Digestive Tract: Let's Get to the Bottom of it
advertisement
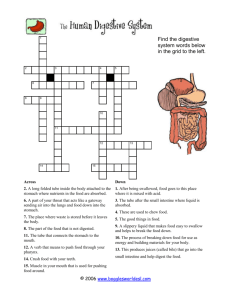
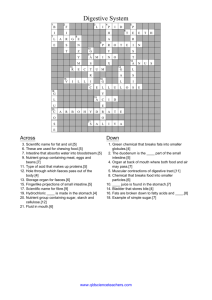
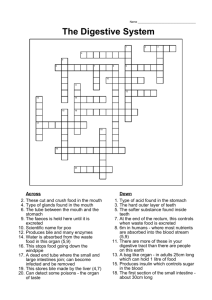
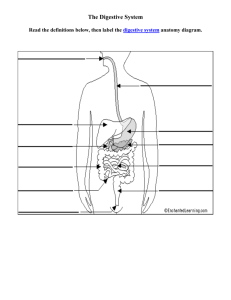
Digestive Tract: Let’s Get to the Bottom of it By: Diana Blum RN MSN Metropolitan Community College Primary Role Extract molecules essential for cellular function from fluids and food. Ingestion, Digestion, Absorption, Elimination Digestion: breakdown of food into simple nutrient molecules that can be used by cells Process requires: 1. 2. 3. http://health.discovery.com/centers/digestive/machine.html Digestive tract Also called ___________tract muscular tube about 30 ft long Main parts Mouth Pharynx Esophagus Stomach Small intestine Large intestine Anus Acessory Organs Salivary glands Liver Gallbladder Pancreas Each of the above accessory organs secrete fluid that contain special enzymes that enable breakdown (metabolism) of food Peritoneum lines the abdominal cavity and covers surface of organs Enables organs to moves without friction during breathing and digestion mouth Teeth cut and grind food Salivary glands secrete saliva Saliva: Amylase: Tongue mixes saliva with food and when small enough- forces the food into the pharynx Pharynx Shared by digestive and respiratory tracts Joins mouth and nasal passages Contains the epiglottis Covers the airway (like a trap door) to prevent food from entering respiratory tract esophagus Long muscular tube that passes through the diaphragm into the stomach Gravity helps move the food but it is not essential Circular, wave like contractions of the muscles propel food down the tract (peristalsis) Stomach Widest section of the GI tract Separated from esophagus by the cardiac sphincter Has 3 sections Unique muscle layers churn food by mixing it with gastric secretions Rennin-starts breakdown of milk proteins Pepsin-partially digests protein HCL acid-partially digests protein Lipase-breaks down fat Chyme: Pyloric sphincter- keeps food in stomach until it is mixed properly Small Intestine Chyme leaves stomach and enters here Chemical digestion and absorption of nutrients take place 20 feet long 3 sections Duodenum-liver and pancreatic enzymes enter here Jejunum Ileum Small Intestine Continued Bile- produced in the liver and stored in the GB break down large fat globs Pancreatic enzymes-reduce the fat to glycerol and fatty acids to be easily absorbed 3 layers of tissue make up the wall Mucous membrane-secretes digestive enzymes Sucrase, lactase, maltase, lipase, etc. (see table 36-1) Inner layer- covered with Villi (microscopic projections). Digestive food molecules are absorbed through the villi into the bloodstream Muscle layers continue to contract moving the chyme into the large intestine. Large Intestine No Villi No digestive enzymes Chyme enters through the ileocecal valve Water is absorbed and remaining waste=feces 5 sections Cecum-1st section..appendix is here Ascending colon-up right abdomen Transverse colon- across abdomen just below waist Descending colon-down the left abdomen Sigmoid colon-the part of the descending colon between iliac crest and rectum Rectum-the last 6-8 inches of the large intestine Anus – where waste leaves the body Age related changes Teeth mechanically worn down Illness causes increased risk for problems with digestion/elimination Gingiva recedes Tooth loss from caries and periodontal disease Loss of taste buds Xerostomia (dry mouth) is common Walls of esophagus and stomach are thinner with lessened secretions HCL Acid and digestive enzyme production decreases Gastric motor activity slows Delayed gastric emptying Hunger contractions diminish In the large intestine- muscle layer and mucosa atrophy Smooth muscle tone and blood flow decreases Connective tissue increases Constipation is frequent More laxative