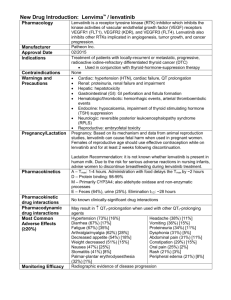
PHARMACOTHERAPY IN METASTATIC THYROID CANCER
PHARMACOTHERAPY IN
METASTATIC THYROID
CANCER
VOICHI ŢA MOGOŞ
Differentiated thyroid cancers may be among the most effectively treated malignancies in patients present with disease localized in the thyroid bed. In this stage the disease may be cured or contained indefinitely with surgery combined with radioiodine thyroid remnants ablation where indicated.
10 % of thyroid cancer patients either present with advanced disease or later have recurrences after primary therapy.
Advanced thyroid cancer is defined as:
Presence of distant metastases not including cervical lymph node metastases
Recurrent locally invasive disease of the neck
According to American Association Joint Committee on Cancer
Classification advanced thyroid cancer includes:
• Stage IV disease
• Stage II disease (distant metastases) in patients older than 45 years .
• Any occurrence of anaplastic thyroid cancer is also considered a advanced disease because of its extremely poor prognosis even after aggressive surgical resection
70
60
50
40
30
20
10 papillary follicular mixeddif/anaplastic anaplastic medullary
0 nodule nodule /lymph node multinodular multi/lymph node s lung me ta bone me ta
Clinic of Endocrinology – Iasi: 326 cases of thyroid cancer – clinical data at presentation
Most important sites of metastases in DTC
• lung - 45 %** - 49 %*
• bone only- 24%*- 39 %**
• other single sites – 4 %**- 8%*
• multiple sites – 12 %**- 19 %* papillary cancer in 51 % of cases follicular cancers in 49 % of cases
Clinical symptoms in patients with metastases from DTC
(differentiated thyroid cancer) may be present especially from bone metastases: swelling, pain , fractures (80 %)
Hag M., Harmer C.: Clin.Endocrinol.(Oxf), 2005, v.63, nr.1, pp: 87-93
Samson E., Brieley J., Le LW., Rotstein L., Thang RW.Cancer 2007, v.110, nr.7, pp: 1451-1456
Prognostic factors in patients with metastastatic DTC at the time of diagnosis
• age 100 % survival before 45 years and 62 % survival after 45 years
• site of metastases : bone metastases or brain metastases are of worse prognosis
• histology : papillary – 75 %, follicular – 62 %
• iodine avidity of metastases : iodine avid – 82 %, non iodine avid – 57 %
• 3 years actuarial survival - 69 %
• 5 year actuarial survival - 50 %
• 5 year disease - free patients - 16 %
• 71 % of death are produced by disease progression
120
100
80
60
40
20
0
0 5 years 10 years 15 years
StageI
Stage II
Stage III
Stage IV
Treatment of advanced DTC
Patients with advanced thyroid cancer have a few therapeutic options for effective disease control
• 131 I therapy is the mainstay of initial therapy for advanced differentiated thyroid cancer . Unfortunetely the metastatic disease is frequntly unresponsive either primary or secondarily to radioiodine therapy.
• Other modalities:
• aggressive surgery
• external beam irradiation
• gamma knife radiosurgery may be useful in selected patients especcialy in respect to symptom palliation
• chemotherapy
Morris JC., Bible KC., Smallridge RC.: Clinical trials for advanced thyroid cancer. Mayo Clinic Endocrinology
Update 2007,www.mayoclinic.org/endocrinology
Pacini F., Schlumberger M et al. Eur.J.Endocrinol. 2006, v.2, 154- 203
Samson E., Brieley J., Le LW., Rotstein L., Thang RW.Cancer 2007, v.110, nr.7, pp: 1451-1456
DTC – lung metastases
• In the case of radioiodine uptake treatment consists of 131 I administration after prolonged suppressive T4 therapy withdrawal or rhTSH
• 131 I activity ranges from 1.7 to 7.4 MBq or higher every 4-8 month in the first 2 years and thereafter at longer intervals.
