GI Associated Glands What are the 3 classes of functions performed
advertisement
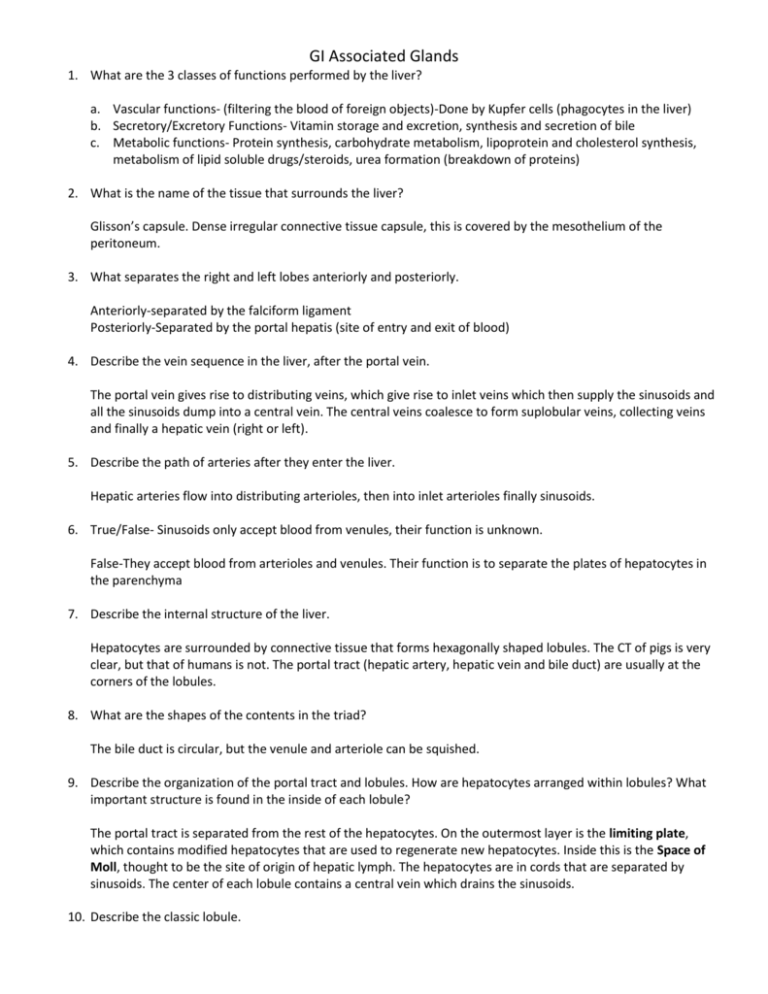
GI Associated Glands 1. What are the 3 classes of functions performed by the liver? a. Vascular functions- (filtering the blood of foreign objects)-Done by Kupfer cells (phagocytes in the liver) b. Secretory/Excretory Functions- Vitamin storage and excretion, synthesis and secretion of bile c. Metabolic functions- Protein synthesis, carbohydrate metabolism, lipoprotein and cholesterol synthesis, metabolism of lipid soluble drugs/steroids, urea formation (breakdown of proteins) 2. What is the name of the tissue that surrounds the liver? Glisson’s capsule. Dense irregular connective tissue capsule, this is covered by the mesothelium of the peritoneum. 3. What separates the right and left lobes anteriorly and posteriorly. Anteriorly-separated by the falciform ligament Posteriorly-Separated by the portal hepatis (site of entry and exit of blood) 4. Describe the vein sequence in the liver, after the portal vein. The portal vein gives rise to distributing veins, which give rise to inlet veins which then supply the sinusoids and all the sinusoids dump into a central vein. The central veins coalesce to form suplobular veins, collecting veins and finally a hepatic vein (right or left). 5. Describe the path of arteries after they enter the liver. Hepatic arteries flow into distributing arterioles, then into inlet arterioles finally sinusoids. 6. True/False- Sinusoids only accept blood from venules, their function is unknown. False-They accept blood from arterioles and venules. Their function is to separate the plates of hepatocytes in the parenchyma 7. Describe the internal structure of the liver. Hepatocytes are surrounded by connective tissue that forms hexagonally shaped lobules. The CT of pigs is very clear, but that of humans is not. The portal tract (hepatic artery, hepatic vein and bile duct) are usually at the corners of the lobules. 8. What are the shapes of the contents in the triad? The bile duct is circular, but the venule and arteriole can be squished. 9. Describe the organization of the portal tract and lobules. How are hepatocytes arranged within lobules? What important structure is found in the inside of each lobule? The portal tract is separated from the rest of the hepatocytes. On the outermost layer is the limiting plate, which contains modified hepatocytes that are used to regenerate new hepatocytes. Inside this is the Space of Moll, thought to be the site of origin of hepatic lymph. The hepatocytes are in cords that are separated by sinusoids. The center of each lobule contains a central vein which drains the sinusoids. 10. Describe the classic lobule. Organization is based on the connective tissue that surrounds each hepatocyte hexagon. It is bounded by the connective tissue that defines the parenchymal hexagon. There is a central vein in the center and portal tracts on the outside. 11. Describe blood and bile flow through the classic lobule. The blood flows from the portal triad on the outside, then goes to sinusoids which collect at the central vein in the middle of each classic lobule. The central vein then supplies sublobular veins, which supplies a collecting vein that joins either the right or left hepatic vein. Bile flows from the hepatocytes (bile is made in hepatocytes) towards the bile ducts in the portal region. 12. What is the portal lobule? The portal lobule is a form of hepatocyte organization where the bile duct is in the center and the central veins are at the apices. This organization is based upon the flow of bile which flows from the hepatocytes towards the bile ducts located within the portal triad (in the center of the lobule). 