PPT Prolapse
advertisement
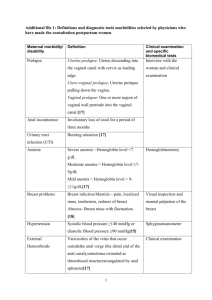
Utero-Vaginal Prolapse Background • The pelvis encloses organs that primarily function in storage, distension and evacuation. The pelvic viscera must maintain their normal anatomic relationships within this cavity so that these physiological functions can be sustained. Background The uterus is normally anteverted, anteflexed Version: is the angle between the longitudinal axis of cervix, and that of the vagina Flexion: is the angle between the longitudinal axis of the uterus, and that of the cervix Genital Prolapse • Genital prolapse is the descent of one or more of the genital organ (urethra, bladder, uterus, rectum or Pouch of Douglas or rectouterine pouch) through the fasciomuscular pelvic floor below their normal level • Vaginal prolapse can occur without uterine prolapse but the uterus cannot descend without carrying the vagina with it. Supports of the uterus • DeLancey in 1994 defined three levels of vaginal support, reviving the importance of the connective tissue structures and giving a working basis for the present day understanding of the anatomy and surgical treatment. Three level of Supports of Uterus • Level I: The cardinal uterosacral ligament complex • Level II: The pubo- cervical and recto-vaginal fascia • Level III: The pubo-urethral ligaments anteriorly & the perineal body posteriorly Anterior vaginal wall prolapse • Prolapse of the upper part of the anterior vaginal wall with the base of the bladder is called cystocele • Prolapse of the lower part of the anterior vaginal wall with the urethra is called urethrocele. • Complete anterior vaginal wall prolapse is called cysto-urethrocele. Anterior vaginal wall prolapse • Weakness in the – Supports of the bladder neck – Urethero vesical junction – Proximal urethra • Caused by – Weakness of pubocervical fascia and pubourethral ligaments Middle compartment defect • Enterocele and eversion of vagina • Enterocele (Herniation of POD) Posterior compartment defect • Rectocele • Perineal body descent Uterine descent • Utero-vaginal (the uterus descends first followed by the vagina): This usually occurs in cases of virginal and nulliparous prolapse due to congenital weakness of the cervical ligaments. • Vagino-uterine (the vagina descends first followed by the uterus):This usually occurs in cases of prolapse resulting from obstetric trauma. Degree of uterine descent • 1st degree: The cervix desends below its normal Ievel on straining but does not protrude from the vulva (The extemal os of the cervix is at the level of the ischial spines) • 2nd degree: The cervix reaches upto the vulva on straining • 3rd degree: The cervix protrudes from the vulva on straining • Procidentia- whole of the uterus is prolapsed outside the vulva and the vaginal wall becomes most completely inverted over it. Enterocele is usually present Vault prolapse • Descent of the vaginal vault, where the top of the vagina descends )or inversion of the vagina) after hysterectomy Pelvic organ prolapse quantitative (POPQ) exam • In 1996, by the ICS • POPQ system describes the location and severity of prolapse using segments of the vaginal wall and external genitalia, rather than the terms cystocele, rectocele, and enterocele Aetiology • Erect posture causes increased stress on muscles, nerves and connective tissue • Acute and chronic trauma of vaginal delivery • Aging • Estrogen deprivation • Intrinsic collagen abnormalities • Debilitation • Iatrogenic Precipitating factors ↑ intra abdominal pressure ↑ weight of the uterus Traction of the uterus by vaginal prolapse or by a large cervical polyp Obesity(40%--75%) Smoking Pulmonary disease (chronic coughing) Constipation (chronic straining) Recreational or occupational activities (frequent or heavy lifting) Symptoms of Prolapse • Pelvic floor disorders become symptomatic through either of two mechanisms: 1. Mechanical difficulties produced by the actual prolapse, 2. Bladder or bowel dysfunction, disrupting either storage or emptying. Clinical presentation • Before actual prolapse. the patient feels a sensation of weakness in the perineum. particularly towards the end of the day • Later the patient notices a mass which appears on straining. and disappears when she lies down • Urinary symptoms are common and trouble some even with slight prolapse: a) Urgency and frequency by day b) Stress incontinence c) Inability to micturate unless the anterior vaginal wall is pushed upwards by the patient's fingers d) Frequency when cystitis develops • Rectal symptoms are not so marked. The patient always feels heaviness in the rectum and a constant desire to defaecate. Piles develop from straining. • Backache, congestive dysmenorrhoea and menorrhagia are common. • Leucorrhoea is caused by the congestion and associated by chronic cervicitis. • Associated decubitus ulcer may result in discharge which may be purulent or blood stained Diagnostic approach • Beginning with a careful inspection of the vulva and vagina to identify erosions, ulcerations, or other lesions • The extent of prolapse should be systematically assessed • Suspicious lesions should be biopsied Examination • • • • • • • Local examination Per speculum examination Per vaginal/ Bimanual examination Bonney’s stress test Evaluation of