• WBS will be performed 2-5 days after iodine administration in order to assess the response to treatment toghether with thyroglobulin monitoring, thus quiding further treatment.
• WBS is not required before treatment because it does not modifie indication for treatment and may induce stunning effect (reduction of uptake of the subsequrnt therapeutic iodine dose).
• There is no maximum cumulative dose of radioiodine that can be given in patints with persistent disease. However most remissions are obtained with an activity equal or lower that 22 GBq (600 mCi
• Litium may be useful as an adjuvant therapy of metastatic DTC increasing accumulation and retention of radioiodine in the lesion.
Pacini F., Schlumberger M et al. Eur.J.Endocrinol. 2006, v.2, 154- 203
DTC – bone metastases
• Bone metastases may be treated with a combination of surgery and 131 I.
• When 131 I is taken in the metastases 100-150 mCi of
131 I every 4-6 month, the effectiveness of higher doses remaind to be demonstrated. The success of the therapy depends of the effective half-life of radioiodine in the tumor.
• Other therapies for bone metastases include: external beam iradiation, bisphosphonates, embolisation and cement injections.
• Palliative surgery for bone metastases when there are neurological or ortopedic complications is usefull to debulk large tumors anf may be curative in patients with a single of a few bone metastases
Pacini F., Schlumberger M et al. Eur.J.Endocrinol. 2006, v.2, 154- 203
DTC brain matastases
Brain matastases are rare .
• When possible they will be resected and if non iodine avid or non resecatable external beam irradiation may provide palliation. Usually they carry a worse prognosis, having a mean post treatment survival of around 12 months.
Thyrotropin suppressive therapy
Rationale and recommendations for THS suppressive therapy:
• to inhibit THS –dependent growth of thryroid cancer cells by decreasing TSH levels to less than 0.1 mIU/L
• TSH suppressve therapy is manditory in patients with persistent disease including those with detectable levels of thyroglobulin and no signs or symptoms and in high risk patients for 3-5 years.
• Adverse events of THS suppressive therapy: thyrotixicosis and bone loss
Human Recombinant TSH for diagnostic and therapeutic purposes in DTC
Protocol for hr TSH adminsitration prior diagnostic or therapeutic
131 Iodine administration
• 0.9 mg hrTSH day 1 and 2
• 131 Iodine id given day 3
• TG measurements in days 1-3-5
• WBS in day 5
Adverse effects of hrTSH:
• nausea
• fatique
• headache
• No toxicity and antibodies directed against hrTSH have been seen.
hrTSH provides a stimulation of tumor cells as good as T4 withdrawal.
131 I
WBS
Duntas LH et all. Hormones 2003, 2(3), 169-174
hrTSH
• preserves quality of live of patients avoiding prologend hypothyroidism
• decreases morbidity associated with prolonged thyroid hormones withdrawal
• it is indicated in patients unable to rise endogenous TSH and in those in whom prolonged withdrawal is contraindicated
• in patients with spine metastases and spinal cord compression a short course of high dose corticoisteroids will avoid worsening of neurological symptoms
• hrTSH is particularly suitable in advanced reccurent or metastatic DTC, and in patients who are intolerant to
TSH stimulation by L4 withdrawal
Stategies to enhance 131 I uptake and retainment into
DTC neoplastic cells
Litium therapy : 300 mg 3 times per day or 10 mg/kg.bw
Redifferentiation in iodide non –avid DTC
– Retionoids are derivatives of vitamin A(retinol) that increase NIS mRNA expression and iodide uptake in thyroid cancer line cell. They bind to RXR retinoid nuclear receptor that regulates cell growth and differentiation. In clinical trial retionoic acids reestablish iodide transport in 20-50 % of cases. Recommended doses are of 1-1.5 mg/ kg / day of isotretinoin or 300 mg per day bexarothene prior to 131 I uptake
– Histone dyacethylase inhibitors indice through a unclear mechanism cell cycle arrest and dedifferentiation. Thay reestablish NIS expression,
Tg mRNA and iodide accumulation
– Valproic acid inhibits histone dyacetylase
– Gene therapy is directed to introduce NIS code into less differentiated thyroid carcinoma cells by using a viral vector carrying the gene
Chemotherapy
Classic chemotherapy has a little or no role in the management of advanced differentiated thyroid cancer. I is restricted to patients with progressive disease, uncontrolled by surgery and 131 iodine therapy.