13. What is a hepatic portal acinus? This is the form of organization that is most popular now and divides the hepatocytes into the smallest possible functional unit. It is a diamond shape structure, the ends of the long axis are the central veins, while the ends of the short axis are the portal tracts. The meridian (between the tracts) is the preterminal branches of a distributing arteriorle that supplies blood to sinusoids. 14. How are the cells divided in the hepatic portal acinus The cells are divided into zones based upon their distance from the distributing arteriole. a. Zone 1 cells are the ones that are closest to the arteriole and receive the most oxygen and are minimally exposed to waste b. Zone 2 cells receive less oxygen and are more exposed to wastes than zone 1 cells. c. Zone 3 cells receive the least oxygen and are heavily exposed to wastes. They are the cells that are first damaged form liver toxicity due to alcohol and drugs. Liver disease and degeneration first shows up in these cells. The cells are the ones closest to the central veins. 15. What is the general relationship between hepatocytes and sinusoids? Within each lobule, hepatocytes are arranged into thin cords or plates that are separated by endothelialy lined sinusoids. The hepatic plates are a continuous set of cells while the sinusoids are continuous with the central vein. 16. How do hepatocytes interact with sinusoids? What other cells are located in the area? Hepatocytes do not directly contact sinusoids, but instead do it via the Spaces of Disse. These are small spaces that only contain plasma, no blood cells or platelets. The hepatocytes have microvilli that extend into the spaces of Disse. Outside of the sinusoids, there are also perisinusoidal cells of Ito, they are irregular cells with long cytoplasmic processes that concentrate vitamin A, their function is not understood. 17. Describe the endothelium and lumen of sinusoids. The endothelium of sinusoids is made of simple squamous endothelial cells that are discontinuous and lack a basal lamina in some areas. The membrane of endothelial cells is riddled with clusters of small holes known as Sieve Plates. These sieve plates allow for the passage of substances from the sinusoids into the spaces of Disse. Reticular fibers hold the endothelium in place. The lumen of the sinusoids have Kupffer cells which are phagocytes of the liver, they phagocytize damaged RBCs and plasma debris. 18. What are the functions of hepatocytes? Hepatocytes function to metabolize the end products of absorption from the alimentary canal, then they store these products as inclusions, then release them into sinusoids in response to neural or hormonal signals. 19. What are the organelle features of hepatocytes? Describe the special nature of smooth endoplasmic reticulum. a. The nucleus is of variable size, cells can be binucleated b. There are numerous mitochondria c. Abundant RER and free ribosomes d. Prominent Golgi used for molecular packaging e. Numerous peroxisomes, lysosomes and endosomes f. Many lipid droplets (esp. VLDL) that increase after fatty meals. Smooth Endoplasmic Reticulum facts: Responsible for drug metabolism and detoxification. Lumen have a microsomal mixed function oxidase system. Methylation, conjugation, oxidations are the most common reactions that occur, that are performed in hepatocytes. 20. Describe the drug detox system that occurs within hepatocytes. Mainly controlled by cytochrome P 450 enzyme system. Most liver enzymes are inducible and are upregulated when there are more drugs present. The liver represents the first pass for most drugs. Drugs will enter the GI tract, then go to the portal vein and into the liver. Some drugs are completely degraded in the liver through this process and therefore a lot of drug is needed. This effect is called the first pass metabolism. 