remote and rural areas. For example – recruitment of nursing staff in Lewis and the Western Isles hospital does not present a problem – but, in Uist and Barra recruitment to nursing and Health Care Assistant posts can be a challenge. Recruitment and retention of Domestic Assistants and other support staff is a challenge in the smaller remote hospitals and clinics. Page 26 of 28 Appendix: 1 JOB FAMILIES & SUB JOB FAMILIES (NHS Scotland) (red – employed by NHS Western Isles) JOB FAMILIES Allied Health Professions SUB JOB FAMILIES Dietetics Occupational Therapy Orthotists Podiatry Physiotherapy Radiography Speech & Language Therapy AHP Training/Administration Administrative Services Finance Human Resources Office Services Patient Services Information Systems/Technology Health Science Services Clinical Sciences Biomedical Sciences Clinical Technology Medical & Dental Support Theatre Services Dental Nursing Dental Technology Oral Health Physicians Assistant Nursing & Midwifery Bank Nursing General (Acute) Nursing Care of the Elderly Nursing Paediatric Nursing Mental Health Nursing Learning Disabilities Nursing Midwifery Community General Nursing NHS24 Nursing Nurse Training / Administration/ Management Public Health Nursing Treatment Room/Practice Nursing Other Therapeutic Optometry Pharmacy Page 27 of 28 Play Specialists Genetic counselling Personal & Social Care Health Promotion Hospital Chaplaincy Social Work Support Services Hotel Services Sterile Services General Services Estates Portering Services Stores Services Page 28 of 28