• Studies with chemotherapy in radioresistant DTC are limited.
• Single agent doxorubicin or a combination of doxoribicin and cysplatin provide a 10-20 % partial and transient response without impact on prolonged survival in patients with metastatic DTC..
Recommanded doses of doxorubicin are 60-70 mg/m 2 every 3 weeks.
Cysplatin and epirubicyn is another possible chemotherapy regimen
• Combined chemotherapy using carboplatin and epirubicin under
THS endogenous or exogenous stimulation demonstrated a rate of complete and partial response of 37 %.
• Anthracycline may be indicated in patients wit bone nonfunctioning metastases with progressive disease.
Novel therapies and clinical trials for DTC
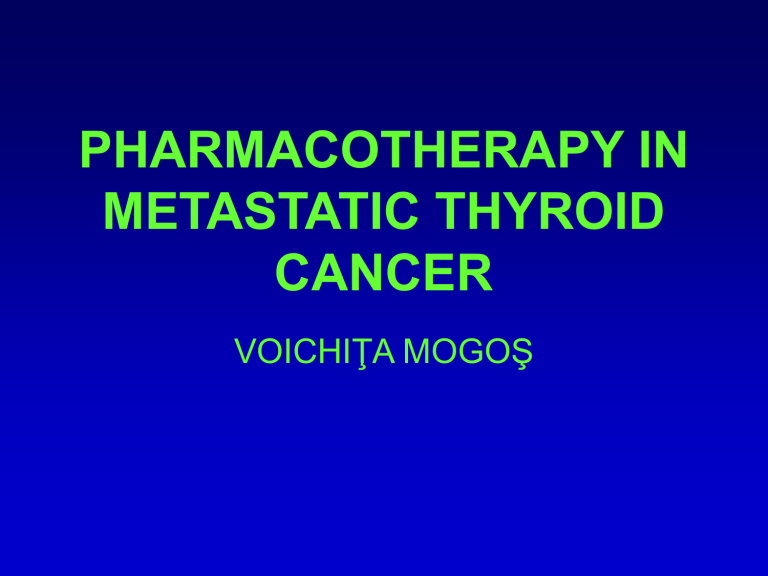
Target therapy is a new generation of anticancer treatment which planned to interfere with specific molecular targets, tipically a protein that is believed to play a crucial role in tumor growth and progression.
Tumor progression is associated with more aggressive behavior, metastatoc spread, loss of iodine uptake ability that makes tumor resistant to conventional therapies .
1. Oncogene inhibitors
2. Angiogenesis inhibitors
3.
Modulators of growth or apoptosis
Cooper DS, Doherty GM et all. Thyroid, 2006, 16, 2, pp 4-22
Coelho SM et all. Arq.Bras.Endocrinol.Metab.2007, 51, 4, 612-624
Coelho Sm et al. Arq.Bras.Endocrinol.Metab.2007, 51, 4, 612-624
Jan Willem B. de Groot, Thera P. Links, John T. M.
Plukker, Cornelis J. M. Lips and Robert M. W.
Hofstra: RET as a Diagnostic and Therapeutic Target in Sporadic and Hereditary Endocrine Tumors
Endocrine Reviews 27 (5): 535-560
Strategies to inhibit RET. The different steps involved in RET activation, regulation, and synthesis are schematically depicted. Each step is associated with a potential means of inhibition for therapy.