21. Describe the hepatocyte domains. Describe the hepatocyte membrane composition. a. Lateral domain-domain of hepatocyte that borders other hepatocytes (see next question for more details) b. Sinusoidal doman-domain of hepatocyte that borders the sinusoids. The hepatocyte membrane that abuts the sinusoids has a lot of microvilli that extend into the Space of Disse to increase absorption, they have a lot of Na+/K+ and adenylate cyclase membrane activity 22. What are the spaces formed by the lateral domains? Describe The spaces are called bile canaliculi. These spaces conduct bile between hepatocytes to the bile duct located in the portal triad. These are formed from the hepatocyte membranes alone. Bile does not leak out of the bile canaliculi because there are tight junctions on the rest of the hepatocyte membrane that is not covered by the bile canaliculi. The bile canaliculi are found throughout the hepatocyte membrane and form a branch network which converges into bile ductules (canals of Herring) located in the portal region. The Bile ductules dump into the portal bile ducts and eventually into the left and right hepatic ducts. 23. What is the role of bile in the GI system? How is it transported in the GI system? Bile dilutes and neutralizes acid chyme in the intestines, adjusts intestinal pH in the intestines so that pancreatic enzymes can work, emulsifies fat, helps excrete waste products from the degradation of worn out RBCs and excretion of excess cholesterol synthesized in the liver. Bile is transported from hepatocytes into the bile canaliculi via a series of ATP dependent transporters. Bile is made in the liver, concentrated in the the gall bladder then released in the duodenum 24. What is bile composed of? Bile salts (including taurocholate and glycocholate), bilirubin (yellowinsh-green toxic product of hemoglobin degradation in the spleen) and others such as IgA, electrolytes, cholesterol, phospholipids. 25. How does bile exit the gallbladder? Bile exits through a cystic duct, which combines with the hepatic duct to form a common bile duct that enters into the duodenum. 26. Label the layers of the gall bladder wall A B C E D a. Simple columnar epithelium that is composed of 2 different cell types: clear cells and brush cells. Brush cells are the ones responsible for concentrating bile. b. Lamina propria- composed of vascularized loose connective tissue c. Muscularis Externa- composed of smooth muscle of mixed orientation d. Perimuscular connective tissue e. Thin outer simple squamous epithelium 27. How is bile released from the gallbladder? Bile is released in response to cholecystokynin (CCK) produced by the enteroendecrine cells of the intestinal epithelium. The flow of bile is controlled by the sphincter choledochus, located at the junction of the common bile duct and duodenum. This sphincter is relaxed in response to CCK release, bile enters the duodenum at the Ampulla of Vater. 28. What are gallstones? Gallstones are chunks of cholesterol that build up along the walls of the ducts. If they get stuck in the common bile duct they can obstruct the flow of bile and can be very painful. 29. How is the pancreas divided? The pancreas is divided into lobules by a thin capsule of connective tissue. The connective tissue is called septae. Loose CT from the septae surround each glandular unit as well. 30. What are the functions of the pancreas? Where are they performed? The pancreas has exocrine and endocrine functions. Exocrine is in pancreatic acini, endocrine functions are in the Islets of Langerhans. 