tone of pelvic muscles Recto vaginal examination Position of patient for examination - standing & straining - dorsal lithotomy Diagnostic approach • The maximal extent of prolapse is demonstrated with a standing straining examination when the bladder is empty • Pelvic muscle function should be assessed after the bimanual examination → palpate the pelvic muscles a few centimeters inside the hymen, along pelvic sidewalls at the 4 & 8 o’clock • Resting tone & voluntary contraction of the anal sphincters should be assessed during rectovaginal examination Evaluation of pelvic floor tone • Place 1 or 2 fingers in the vagina and instruct the patient to contract her pelvic floor muscles (i.e., the levator ani muscles). Then gauge her ability to contract these muscles, as well as the strength, symmetry, and duration of the contraction. • The strength of the contraction can be subjectively graded with a modified Oxford scale (0 = no contraction, 1 = flicker, 2 = weak, 3 = moderate, 4 = good, 5 = strong). Bladder evaluation • For all patients with prolapse following information should be obtained – Screening for urinary tract infection – Postvoid residual urine volume – Presence or absence of bladder sensation • Bonney’s stress test performed following reduction of prolapse • If test positive incontinence surgery should be performed at the time of prolapse surgery Testing for Integrity of anal sphincter • Should be assessed for resting tone and voluntary squeeze and sensation around the vulva with the bulbo-cavernous reflex and crude sensory testing for evidence of pudendal neuropathy Prevention • During labour &puerperium – Avoid premature bearing down – Avoid long second stage – Repairs all tears &incisions accurately in layers – Use delayed absorbable suture – Do not express the uterus when attempting to deliver placenta – Encourage pelvic floor exercise – Avoid puerperal constipation-decreases bearing down Prevention • At hysterectomy – Vault suspension with uterosacral and cardinal ligaments – Obliteration of deep cul-de –sac by Moschowitz sutures – Sacropexy in high risk situations like collagen disorders – Increase acceptability of estrogen replacement therapy Treatment • Physiotherapy – Kegel’s pelvic floor exercise • Kegel’s perineometer • Influence only the voluntary muscles • No action to the fascial supporting system – Vaginal cones of increasing weight . Associated decubitus ulcer • To relieve congestion, the prolapse can be reposited in the vagina with the help of tompoons ar pessary and this helps in healing of the ulcer • Hygroscopic agents like acriflavin-glycerine can help reduce the congestion further Pessary • During pregnancy • Immediately after pregnancy, during lactation • When future childbearing is intended in near future • Refusal to operation by patient • As a therapeutic test • To promote healing in a decubital ulcer Pessary in situ Complications of pessary • • • • • • • Constipation Urinary incontinance B.vaginitis, ulceration of vaginal wall Cervicitis Carcinoma of vaginal wall Impaction of pessary Strangulation of prolapsed tissue Principles of Management • Physical examination must not be used in isolation to develop treatment strategy. • Any decision for surgical intervention should take account of how prolapse is affecting lifestyle. Aim of pelvic reconstructive surgery • To restore anatomy, maintain or restore visceral function, and maintain or restore normal sexual function Uterine descent- surgeries • Vaginal hysterectomy • Sling surgeries – Shirodkar – Khanna’s – Purandares • Fothergill’s surgery Vault prolapse • Separation of the rectovaginal fascia from pubocervical fascia. • In post hysterectomy patients it is important to reattach the rectovaginal fascia to the pubocervical fascia and to provide good support to the vaginal apex by reattaching the vaginal cuff to the uterosacral cardinal ligament complex. Surgery for prolapsed vaginal vault • Vaginal surgery – Decreased operative time – Decreased incidence of adhesion formation – Quicker recovery time • Abdominal surgery. – Failed previous vaginal approach – Have foreshortened vagina – Young patients with advanced prolapse – With other co existing conditions • Obliterative procedures Vaginal surgery • Mc Call culdoplasty – Internal – external • Sacrospinous ligament fixation • High uterosacral ligament suspension with fascial reconstruction • Iliococcygeus fascia suspension Abdominal repairs • Abdominal sacral colpopexy • High uterosacral ligament suspension • Laparoscopic approach Obliterative procedures • Le forte partial colpocleisis • Colpectomy and colpocleisis Diagnosis of Stress Incontinence with Pelvic Organ Prolapse • Loss of urine during coughing, sneezing, laughing or lifting something heavy • These activities cause an increase in "belly pressure” → forces the urine out of the bladder • Stress incontinence occurs almost exclusively in women & thought to be due to "pelvic (vaginal) relaxation" from childbirth or aging Treatment of Stress Incontinence with Pelvic Organ Prolapse • Conservative therapy - Pelvic floor exercises - Urinary meatel occlusion devices - Collagen injections • Urinary incontinence surgery - Ant repair & Kelly’s plication - Pubo-vaginal sling procedure - TVT sling procedure - Burch Urethropexy Thank you