1, Ligand binding and formation of ligand-GFR complex (antagonists, antibodies);
2, receptor dimerization (inhibitors);
3, autophosphorylation (tyrosine kinase inhibitors)
4, recruitment of adaptor proteins
(phosphatases, inhibitors of proteinprotein interaction)
5, intracellular signaling (various inhibitors)
6, internalization and nuclear translocation (antibodies, inhibitors); and
7, biosynthesis (gene therapy, RNAi).
ONCOGENE INHIBITORS
RET tyrosine kinase inhibitors in DTC
• YD6474 – Zactima acts as antiangiogenic,
RET blocking agent and inhibits EGFR
(tested in PTC cell lines)
• Pyrazolopyridines PP1 and PP2
• indolocarbazole derivatives inhibit RET in
MTC cell lines
• Sorafenib (BAY 43-9006) multikinase inhibitor inhibitsd RET/PTC autophosphorilation
BRAF inhibitors
• BRAF kinase belongs to the RAF family of serine/threonine kinases ( BRAF – MAPK
– ERK pathway) 36-69 % of PTC carry a point BRAF mutation.
• Sorafenib was tested in advanceed PTC and anaplastic thyroid cancer
• Antisense nucleotides designed to inhibit
C-RAF ISIS 5132 (phase I study)
RAS inhibitors
RAS is a GTP-binding protein involved in cell proliferation and survival. Mutations of
RAS have been reported in thyroid cancer
• ISIS as first generation antisense nucleotide
• Farnesyl transferase inhibitors inactivate
RAS
• Tipifarnib, Lonafarnib, Manumicin and paclitaxel
Other oncogene inhibitors
MEK inhibitors
• CI – 1040
• PD 03225901
• ARRY – 142886
NTRK1 incodes for a high afinity receptor for NGF and its interraction with NGF is blocked by CEP – 701
Akt/mTOR (Akt/ mammalian target of rapamicin) acts through IP3 pathway.
- rapamicin ( Sirolimus)
- LY 294002 inhibitor of IP3 pathway was used in MTC cell lines
Angiogenesis inhibitors
Inhibitors of VEGFR
VEGF-R is the most prominent factor involved in tumor angiogenesis and is overexpressed in poorly differentiated and metastatic DTC
• recombinant human monoclonal antibodies against
VEGF reduce angiogenesis
• Semaxanib , Vatalanib and Axitinib (USA clinical trial) are
VEGFR inhibitors and tyrosine kinase inhibitors
• ZD6474 inhitis VEGF, RET oncogene an MEN 2a and 2 b
• Combrestatin is a tubulin –binding protein inhibitor with vascular targeting properties
Inhibitors of EGFR
EGF-R is overexpressed in PTC and associated with poor prognosis It. Acts through RAS-RAF MAPK cascade and
PI3 kinase pathway
• recombinant human monoclonal antibodies agains
EGFR - Mab 4253 was testes in PTC cell lines
• AG1478 is a tyrosine kinase inhibitor taht antogonises
EGF – mediated angiogenesis and local invasion
• Geftinib is a EGFR tyrosine kinase inhibitor in phase II clinical trial for iodine refractary DTC and advanced DTC
• Irressa (ZD1830) is a tyrosine kinase inhibitor that blocks
EGFR
Inhibitors of EGFR
• Thalidomide is an antiangiogenic factor was used in a phase II clinical trial including follicular, insular carcinoma refractory to radioiodine and
MTC with distant metastases. 800 mg tolerated dose induced partial response in 18 % and stable disease in 32 % of cases with a median survavil of 23.8 months for responders and 11 months for non-responders
• Lenalidomide – immunomodulatory, antiangionegesis, clinical trial in USA
Modulators of growth or apoptosis
HSP 90 is a multichaperone protein complex that mediates maturation and stability of different proteins involved in tumorigenesis: BRAF, Akt, CRAF,
Her-2, EGFR, p53. Inhibition of HSP90 lead to degradation of these proteins and interruption of signal transduction that is essential for tumor progression.