31. What makes up the functional unit of the exocrine pancreas? Functional unit of the exocrine pancreas are formed by tubuloacinar glands composed of secretory acinar cells and their accompanying ducts. The entire gland system are called “acini”, they are composed of: a. Acinar cells, forming the secretory component of the pancreas b. Centroacinar cells- form the initial portion of the duct system (located in the middle of the acinar cells), forms intercalated ducts. 32. What is the organization of pancreatic ducts beyond the acini? Intercalated ducts from neighboring acini join to form larger intralobular ducts composed of simple cuboidal columnar cells Intralobular ducts converge to form larger interlobular ducts composed of low columnar epithelium Interlobular ducts empty into the main pancreatic duct which merges with the duodenum 33. What are the 2 regions of acinar cells? a. Basal region- sits on basement membrane that surrounds each acinus. Has a round nucleus, extremely well developed RER in basal aspect and has numerous mitochondria. This part is basophilic b. Apical region- Numerous zymogen granule s that change in number based upon the state of fasting, well developed golgi apparatus, numerous microvilli on the luminal surface, tight junctions exist in between cells. 34. How are enzymes released and activated in the pancreas? How is this process controlled in the pancreas? What happens in pancreatitis? Enzymes are released as precursors, that need to be activated by trypsin in the intestine. The pancreas itself is protected because it releases anti-trypsin enzymes that prevent the pancreatic enzyme from eating away at the pancreas itself. In pancreatitis, inflammation the acinar cells to lyse, releasing pancreatic enzymes into the abdominal cavity and cause organ damage. 35. What are centroacinar cells? What is secreted by these cells? Centroacinar cells are those that are in the intercalated ducts of acini. They are clear staining and are located in the center of acini. Their function is to secrete bicarbonate ions to maintain the duodenal pH so that pancreatic enzymes can function properly. 36. What regulates hormone release from the acinar cells and centroacinar cells? Hormone release from acinar cells is controlled by CCK, which has receptors on acinar cells and is released by the duodenal epithelium. Hormone release from centroacinar cells is controlled by secretin, produced by the duodenal epithelium. 37. What is viral hepatitis? A blood borne infection that leads to inflammation and causes destruction of hepatocytes. It results in fatigue, decreased appetite, weakness, nausea, joint and muscle pain and fibrosis of the liver, treatment is to use antiviral drugs. 38. What is cirrhosis? It is a chronic disease of the liver. It results in fibrosis of the liver following hepatocyte damage. It is associated with alcoholism, chronic hepatitis and bile obstructions. Problem is associated with blood and bile drainage, results in jaundice, portal hypertension, GI bleed, etc. 39. What are Wilson’s Disease and Hemochromatosis? Wilson’s Disease occurs when copper accumulates in the liver. Hemochromatosis is an inherited iron overload disease, symptoms include joint pain, fatigue and abdominal pain. 40. What are common liver function tests? Test for alanine aminotransferases and aspartate aminotransferases (ALT, AST) (increased in liver damage. Bilirubin should increase, plasma albumin decreases and increased blood clotting times. 41. What are the results of liver failure? a. Reduced protein synthesis- Leads to decreased albumin levels and therefore formation of edemas. Reduced formation of clotting factors leads to increased bleeding. b. Reduced metabolic detoxification- Increases plasma levels of biological toxins, leading to hepatic coma c. Decreased bile secretion- Bile accumulates in the liver and plasma manifests as jaundice.