use Nursing Assessment Hx of illness: weight loss, indigestion, change in bowel habit PMH: surgery, trauma, infection, burns, hepatitis, ulcers, cancer, stomas, meds, allergies Fam Hx: diabetes, CA, ETOH, polyps, obesity, ulcers, GB Dx System Review: flatus, dyspepsia (indigestion), skin changes, caries, diff chewing, abd distention, pain, elimination Functional: nutrition, activity, meal times, likes/dislikes, food beliefs Physical exam: mucous membranes, condition of mouth/teeth, abd distention, bowel tones, palpation, percussion, rectum/anus for lesions, color, hemorrhoids diagnostics Imaging/radiographs: NPO, allergy (iodine, dye, shellfish), consent UGI Barium swallow/enema Endoscope Upper Lower Hemmocult-looks for blood NG Salem Sump Tube feedings Assist pt into fowlers to reduce aspiration. Pt remains up at least 30 degree during continuous feeding Check placement for tube in stomach or duodenum prior to use Remains this way for 30 minutes after Air bolus and residual Check to make sure you have the correct formula Stop feeding if nausea or pain Rinse tube with 30 cc fluid after each bolus Administration Remove plunger Pinch tube while inserting syringe to avoid stomach content leak Hold barrel about 12 inches above stomach and allow gravity to infuse Flush after bolus complete GI decompression Ng with suction removes fluid and gas To use Attach to sxn as ordered Generally low, intermittent is used for single tube Low continuous for dual lumen tubes Check patency Irrigate routinely Monitor output Assess for flatus Provide comfort measures Once tube in place- securely tape it to nose feedings TPN Deliver nutrients directly into bloodstream via central line Use sterile technique for dressings and care Monitor flow rate Monitor blood glucose Label lines PPN Same as TPN except goes through peripheral line Anorexia Lack of appetite Causes Nausea Physical/emotional disturbances Environment Decreased sense of smell Tests: weight, physical, hemoglobin, iron, electrolytes, thyroid Nursing diagnosis Imbalanced nutrition less than requirements r/t anorexia Goal: improved appetite and adequate food intake AEB: increase in intake, stable or increased wt Interventions: provide antiemetics prior to meals, remove the bed pan and emesis basin from sight, conceal drains and collection devices, deodorize room clients with Feed problems Paralyzed Confused Severe arthritis CVA Visually impaired Etc FEEDER is demeaning and can threaten self esteem Interventions for feed problem Position properly Specially enhanced utensils Open sealed products Cut meats Butter bread Season food after asking client their preferences See page 751 Role play Practice feeding classmate a simple meal then reverse. The person being fed can not speak but understands what is being said 1.How did it feel to be fed? 2. What steps did you use? 3. How did the feeder feed? 4. What did you learn? Stomatitis Inflammation of the oral mucosa Mechanical trauma (poor fitting dentures) Irritation 2nd to smoke and ETOH Poor hygiene Radiation Drug therapy Treatment: soft bland diet, antiviral agents, antibiotics Vincent’s infection (aka Trench Mouth) Vincent’s infection Caused by bacteria Called trench mouth b/c occurred in WWI field S/S: metallic taste foul breath. Bleeding ulcers, increased saliva, general infection signs, anorexia TX: topical antibiotics, mouthwash, rest, nutritious diet, good oral hygiene Herpes Simplex Herpes Simplex Caused by Herpes simplex virus type 1 S/S: ulcers and vesicles in mouth and on lips Other name is cold sore or fever blister Common with people who have upper respiratory infections, excessive sun exposure, or are stressed TX: Camphor, topical steroids, antiviral agents Aphthous Stomatitis (aka canker sore) Caused by virus S/S: ulcer on lips or mouth that recur at intervals TX:topical or systemic steroids