HSP 90 inhibitors:
• Geldamicin and ist derivatives 17 AAG and 17 DMAG ( phase I/II clinical trials)
• Macrolide radicicol and its derivative
• Cysplatin
• Novobiocin
Tumor necrosis factor-related apoptosis inducing ligand TRIAL activates apoptosis by acting on its receptors TRIAL R1 and TRIAL R2 ans caspase pathway. TRIAL-induced apoptosis is inhanced by cycloheximide and paclitaxel
Proteazome inactivators
• Bortezomib (USA clinical trial)
Modulators of growth or apoptosis
Tiazolidindione and derivatives
PPAR
is considered a tumor suppressor factor. PAX8/ PPAR
fusion oncogene was seen in follicular carcinoma and supresses wild type PPAR
activity.
• Troglitazone and rosiglitazone (USA clinical trial) inhibit tumor cell growth and upragulate NIS mRNA.
• High afinity PPAR
agonist RS5444 produces growth inhibition in anaplastic thyroid cancer cell lines. PPAR
agonists induce reversion of epidermal/mezenchymal transition which is critical for anaplastic transformation of differentiated thyroid cancer.
They also increase cyclin-dependent apoptosis, increase cyclin-dependent kinase inhibitors P21 and P27, decrese BcL-x expression and decrease caspase 3 and caspase 7 activity.
• Cyclooxigenase 2 inhibitors
• Activation of COX 2 is overexpressed in different malignancies including thyroid carcinoma. A phase II clinical trial with celocoxib failed to prove any rezults in advanced thyroid cancer
Other targeting therapies
Demetilating agents. Reducing aberant metilation of gene promoters that inhibit gene expression and is associated with loss of NIS, failure of 131 I treatmetn and aggressive behavior of DTC may be achieved by:
• 5 azacytidine
• 5 azo 21 deoxycytidine, decitabine (USA clinical trial)
• sodium butirate, phenylbutirate and phenyacetate that act through unknown mecanisms to induce NIS expression and iodine uptake
Coelho SM., Pines Carvalho D., Waisman M.: Arq. Bras. Endocrinol. Metab. 2007, v.51,nr.4, 612-624
Gene therapy
Viral vectors were used to introduce
NIS gene
• Wt (wild type) p53 gene that is critical regulator of cell cycle progression by activation the cascade of events that lead to apoptosis.
• Prodrug suicide gene therapy
• Thymidine kinase gene is introduced within the cells and placed under the control of thyroglobulin gene promoter that is expressed only in thyroid cells. Once activated thymidine kinase is able to react with Ganclyclovir resulting in DNA strand breaks and subsequent cell death.
Treatment of advanced MTC
Classical chemotherpy
• Doxorubicin, bleomicin, caboplatin, cyclophosphamide,
DTIC, epirubicin, etoposide, 5 fluorouracil, methotrexate, streptozitocin, vincrisine, vinsine.
• Combinations of drugs:
• DTIC + 5FU + epirubicin
• DTIC + cyclohosphamide+ vincristine
• Complete response: 3 %
• Partial response : 24 %, no benefit for survival.
• Embolisation of liver metastases is associated with regression of metastases and stabilization of the disease in 60 % of patients
• Somatostatin analoques have not proven efficacy
Immunotherapy
Principles of immunotherapy:
• Stimulation of physiological immune response to tumor antigens
• To stimulate physiologic immune response by transfering dendritic cells able to combating , calcitonin, CEA.
Dendritic cells are known to present antigens and induce immune response.
• To transfer immunostimulatory substances
Vaccination with mature dendritic cells.
It may be used in MTC patients not curecd by surgery. 2 studies performed with this treatment showed radiological response ( tumor reduction by 50 % assesse by Xray) in 1/7 and 4/10 patients, and biological response (reduction of CEA and calcitonin) in 3/7 and 7/10 patients. Hormonal and radiological stabilization of the disease was noticed in 4/7 and 3/10 patients. Treatment has a good tolerability.
Transfer of immunostimulatory substances
• Studies on murine models were performed by introducing IL2 or IL12 into MTC cells by adenoviral vectors (murine model)
Vezzosi D., Bennet A., Caron P.: Ann.Endocrinol.(Paris), 2007, v.68, pp:147-153
Radioimmunotherapy
• Intense expression by MTC cells of CEA allowed the use of anti
CEA antibodies labeled with 131 I to target these cells. 9-30 treated patients were followed 12-121 months. Modereate regression (less than 50 %) was noticed in 7-29 %, and stable tumor in 35-73 %.
• Combined treatment with myelodepressant labeled anti-CEA antibodies coupled with autologous graft of hematopietic cells rezulted in reduction of tumor size in 10 of 12 treated patients.
Vezzosi D., Bennet A., Caron P.: Ann.Endocrinol.(Paris), 2007, v.68, pp:147-153
anti CEA
Ab
131 I or 90 Y
MTC cell
CEA
CEA Ab
131 I labeled haptene
CEA
Ab
Bivalnt antibodies
In labeled haptehe
Treatments targeting RET gene or protein
Germ line RET mutation are found in 95 % of hereditary MTC and 40-70 of sporadic
MTC Ocogenic activity of RET may be inhibited by: dominant negative RET mutants that will create a RET protein without oncogenic activity or thyrosine kinase inhibitors, inhibitors of RET proteinkinase or inhibition of tumorigenic patways upstream of tyrosine kinase
Dominant negative RET mutants
• Adenoviral vectors expressing dominant negative RET mutants have being used in some studies. Their use results in reduced quantity of RET protein at cell surface and reduced oncogenic capacity of RET
Thyrosine kinase inhibitors
• ST 15 71, Imatinib (Glivec) reduces tumor size in animal model but the concentration needed to induce clinical efects in humans seems to be too high.
Recently good rezults have been reported with Imatinib 600 mg per day in 9 patients
• A phase II study combining tyrosine kinase inhibitor Imatinib with chemothrapy
(dacarbazine and capecitabine are now in trials)
• Other potential target agents: erlotinib, sorafenib, vandatinib, irinotecan (clinical trials) , bevacizumab.
•
Other combined therapies associate a RET tyrosine kinase inhibitor (Glivec) with FGFR tyrosine kinase inhibitor
Other alternatives to inhibit RET oncogenic activity
•
Use of riboyzmes (catalitic molecules) directed against mutated RET mRNA
Other treatments
Use of suicide genes
The suicide gene system involves a combination of herpex simplex virus type thymidine kinase and ganciclovir.
Phisiologically, intracellular kinases will convert ganciclovir monophosphate in ganciclovir triphosphate wich in toxic for cells. In animal models the suicide gene therapy was effective in 75 % of cells.
COX 1 and COX 2 inhibitors – indometacin could induce inhibition of tumor growth and calcitonin secretion in mTC cell lines.
Radioiodine therapy following iodine symporter (NIS) gene expression induced by a viral virus.
Vezzosi D., Bennet A., Caron P.: Ann.Endocrinol.(Paris), 2007, v.68, pp:147-153
Treatment of anaplastic thyroid cancer
47 % of cases present with syncronous metasteses at diagnosis
Classic chemotherapy
Japanese Society of Thyroid Surgery
• Cysplatin: 40 mg/m 2 + etopiside: 60 mg/m 2 + etopiside: 100mg/m 2 + peplomicine 5 mg for 3 days preoperatively with GCSF (Ganulocyte
Colony Stimulating Factor to prevent a risky granulocyte decrease).
Survival: 3-11 month ofter treatment
•
Ausperger 9 (1990): Vinblastine, cysplatine, doxorubicine and mitoxantrone.