Candidas Albicans AKA yeast like fungus Other names: thrush or candidiasis S/S: bluish white lesions on mucous membrane of mouth Those at risk: steroid users, long term antibiotic users TX: oral medications, topical antifungal agents, vaginal nystatin tablets can be used like lozenges Care and intervention CARE Usually tx outpt Look at pt symptoms Onset of symptoms, meds, radiation, habits, diet, ETOH use, and smoking INTERVENTION Describe pain (location, onset, precipitating factors) Gentle oral hygiene Prescribed mouthwash Use soft bristle tooth brush Instruct to take meds as prescribed (swish and spit, or swish and swallow) Teach flossing techniques Dental Caries Destructive process of tooth decay Caused by plaque Plaque is made from bacteria, saliva, and cells that stick to tooth surface In time if untreated the canal will erode causing intense pain and death of pulp TX: fluoride, good nutrition Gingivitis Beginning of periodontal dx Inflammation of the gums s/s: red inflammed tissue of gums, pain, bleeds easily More frequent in those with missing teeth or whose teeth don’t close properly, vitamin deficiency, anemia Care and Intervention CARE Assess pain and soreness Assess diet and examinations Examine mouth care practices INTERVENTION Minimize pain Gentle mouth care several times a day Teach client proper technique Page 752 Oral Cancer Most life threatening condition of mouth 2 types: Squamous Basal cell S/S: tongue irritation, loose teeth, tongue pain, ulcerations, leukoplakia (hard white spots), decreased appetite, diff swallowing, weight loss, change in denture fit, hemoptysis TX: biopsy, surgery, radiation, chemo Care and Intervention CARE Assess sun exposure, smoking habits, ETOH use, fam hx of oral ca, Interventions Radiation=edema Dry mouth is issue Good hygiene Special rinses see pg 753 Monitor respirations Suction if ordered Stay on top of pain Soft or liquid diet Monitor I/O Use communication board to talk with pt BE PATIENT BE A GOOD LISTENER Monitor for infection If graft: monitor color and temp Parotitis Inflamed parotid glands S/S: painful swelling near low jaw, pain increases with mastication Suseptible: those unable to drink liquids, those weak, no resistance to infection TX: antibiotics, mouthwash, warm compress Complications: gland ruptures, surgical drainage or removal may be necessary Achalasia Progressive worsening dysphagia Low esophageal muscles do not relax Unknown cause TX:dilation, surgery, botulism toxin, isosorbide dinitrate Esphageal cancer Not common Poor prognosis No known cause At risk: smokers, ETOH users, chronic trauma, poor oral hygiene, spicy food eaters S/S: progressive dysphagia, substernal pain, epigastric pain, neck/back pain,sore throats, choking, obstruction, weight loss Esophageal treatment Esophagectomy Esophagogastrostomy Esophagoenterostomy Dilitation of esophagus Stent Laser tx Chemo Radiation Photodynamic therapy See page 756 Interventions Treat pain Daily weight Strict I/O Calorie count Quiet relaxed environment Erect position Chin tuck maneuvers for swallowing Feeding tubes TPN If post op---do not irrigate or reposition Assess pt knowledge Monitor for infection Monitor respirations N/V Nausea: feeling of queasiness Pain, pallor, perspiration, cold, clammy skin Causes: irritating foods, infection, radiation, meds, inner ear disorders, motion sick Vomiting: forceful expulsion of stomach content through the mouth Regurgitation: gentle ejection of fluid or food w/o nausea or retching TACHYCARDIA AND INCREASED SALIVA are common before vomiting Complications: loss of fluid and electrolytes, dehydration, metabolic alkalosis, weakness, aspiration TX: antiemetics, iv fluids, NG tube Interventions: maintain cool room, remove unpleasant stimuli, place in comfortable position, provide emesis basin, cool damp cloth on head/neck, slow deep breaths, offer