Survival: 9 % after 1 year
• Schlumberger (1991): chemotherapy as sensitizer for external beam therapy:
• Before 45 years: doxorubicine 60 mg/m 2 and cysplatine 90 mg/m 2
• After 45 years> mitoxantrone 14 mg. 5 complete response with 3 patients survived more than 20 month
• Tezelman (cit.Giufrida 2000): Bleomicine and flurorouracyl 2 hours before each dose of radiotion therapy
• Kebebew E. 2005: hiperfractionated radiotherapy with 100cGy 4 times a day to the dose of 3600 cGy associeted with doxirubicine
• Doxorubicin and paclitaxel
Treatment of anaplastic thyroid cancer
• Proteayome inhibitors : bertozonib alone ore in association with TRIAL
• Inhibitors of VEGFR : Semaxanib and Vatalanib (USA clinical trial) are VEGFR inhibitors and tyrosine kinase inhibitors
• Sorafenib (RAF kinase) USA clinical trial
• Combrestatin (angiogenesis inhibitor) USA clinical trial
Gene therapy adenoviral mediated:
• p 53 tumor suppressor gene: inhibits cell proliferation and restors Tg gene, thyroperoxidase and TSH receptor genes
• cr6/Gadd45 tumor suppressor gene
Conclusions
• Conventional chemotherapeutic agents have shown not substantive activity in differentiated thyroid cancer and MTC
• Researces directed at defining genetic and signaling patways deffects in different cancer types including thyroid cancer improved understanding of the pathogenesis of thyroid cancer and made possible to design and develop of agents that specifically target these deffects and pathways.
Drug/ agent
Tanespimycin
(17 AAG)
Decitabine
Bortezomib
Romidepsin
Rosiglitazone
Irinotecan
Sunitinib
Combrestatin
Sorafenib
Sorafenib
Lenalidomide
Imatinib
Axitinib
Vandatinib
Disease
DTC
ATC
DTC
MTC target
HSP90
DTC
DTC
DNA methylation
Ubiquitinproteasome pathway
MD Anderson Cancer
Centre
Memorial Anderson
Cancer Centre
DTC
DTC
Hystone deacetylase Memorial Sloan
Kettering Cancer
Centre
PPAR
University of
California San
Francisco
MTC Topoisomerase
DTC/MTC Multikinase
Jonh Hopkins University
University of Chicago
ATC Angiogenesis
ATC
MTC
Multikinase
(RAF-kinase)
Multikinase
(RAF – kinase)
Case Western Reserve
University
Case Western Reserve
University
Ohio StateUniversity
DTC
Primary site
Mayo Clinic Rochster and Mayo Clinic
Jacksonville
Immunomodulatory
Angiogenesis
Multikinase
VGFR inhibitor
University of Kentuky
University of Michigan
Multicenter trial
RET protooncogene Mayo Clinic Rochester and Mayo Clinic
Jacksonville www.cancer.gov/search/clinical_trials
Suggestion reading
• Coelho SM., Pines Carvalho D., Waisman M.: New perspective in the treatment of differentiated thyroid cancer. Arq. Bras. Endocrinol.
Metab. 2007, 51 (4), 612-624
•
Cooper DS, Doherty GM., haugen BR., Kloos RT., Lee SL., Mandel SJ.,
Mazzaferri EL., Melver B:; Sherman SI and the American Thyroid
Association Guidelines Taskforce: Management Guidelines for patients with thyroid nodules and differentiated thyroid cancer
Thyroid. 2006. v. 16 (2) , 4-25
• Pacini F., Schlumberger M., Dralle H., Elisei R., Smit WA., Wiersinga W.
And the European Thyroid cancer Task Force: European Consensus for the management of patients with differentiated thyroid cancer of the follicular epitelium Eur. J. Endocrinol. 2006, v.2, pp: 154-203
• Schlumberger M. : Papillary anf follicular thyroid carcinoma, Ann.
Endocrinol. (Paris). 2007, 68, 120-128
• Vezzosi D., Bennet A., Caron P.: Recent advances in treatment of medullary carcinoma Ann.Endocrinol.(Paris), 2007, 68, 147-153