mouth care after vomiting, clear liquids Hiatal Hernia Protrusion of stomach and and lower esophagus up thru the diaphragm and into chest 2 types: Sliding: gastroesophageal junction is just above the hiatus. Stomach slides when patient reclines (associated with GERD) Rolling: gastroesophageal junction remains in place but a portion of the stomach herniates up throu diaphragm through a 2nd ary opening Complications: ulcerations, bleeding, aspiration Strangulated hernia is one that becomes trapped without blood flow Causes: asymptomatic to fullness, dysphagia, eructation (belching), regurgitation, heartburn TX: meds(antacids, H2 receptor blockers, etc), diet, avoid intra abd pressure, surgery Interventions: stay on top of pain, no food or fluid 23 hours before bed, wooden blocks under top of bed, monitor wt, small frequent meals, avoid fatty foods, caffeine, ETOH, and spicy foods GERD Back flow of gastric content from the stomach into the esophagus Key find: inappropriate relaxation of the low esophagus sphincter Causes: abnormalities in the LES, ulcers, esophageal surgery, prolonged vomiting, gastric intubation S/S: can be sudden or gradual, painful burning that moves up and down (common after meals) resolve after antacids, dysphagia, belching Diagnosis: Based on s/s, raqdiographic studies, endoscopy, bx Tx: H2 receptor blockers (zantac), prokinetic agents (reglan), proton pump inhibitors (prilosec), surgery Gastritis Inflammation of the stomach lining Mucosal barrier that normally protects stomach breaks down H pylori is cause S/S: N/V, anorexia, fullness, pain, hemorrhage Tx: npo until resolve, IVF, Bx, medication,, bland diet, surgery Peptic Ulcer Loss of tissue from digestive lining Caused by pepsin and HCL injure unprotected tissue LOCATION, LOCATION, LOCATION Either gastric or duodenal Causes: drugs, infection, stress. S/S: burning pain, nausea, anorexia, wt loss Complication: hemorrhage, perforation, obstruction, Tx: meds, diet, stress management Drug therapy Used to relieve symptoms Antacids are first line of defense Diet Avoid coffee, tea, meat broth, alcohol, spicy food Frequent small feedings Management NG tube to sxn if hemorrhage suspected Saline lavage after NG procedure on page 769772 Vasopressin may help control hemorrage Table 38-6 discusses surgery tx of peptic ulcer dx Stomach cancer 25,000 dx each year Most common in men, african americans, people over 70, low socioeconomic status S/S: no early signs Late signs: vomiting, ascites, liver enlargement, abd mass 5 yr survival: 10% No known cause Risk factors: pernicious anemia, chronic atrophic gastritis, achlorhydria (lack of HCL), smoking, high salt starch pickled food nitrate diet obesity Excess body fat Causes: heredity, body build, metabolism, psychosocial, caloric intake Complications: heart/lung problems, DM, polycythemia, cholelithiasis, infertility, endometrial cancer, DJD Tx: wt reduction diet, exercise, medication (pg775), surgery, malabsorption 1 or more nutrients not absorbed/digested Causes: bacteria, bile salt and digestive enzyme deficiency, alterations in intestinal mucosa 2 types: Celiac sprue (tropical, nontropical)- genetic, Non-Tropical: changes in mucosa, impaired absorption Tropical: infectious agent Lactose intolerance Inherited or aquired Causes: IBS, gastroenteritis, sprue syndrome S/S: steatorrhea (fatty stools), foul stools, wt loss, decreased libido, easy bruising, edema, anemia, bone pain Tx: diet, meds, elimate gluten for celiac dx Tropical sprue: oral folate, antibx, vit B12 injections Lactose: no milk or milk products, lactase enzyme, monitor vitamin levels diarrhea Loose liquid stools Causes: spoiled foods, allergies, infection, diverticulosis, cancer, malabsorption, impactions, tube feedings, medications S/S:cramps, abd pain, urgency Complications: dehydration, electrolyte imbalance Tx: anti diarrheal drugs, clear liquids vs npo, possible TPN constipation Hard dry infrequent stools Causes: ignoring urge, laxative use, inactivity, inadequate fluid intake, drugs, brain/spinal cord injury, colon diseases, surgery, Tx: laxatives, stool softeners, megacolon Large intestine looses ability to contract to move feces to rectum Pts need regular enemas Fecal impaction Retention of large amount of stool in the rectum Some liquid passes around TX: Digital exam/extraction Intestinal obstruction Causes by strangulated hernia, tumor, ileus, stricture, volvulus (twisting of bowel) S/S: vomiting (bile, blood, feces), abd pain, constipation Complications: electrolyte imbalances, gangrene, perforation, shock, death TX: gastric decompression, IVF, surgery appendicitis Blind patch in the cecum Inflammation of opening of appendix-bacteria related s/s: pain especially at mcburney’s point (1/2 way b/w umbilicus and iliac crest), fever, n/v, elevated WBC Tx: NPO, cold pack peritonitis stomach contents enter Abd cavity Complications: fluid shift, abscesses, adhesions, septicemia, hyovolemic shock, ileus, organ failure S/S: abd distention, increased pulse and RR, n/v, fever, rigid abd, shock TX: NG for gastric decompression, IVF, antibiotics, pain meds, surgery IBS 2 types: Ulcerative colitis: Begins in rectum, expands to cecum Crohn’s: regional enteritis Affects all GI tract Most common= terminal ileum Causes: unknown S/S of IBS: constipation, diarrhea, bloody stools, abd cramping, wt loss S/S crohn’s: variable, n/v, pain, cramping, abd tenderness, fever, night sweats, malaise, joint pain Complications:hemorrhage, obstruction, perforation, abscess, fistulas, megacolon, colon cancer, joint inflammation, diarrhea, stones, liver dx, electrolyte imbalances Tx: meds (page 786), low roughage diet without milk, nicotine patches, surgery with possible removal of intestine Diverticulosis Small sac like pouches in intestinal wall Most in sigmoid colon Risk factors: lack of dietary factors, age, constipation, obesity, emotional tension S/S: asymptomatic, constipation, diarrhea, pain, rectal bleed, n/v, urinary problems Complications: bleed, obstruct, perforation, peritonitis, fistula Tx: high residue diet, no spicy foods, no seedy food, stool softener, meds, page 788, surgery Colorectal CA 3rd most common in women High fat low fiber diet is risk factor Most found in rectum or low sigmoid S/S: depend on location, cramping, anemia, weakness, fatigue, left sided= more obvious changes TX: surgery, colostomy, chemo, radiation Polyps Small benign growths that can become malignant Multiple polyps called gardner’s syndrome or familial polyposis S/S:asymptomatic Complications: bleed, obstruction Tx: removal, colectomy hemorrhoids Dilated veins in rectum May be internal or external Risk factors: increased pressure in rectal blood vessels from constipation, pregnancy, prolonged sit or stand S/S: pain, bleed, itching, TX : surgery, ice followed by heat, medication Anorectal abscess Infection in the tissue around rectum S/S: pain, swelling, redness, tenderness, diarrhea, bleeding, itching, discharge Tx: antibx, incision, drainage, surgery, ice packs, pt education r/t to cleansing Anal fissure Laceration b/w anus and perianal skin r/t constipation, diarrhea, crohn’s, TB, leukemia, trauma, childbirth S/S: pain with defecation, bleeding, itching, urinary frequency, urinary retention, dysuria Tx: heal spontaneously, sitz bath, stool softeners, pain meds, surgery Anal fistula Abnormal opening b/w anal canal and perianal skin Causes: abscess, IBD, TB S/S: pruritis, discharge Tx: sitz bath, surgery, temporary colostomy, pain meds Pilonidal cyst Painful and swollen May form abscess Surgery may be needed to fix PT EDUCATION Handwashing Proper food handling Food poisoning Stress management When to call doctor Page 793 THE END